Stronger bones with Osteoporosis
introduction
In 2024 I listened to a podcast titled “Building Stronger Bones” on the Physio Network podcast, hosted by ex-Physica college Sarah Yule. Curios to learn more about the research being discussed, specially the LIFTMOR trial, I turned to college and APA-titled Musculoskeletal Physiotherapist Tonya Jones, who, after many months of diving deep into research on Osteoporosis, has helped to develop the Stronger Bones clinic at Physica. It gives me great pleasure to welcome Tonya to this blog, to share with us the latest research in osteoporosis guiding her clinical practice.
The purpose of the blog is to revise our knowledge of the Osteoporosis disease process, current diagnostic tests and recent changes to our understanding of how progressive strength training should be an integral part of patient long term management. It is exciting and inspiring to hear how physiotherapists are paving the way forward in helping patients build stronger bones and combat risk factors in falls prevention and fractures risk reduction.
Understanding Osteoporosis
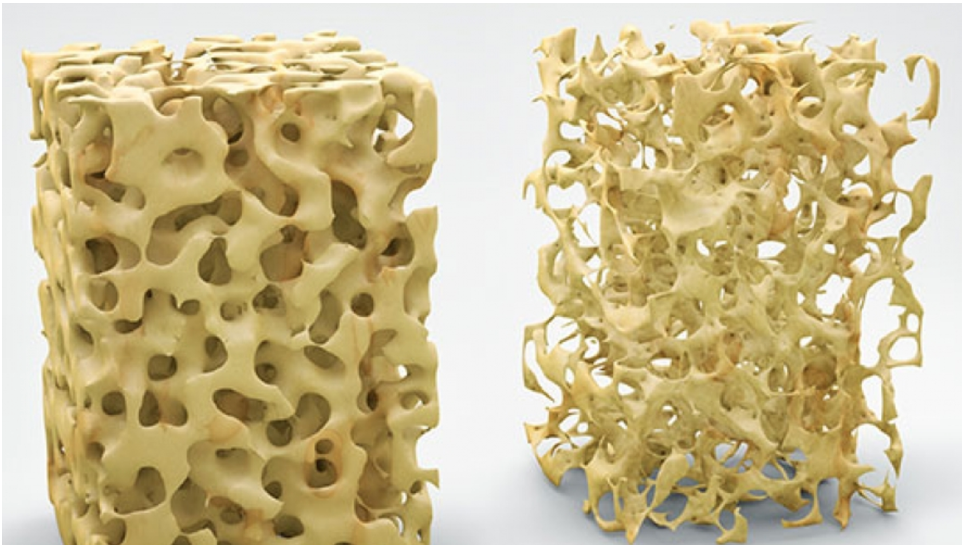
Osteoporosis (OP) is a systemic skeletal disorder characterized by decreased bone mass and the deterioration of the micro-architecture of bone tissue. This deterioration results in a honeycomb-like appearance under microscopic examination, where the structural integrity of bone is compromised due to the thinning and loss of bony struts. As the micro-architecture degrades, bones become increasingly susceptible to fractures, leading to significant clinical implications (International Osteoporosis Foundation [IOF], 2024).
Prevalence
The prevalence of OP has escalated dramatically in recent decades, becoming the most common bone disease globally. Historical data indicates that while OP has existed for millennia, it was not recognized as a significant health concern until approximately 250 years ago (Mays, 1999). The aging population, particularly those over 50, is predominantly affected, largely due to increased life expectancy attributed to advancements in healthcare and lifestyle changes. By 2024, one in three women and one in five men over the age of 50 are diagnosed with OP, highlighting a pressing public health challenge (Stride et al., 2013).
The transition from active lifestyles to sedentary behaviour, influenced by technological advancements and labour-saving devices, has further exacerbated this issue. As society shifts towards less physically demanding activities, the opportunities for engaging in bone-loading exercises have diminished. Consequently, the need for effective intervention strategies has become critical.
Impact
OP is considered a silent disease as there are no symptoms. Instead, diagnosis often occurs after someone suffers a bone fracture especially if the fracture occurred in an event that would not normally be expected to cause injury like a minor stumble or fall (Lorentzon and Cummings, 2015). While fractures aren’t rare and can occur in the young, fractures in the elderly can have serious ramifications. Hip fractures cause hospitalization in almost all cases, and more than half will not regain their previous levels of mobility (IOF, 2024). Alarmingly, statistics also show that one in five people who fracture their hip will not survive the first twelve months. Other fractures such as the wrist which may not impact life as dramatically can still significantly and negatively impact the quality of life with 50% of sufferers reporting a loss in function more than six months later. The impact on the individual, their families, the community and the healthcare system is significant. In 2022, six million people over fifty in Australia were living with OP or Osteopenia (the pre-curser to OP). In the same year there were 108,103 fractures as a result of the disease costing healthcare AUD$3.84 billion (Osteoporosis Australia, 2022). In women over fifty, fractures due to OP resulted in more days in hospital than T2DM, heart attack and breast cancer combined.
Measurement and diagnosis
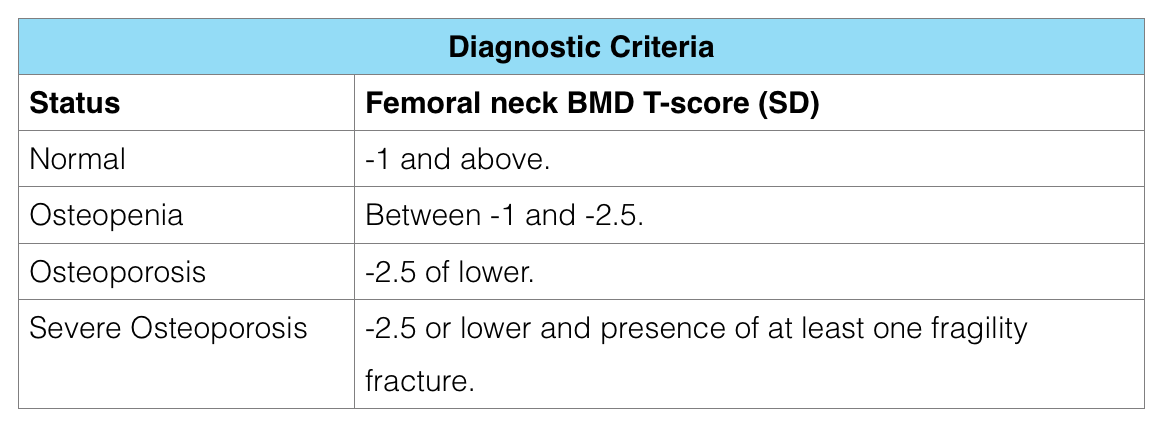
OP is usually quantified by measuring our bone mineral density (BMD) using dual-energy X-ray absorptiometry (DEXA). Though BMD is only one component of bone strength, it is a good enough proxy to be the current gold standard recommended by the World Health Organisation (2003). A DEXA scan gives our BMD a T-score. A T-score of more than -1.0 is considered normal BMD. A T-score between -1.0 and -2.5 is considered to be osteopenic and a T-score lower than -2.5 is considered osteoporotic.
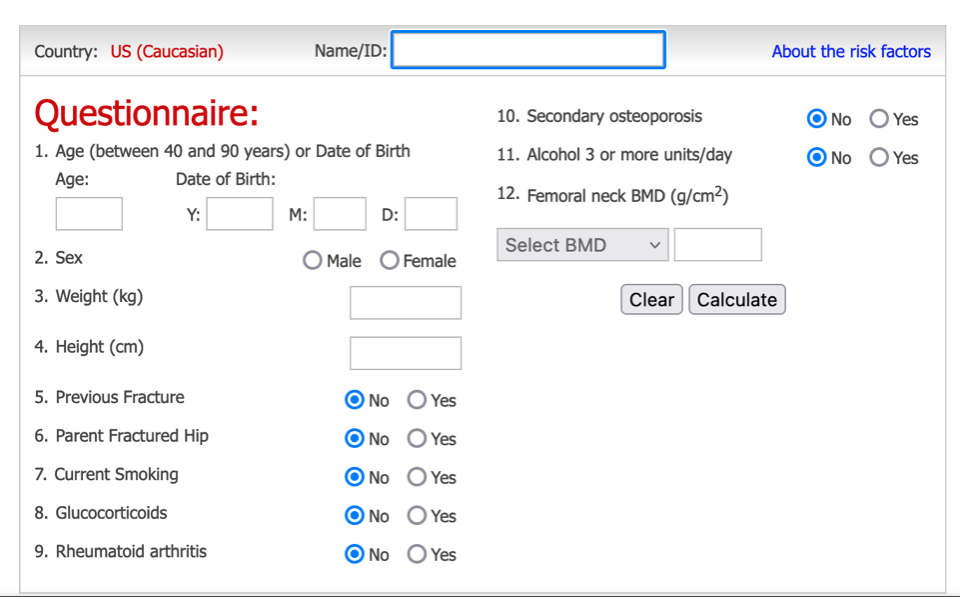
Another useful assessment tool is the Fracture Risk Assessment Tool or FRAX tool. Developed by the University of Sheffield in 2008, this free, easy-to-use questionnaire determines a person’s 10-year risk of hip and major osteoporotic fracture. The risk factors considered are; age, sex, weight, height, previous fractures, parental hip fractures, smoking status, alcohol intake, corticosteroid use, concurrent Rheumatoid Arthritis, risk for secondary OP from other diseases such as hyper-parathyroid or thyroidism, multiple myeloma’s, Cushing and celiac disease and the bone mineral density score (from the DEXA scan). A FRAX score above 20 indicates a high risk of a major osteoporotic fracture within the next 10 years and would alert the doctor to consider pharmacological or other management options.
Modifiable risk factors
Engaging in regular physical activity is equally critical, as recent research has demonstrated that certain types of exercise can prevent bone loss and may even increase BMD at the spine and hip. The latest guidelines from the Royal Australian College of General Practitioners emphasize exercise as a key intervention for managing OP (2024).
There are several other modifiable factors that can positively influence bone density and overall health. Historically, estrogen therapy was the primary treatment for OP in post-menopausal women, known for its ability to slow bone resorption and enhance calcium absorption (IOF, 2024). However, a comprehensive approach now encompasses various pharmacological options and lifestyle modifications.
A balanced diet rich in calcium and vitamin D is vital for optimal bone health. Other modifiable risk factors to be considered is reducing caffeinated drinks to <4 per day, decrease smoking, decrease BMI, increase protein intake and to reduce falls risk through improved balance and environment management (lighting, reducing clutter, removing rugs etc).
liftmor trial
Osteogenic exercise prescription is the new frontier in management of OP with some exercise types being better for improving all aspects of bone strength. The LIFTMOR trial has provided compelling evidence regarding the benefits of progressive resistance training (PRT) and impact weight-bearing exercises (IE) for individuals with osteoporosis. This trial demonstrated that structured PRT and IE not only improves muscle strength but also leads to increased bone mineral density in key areas such as the spine and hip.
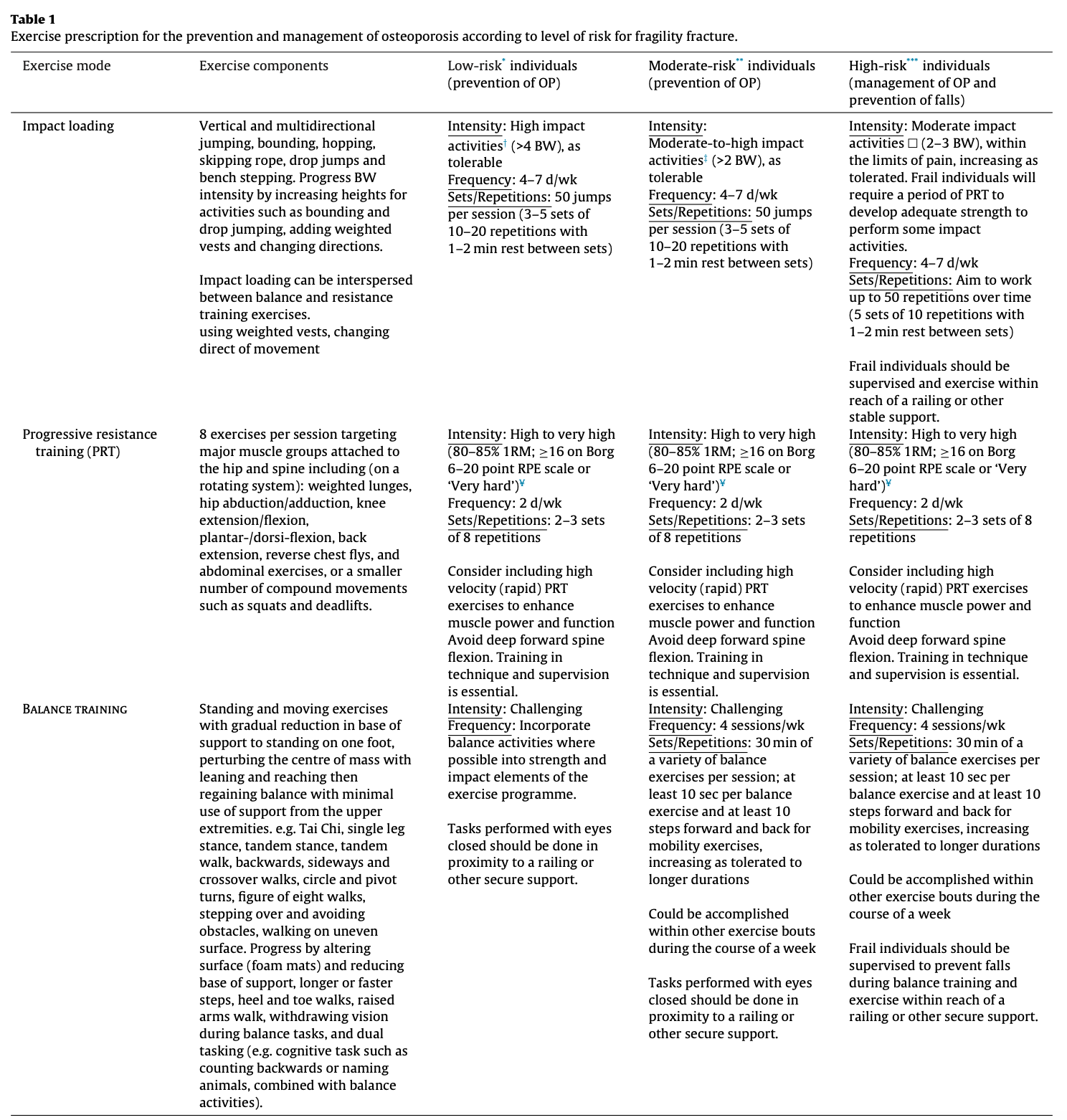
Participants engaged in PRT and IE experienced a significant reduction in the risk of falls and related fractures due to both the gain in muscle mass and increases in bone density highlighting the trial's endorsement of incorporating resistance and impact exercises into standard care for OP management. The following table highlights the different exercise recommendations for individuals who are determined to be low-risk, moderate-risk or high-risk for fragility fracture.
(Beck et al., 2017, p. 441)
The work of Professor Belinda Beck in her LIFTMOR trial conducted at Griffith University, QLD along with other reputable sources globally and within Australia (such as the International Osteoporosis Foundation (IOF). exercise guidelines from Exercise and Sport Science Australia (ESSA), Healthy Bones Australia (healthybonesaustralia.org.au), Osteoporosis Australia (osteoporosis.org.au) and Know Your Bones (knowyourbones.org.au) collectively state that PRT should involve resistance training performed in standing positions using weights, ideally comprising 6-8 exercises targeting the hips and spine, conducted at least three times per week. The weight used should be adjusted to individual capabilities, with higher loads yielding greater benefits. Impact exercises, which impose greater mechanical load on joints, are also beneficial. Individuals should aim for 10-50 impact steps on each leg several days a week, easily integrated into regular walking routines. It is crucial to maintain variety in exercise programs to stimulate ongoing bone remodelling, with modifications implemented every 3-6 months (Royal Osteoporotic Society, 2022). While balance training is not directly linked to bone preservation, it is recommended as a preventive measure against falls.
developing the ‘stronger bones’ class
In late 2023, my colleague Grant Freckleton asked me if I would be interested in running a new Physica programin 2024 for people with Osteoporosis (OP). I was very excited to be asked as I had a personal interest as a mature-aged therapist. Over the 2023 Christmas holidays I read as much research as I could find on the topic and returned in January with many additional suggestions to develop our course further. Combining our collaborative efforts in January 2024, the Stronger Bones Program (SBP) was launched.
The SBP incorporates the latest evidence on exercise prescription for OP from the sources above. The goal of the SBP is to preserve and increase bone strength, as well as address modifiable risk factors. It is unique in that it is a twice weekly, 6 -week supervised exercise, education and empowerment program. The aims of the SBP are to educate each participant about OP and the role diet, exercise and lifestyle play in the management of the condition. It also aims to safely introduce and progress participants through the three types of exercise required for bone growth and falls prevention (namely progressive resistance training, impact exercises and balance challenges). Finally, the SBP aims to empower participants with the tools and information needed to continue to progress their program beyond the 6 weeks independently whether opting to continue their exercises at home, in a gym or integrated into a local class.
Once the SBP physiotherapist has completed the assessment they can then match that person’s capabilities, functional capacity and bone density status with the safest and strongest progressive resistance training, impact exercises and balance challenges program possible to ensure there is the greatest chance of muscle and bone growth as reduced risk from falls.
conclusion
Physiotherapists play a vital role in the management of osteoporosis through individualized assessments and tailored exercise prescriptions. By developing comprehensive exercise programs that incorporate PRT, impact activities, and balance training, physiotherapists can enhance patients' bone health and overall quality of life.
biography
Tonya is an Australian musculoskeletal physiotherapist working in private practice at Physica Spinal and Physiotherapy Clinic, Ringwood, Melbourne. In 2022, In the same year, Tonya graduated with a Masters in Musculoskeletal Physiotherapy from La Trobe University having completed her undergraduate degree at Monash University in 2014. Prior to becoming a physiotherapist Tonya studied ballet and contemporary dance completing her first degree at the University of Kent in Canterbury and London Contemporary Dance School. She then ran her own Pilates and Personal Training gym in the UK for 6 years. Tonya has had a lifelong passion for human movement and exercise prescription which she has enjoyed further developing in the area of Osteoporosis with the launch of the Stronger Bones Program. Outside of her clinical practice work at Physica, Tonya tutors on spinal courses for the Australian Physiotherapy Association (APA). In 2023, she assisted in writing and delivering a new spinal course for the APA which was run both in Victoria and interstate.
References
Al-Azzawi, F. (2013). Hormonal changes and osteoporosis in women. Menopause International, 19(2), 77-82. https://doi.org/10.1177/1754045313499081
Beck, B.R., Daly, R. M., Singh, M. A., Taaffe, D. R. (2017). Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. Journal of Science and Medicine in Sport. 20(5):438-445.
Bonaiuti ,D., Shea, B., Iovine, R., Negrini, S., Robinson, V., Kemper, H. C., Wells, G., Tugwell, P., Cranney, A. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Systematic Reviews. 2002;(3):CD000333.
International Osteoporosis Foundation (IOF). (2024). Osteoporosis: A silent disease. https://www.iofbonehealth.org
Lorentzon, M., & Cummings, S. R. (2015). Osteoporosis: A global perspective. Nature Reviews Disease Primers, 1, 15001. https://doi.org/10.1038/nrdp.2015.1
Mays, S. A. (1999). The evolution of osteoporosis: A historical perspective. American Journal of Physical Anthropology, 38, 163-174. https://doi.org/10.1002/(SICI)1096-8644(199908)38:2<163::AID-AJPA8>3.0.CO;2-3
Osteoporosis Australia. (2022). The burden of osteoporosis in Australia. https://www.osteoporosis.org.au
Royal Australian College of General Practitioners. (2024). Guideline for the management of osteoporosis. https://www.racgp.org.au
Royal Osteoporotic Society. (2022). Osteoporosis and fractures. https://theros.org.uk
Stride, M., et al. (2013). Changes in physical activity and the risk of osteoporotic fractures. Journal of Bone and Mineral Research, 28(8), 1682-1690. https://doi.org/10.1002/jbmr.1957
Watson, S. L., Weeks, B. K., Wei,s L.J., Harding, A.T., Horan, S.A., Beck, B.R. (2018). High-Intensity Resistance and Impact Training Improves Bone Mineral Density and Physical Function in Postmenopausal Women With Osteopenia and Osteoporosis: The LIFTMOR Randomized Controlled Trial. Journal of Bone and Mineral Research. 33(2):211-220.
World Health Organization (WHO). (2003). Prevention and management of osteoporosis: A WHO scientific group report. https://www.who.int
University of Sheffield. (2008). FRAX: Fracture risk assessment tool. https://www.sheffield.ac.uk/FRAX