Meniscus Injury...conservative or surgical management?
Meniscus injuries are common but what is the appropriate management? What clinical factors indicate conservative or surgical management pathways? The main clinical issue currently is the lack of research regarding the efficacy of arthroscopic meniscal repairs compared to a conservative approach (Englund, Roemer, Hayashi, Crema, & Guermazi, 2012). The long-term sequelae of these two approaches are still unknown, especially regarding development of knee osteoarthritis.
There is minimal literature regarding clinical prediction rules or protocols which indicate surgery rather than conservative management. There are multiple articles displaying the benefits of physiotherapy following meniscectomy, however only two articles exist (that I'm aware of) comparing surgical and conservative management following meniscal tears.
Herrlin and associates (2007) analysed a group of 90 individuals with degenerative medial meniscus tears, half receiving arthroscopy and supervised exercise program while the remaining individuals received only the exercise program. The exercise program consisted of twice-weekly sessions for eight weeks, consisting of stationary bicycle, calf and quadriceps strengthening, lunges, stairs, leg press, balance training and knee stretching, enhanced by a similar home exercise program. At eight weeks and six months follow-up both groups improved in VAS scores, knee function measures and satisfaction measures, with no significant difference between groups. This article is a landmark paper as it justifies an eight week targeted exercise program, compiled and delivered by a physiotherapist, is as effective as a surgical procedure (Herrlin et al., 2007). Using literature, we can validate our treatment is more cost-effective, time-effective and provides less risk for the patient.
Bulgarian Lunge...late stage single leg progression in meniscus rehabilitation.
A more recent study by Katz and colleagues (2013) randomly assigned 351 individuals, aged 45 years or older with meniscus tears and mild to moderate osteoarthritis evident on imaging, into a surgical group (who then received physiotherapy) and a physiotherapy group (with individuals able to receive surgery if indicated or chosen by the patient). The physiotherapy group consisted of a standardised program (addressing range of motion, muscle strength, aerobic capacity, proprioception and balance) where exercises were individually progressed as the patient's objective measures improved. The WOMAC Index was used as the primary outcome measure, assessed at baseline, 3, 6 and 12 months post-intervention. There was no significant difference between groups at 6 months, however 30% of individuals in the physiotherapy group underwent surgery within 6 months (Katz et al, 2013). Although this appears less enchanting than the Herrlin study, 70% of individuals had full return to function without requiring surgery. We are still able to justify the efficacy of physiotherapy as a valid alternative to surgical intervention, with only 30% requesting surgery.
A case report by Stensrud and colleagues (2012) provided a twelve week neuromuscular and strengthening program, progressing to single leg exercises, which also produced these positive results, however the physiotherapy group was compared to control rather than an arthroscopy group.
We must remember that Herrlin’s study looked only at degenerative meniscal tears, with traumatic injuries being excluded. Katz's study does not dictate whether the tears were traumatic or degenerative, so extrapolation to treating traumatic meniscus tears is difficult. With traumatic tears, the severity ranges from mild pain to severe pain and locking or restricted knee range. Brukner & Khan (2012) state a locked knee requires immediate arthroscopy. However, the majority of patients present with moderate pain and mechanical symptoms, with some catching rather than true locking. The management for these patients must be made considering the patient’s signs and symptoms, work and sporting demands, timeframes, financial status and MRI findings.
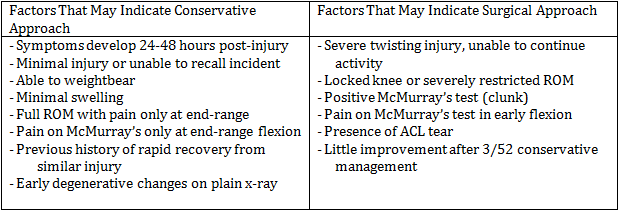
Patients who appear to respond best to arthroscopy present with increasing pain, some locking and/or catching and have a displaced meniscus tear on MRI (Suter et al., 2009). Brukner & Khan (2012) provide an amazing table (Table 1.1) which gives a rough outline of patients who may respond favourably to arthroscopic management. Certain therapists are more conservative in their approach and will try three to six weeks of conservative management, monitoring symptoms. If no improvements occur they will be referred for a surgical consultation. This greatly depends on sporting and work timelines, if a deadline is looming and surgery can return a player to function faster, surgery may be indicated. However, with greater knowledge of bone oedema and osteoarthritis secondary to trauma, therapists are trending towards a more conservative approach.
Table 1.1 Clinical Factors which may indicate a surgical or conservative approach, Brukner & Khan, 2012 pg 636.
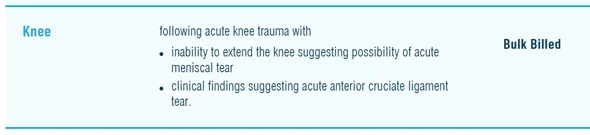
With regards to MRI, current Medicare guidelines (Australia only) stipulate a patient with suspected meniscus tear can be bulk-billed for an MRI when referred by a General Practitioner (GP).
The clinical history/findings on the referral must include:
- an acute traumatic injury
- inability to extend knee
- positive findings on meniscus testing/ACL testing
The current cost of MRI in Victoria is $295, completely covered by Medicare. In Western Australia, scans cost $520 with the rebate of $295 being covered (so an out-of-pocket expense still exists). If I suspect a moderate to severe meniscus tear, I automatically refer back to the GP politely suggesting/requesting an MRI scan.
Some literature exists regarding MRI ability to predict repairability of tears (can a surgeon determine pre-surgery, based on MRI, if a repair or meniscectomy will be performed?), however this doesn’t provide a patient prognosis, only the type of surgery performed (Nourissat et al., 2008; Shiozaki et al., 2002).
The patient with a meniscus tear can be managed conservatively or surgically.
- degenerative meniscus tears should be managed conservatively, with an exercise program targeting joint mobility, lower limb kinetic chain strengthening, balance training and stretching
- a traumatic meniscus tear with locking should be managed surgically
- a traumatic tear with increasing pain, some locking and displaced tear on MRI would respond well with surgery
- all other traumatic tears, the decision should be based on clinical reasoning, but trending towards a conservative approach
Alicia
References:
Brukner, P., & Khan, K. (2012). Brukner & Khan's clinical sports medicine (4th ed.). Sydney ; New York: McGraw-Hill.
Englund, M., Roemer, F. W., Hayashi, D., Crema, M. D., & Guermazi, A. (2012). Meniscus pathology, osteoarthritis and the treatment controversy. [; Research Support, Non-U.S. Gov't; Review]. Nature reviews. Rheumatology, 8(7), 412-419.
Herrlin, S., Hallander, M., Wange, P., Weidenhielm, L., & Werner, S. (2007). Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 15(4), 393-401.
Nourissat, G., Beaufils, P., Charrois, O., Selmi, T. A. S., Thoreux, P., Moyen, B., . . . French Society of, A. (2008). Magnetic resonance imaging as a tool to predict reparability of longitudinal full-thickness meniscus lesions. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 16(5), 482-486.
Shiozaki, Y., Horibe, S., Mitsuoka, T., Nakamura, N., Toritsuka, Y., & Shino, K. (2002). Prediction of reparability of isolated semilunar lateral meniscus tears by magnetic resonance imaging. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 10(4), 213-217.
Stensrud, S., Roos, E. M., & Risberg, M. A. (2012). A 12-week exercise therapy program in middle-aged patients with degenerative meniscus tears: a case series with 1-year follow-up. The Journal of orthopaedic and sports physical therapy, 42(11), 919-931.
Suter, L. G., Fraenkel, L., Losina, E., Katz, J. N., Gomoll, A. H., & Paltiel, A. D. (2009). Medical decision making in patients with knee pain, meniscal tear, and osteoarthritis. Arthritis and rheumatism, 61(11), 1531-1538.