Cervicogenic Headache
Introduction
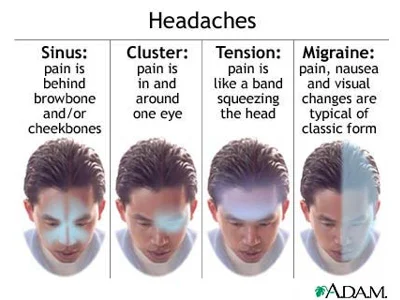
Headaches are a common presenting complaint in the private setting. There are many types of headaches we need to be able to differentiate between, with some common examples being migraine-without-aura, migraine-with-aura, cluster headache, tension-type headache (TTH), chronic paroxysmal headaches, and the one we like to treat, cervicogenic headaches. It is important we know how to recognise the symptoms/signs which are typical to each headache type and in particular the diagnostic criteria of CGH. This is not to say that patients with other types of headache can't find benefit from physiotherapy treatments, but the benefit is not based on the premise that we are improving the primary driving musculoskeletal impairment in the cervical spine.
Research has shown up to 70% of headache sufferers report neck pain, with only 18% of these people having CGH, reflecting the bidirectional nature of the TCN (Nilsson, 1995). Due to the bi-directional interactions between the TCN and cervical afferents, neck pain and hypersensitivity is not an unique feature of CGH and can be present in migraine and TTH (Jull, et al., 2007; Jull, et al., 2009).
Unlike migraine and tension-type headache (TTH), which are defined as primary headaches, CGH is as a secondary headache and currently understood to originate from a musculoskeletal dysfunction of the upper cervical spine (Sjaastad & Bakketeig, 2008; Sjaastad, Fredriksen, & Pfaffenrath, 1998; Sjaastad, Saunte, Hovdahl, Breivik, & Gronbaek, 1983). Currently three musculoskeletal impairments have been validated as clinical features of CGH, which are not present in migraine and TTH (Jull, Amiri, Bullock‐Saxton, Darnell, & Lander, 2007; King, Lau, Lees, & Bogduk, 2007; Zito, et al., 2006):
A painful upper cervical joint,
Loss of range of movement, and
Impairment in the muscular system of the cervical spine.
With time our understanding of the pathophysiology and presentation of CGH has changed. The mechanism of the headache is now thought to originate from convergence of primary afferent neurones of the upper three cervical nerves onto the trigeminocervical nucleus (TCN), therefore allowing the neck to refer pain into regions of the head.
HISTORY
It was in the early 1980's that authors reported a type of unilateral headache provoked by neck movements, which was categorised as Paroxysmal Hemicrania, although therapists were perplexed by the uncharacteristic mechanical nature of these headaches (Sjaastad, et al., 1983). As such, a new category of headaches was developed, and in 1988 Sjaastad and colleagues provided a definition for cervicogenic headache as a secondary headache, which is currently accepted by the The International Headache Society (Olesen & Steiner, 2004). At this time there were two cardinal signs of CGH, which to this day remain vital features in differential diagnosis. These are the presence of a unilateral headache and the provocation of headache with neck movements. The current definition (if you'd like to read further) is presented in Jull, Sterling, Falla, Treleaven, and O'Leary (2009, p. 119).
At the time that significant research regarding the diagnosis of CGH began (in the early 1980’s), the gold standard for diagnosis remained the use of diagnostic blockade (Amiri, et al., 2007; Bogduk & Govind, 2009; King, et al., 2007; Sjaastad, et al., 1983). However, this is often not accessible to all headache patients with possible CGH presentation. Instead we rely on our musculoskeletal examination.
One important and often under described component of this examination is the manual palpation of the upper cervical spine. Jull, Bogduk, & Marsland published a landmark paper in 1988 stating that an experienced musculoskeletal physiotherapist has the same accuracy in detecting a symptomatic joint with manual examination compared with radiologically controlled diagnostic nerve block. However, manual palpation is a trained skill, which clinicians used to describe/detect changes in feeling when applying pressure to an area of the human body.
Many authors have since debated that manual palpation has 100% specificity and sensitivity and the premise for this debate is based on the following questions (Bogduk & Govind, 2009, King et al, 2007):
Can manipulative therapists actually feel movement in specific vertebral joints?
Are the allegedly palpable abnormalities at all diagnostic, or are they non-specific signs?
Is it possible for manipulative therapists to accurately diagnose vertebral disorders by manual examination?
In regards to the clinical presentation, there is moderate agreement that considerable overlap exists between the symptoms of CGH, migraine and TTH, and that no particular symptom is specific to each headache type (Antonaci & Sjaastad, 2011; Biondi, 2005; Jull, et al., 2009). Therefore, we rely more heavily on the physical examination to confirm our suspicion of the cervical spine as a primary driver of the headache.
For CGH in particular we must perform an examination which identifies a loss of range of movement (in AROM testing or with the flexion/rotation test), deficits in muscular activation/endurance/coordination (using the craniocervical flexion test and pressure biofeedback unit), and a comparable joint sign confirmed with manual palpation (hopefully with reproduction of the headache).
Manual examination
Maitland and Hengeveld (2005) describe manual palpation as an objective way to measure the range and quality of movement at a spinal segment. Accuracy and sensitivity of palpation relies on the therapist’ ability to describe the end-feel of a joint, the quality of resistance through movement and the reproduction of pain.
Criticism of the research conducted by Jull and colleagues (1997), is that no standardized assessment procedure was used. Therapists conducted their manual palpation in the same manner they would do so in clinical practice. Although the results of this study showed excellent agreement among therapists in their ability to detect a symptomatic level, the study design and power of results were questioned.
King, et al. (2007) have been the first authors to successfully repeat the study design done by Jull in 1988, i.e. to evaluate the validity of manual palpation in the diagnosis of zygopophysial joint dysfunction. This study was eight times larger and of much superior methodology to the early study. The results indicated that sensitivity was 89% and specificity 47%, with an overall likelihood ratio at 1.7. One of the major strengths of this research is that “the values are probably more realistic, because they were based on larger sample sizes, and they do not imply infallibility, which a value of 1.00 does” (King, et al., 2007, p. 25).
In regards to specificity, the authors have failed to provide information about the method of manual palpation and thus both of these cornerstone articles have left readers without guidance about the ideal procedure for performing passive accessory intervertebral movements (PAIVMS). Throughout the literature musculoskeletal physiotherapists with 20 years of experience or more are utilised as the examiners in the trial. Maybe this reflects the true nature of physiotherapy practice? However, it begs the question whether the results could even be generalised to less experienced physiotherapists who may not have developed the same skill in their handling?
Palpation of the upper cervical spine
“The anatomy of the high cervical spine is unique and, to some degree, more complicated to assess than the rest of the vertebral column. The shape of the bones and their articulations are distinctly different between the occiput and atlas, atlas and axis, and axis and C3. Such a marked change in anatomy does not occur in such close proximity anywhere else in the vertebral column” (Edwards, 1992, pp. 42-43). As such, careful consideration must be made when understanding which level is being loaded under pressure, and what sensitising movements can be applied to differentiate between intra-articular and periarticular restrictions to movement.
Edwards (1992) and Maitland (2005) recommend that palpation of the upper cervical spine should be used to CONFIRM the findings of the active range of movement and passive physiological range of movement assessment. They also suggests that palpation should be combined with movements to enhance structural differentiation.
If you're not sure about what structures you are palpating or loading then get the skeleton out and have a look at what happens when pressure is applied to each level in various positions....
These are the principles I follow with my manual examination:
- In right rotation and slight flexion there will be a general 'opening' on the left side of the cervical spine.
- If you apply a posterior-anterior (PA) pressure on left C1, you will notice an increased stretch at C1/2 joint and periarticular structures.
- If you apply a PA pressure on left C2, you will notice how it decreases stretch at C1/2 joint but increases the stretch at C2/3.
- Therefore, if you are applying a PA to the left C2 in neutral and there is pain, rotation to the right with increased symptoms implicates C2/3, but if you rotate to the left and the symptoms increase, it suggests C1/2.
- If we go through a different posture.... In left rotation and extension
- PA pressure on left C2 increases stretch at the C1/2 joint.
- PA pressure on left C1 decreases rotation at the C1/2 joint.
- Adding upper cervical flexion often biases/loads O/C1.
- If you start with your fingers on the occiput and slip down onto C1 articular pillar and the direct pressure cephalad and medial, you'll find O/C1.
It is important to remember that many authors insist the diagnosis of a symptomatic level should be made based on the clinical theory proposed by Maitland of joint mobility taught through the construct of a movement diagram - discussed in a previous blog (Jull, Treleaven, & Versace, 1994; Zito, et al., 2006).
Maitland describes that thickness in the capsules and surrounding tissues can indicate chronicity of the soft-tissue changes. These changes need to be related back to the history and chronicity of the patient’s symptoms and related to the pain provocation and pain referral created by the palpation of that area. Maitland (2005) encourages the therapist to compare findings between left and right and adjacent levels to gain an understanding of the significance of the movement abnormality.
Conclusion
To this day there has been little research conducted specifically in the field of CGH. Much of the research existing from the study of neck pain and headaches should be applied thoughtfully to this definitive subgroup of headaches. Current literature provides evidence that assessment of the cervical spine for the three main musculoskeletal impairments (identified above) is a good base for diagnosing CGH (Jull, et al., 2009). Of the three main musculoskeletal impairments indicative of CGH, manual examination is the least standardized.
However, therapists such as Maitland provide us with examination procedures to help improve the consistency, reliability and validity of our manual palpation.It may not be as good as diagnostic blockade, but in current physiotherapy practice, our ability to detect a symptomatic upper cervical joint is fairly reliable and should be used in conjunction with other physical tests to reproduce (confirm) and reduce (treat) patients with CGH.
Sian
References
Amiri, M., Jull, G., Bullock-‐Saxton, J., Darnell, R., & Lander, C. (2007). Cervical musculoskeletal impairment in frequent intermittent headache. Part 2: Subjects with concurrent headache types. Cephalalgia, 27(8), 891-898.
Antonaci, F., & Sjaastad, O. (2011). Cervicogenic Headache: A Real Headache. Current neurology and neuroscience reports, 11(2), 149-155.
Biondi, D. M. (2005). Cervicogenic headache: a review of diagnostic and treatment strategies. JAOA: Journal of the American Osteopathic Association, 105(4 suppl), 16S-22S.
Bogduk, N., & Govind, J. (2009). Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. The Lancet Neurology, 8(10), 959-968.
Edwards, B. C. (1992). Manual of combined movements: their use in the examination and treatment of mechanical vertebral column disorders: Churchill Livingstone.
Jull, G., Amiri, M., Bullock-‐Saxton, J., Darnell, R., & Lander, C. (2007). Cervical musculoskeletal impairment in frequent intermittent headache. Part 1: Subjects with single headaches. Cephalalgia, 27(7), 793-802.
Jull, G., Bogduk, N., & Marsland, A. (1988). The accuracy of manual diagnosis for cervical zygapophysial joint pain syndromes. Med J Aust, 148(5), 233-236.
Jull, G., Sterling, M., Falla, F., Treleaven, J., & O'Leary, S. (2009). Whiplash, headache and neck pain. Edinburgh: Elsevier Churchill-Livingstone.
Jull, G., Treleaven, J., & Versace, G. (1994). Manual examination of spinal joints: Is pain provocation a major diagnostic cue for dysfunction. Australian journal of physiotherapy, 40, 159-‐163.
Jull, G., Zito, G., Trott, P., Potter, H., & Shirley, D. (1997). Inter-‐examiner reliability to detect painful upper cervical joint dysfunction. Australian journal of physiotherapy, 43(2), 125-129.
King, W., Lau, P., Lees, R., & Bogduk, N. (2007). The validity of manual examination in assessing patients with neck pain. The Spine Journal, 7(1), 22-26.
Maitland, G. D., & Hengeveld, E. (2005). Maitland's vertebral manipulation. Edinburg: Elsevier Butterworth-Heinemann.
Nilsson, N. (1995). The prevalence of cervicogenic headache in a random population sample of 20-‐59 year olds. Spine (Philadelphia, Pa. 1976), 20(17), 1884-1888.
Olesen, J., & Steiner, T. J. (2004). The international classification of headache disorders, 2nd edn (ICDH-II). Journal of neurology, neurosurgery and psychiatry, 75(6), 808-811.
Selvaratnam, P., Niere, K. R., & Zuluaga, M. (2009). Headache, Orofacial Pain and Bruxism. Chicago
Sjaastad, O., & Bakketeig, L. S. (2008). Prevalence of cervicogenic headache: Vågå study of headache epidemiology. Acta Neurologica Scandinavica, 117(3), 173-180.
Sjaastad, O., Fredriksen, T. A., & Pfaffenrath, V. (1998). Cervicogenic Headache: Diagnostic Criteria. Headache, 38(6), 442-445.
Sjaastad, O., Saunte, C., Hovdahl, H., Breivik, H., & Gronbaek, E. (1983). "Cervicogenic" Headache. An Hypothesis. Cephalalgia, 3(4), 249-256.
Zito, G., Jull, G., & Story, I. (2006). Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Manual therapy, 11(2), 118-129.