Taking the Sore Thumbs Out of Manual Therapy
I chose this title because it was the same of the presentation that I attended in September 2015 where I first met Dr. Chris DaPrato, know by most as DP. I was at a conference and actually had no intention of attending the seminar after seeing the slides for the presentation and thinking it was a luring and misleading title. Having come out of my Maitland-based Masters program heavily focussed on the specificity and skill of manual therapy from the perspective of joint mobilisation, I was horrified to find out the seminar was in fact about myofascial decompression.
So horrified in fact and defensive about my version of manual therapy, that when I was introduced to DP at the conference, without any hesitation, I gave him a piece of my mind and my opinion on why I wouldn’t be coming to his seminar. Mainly because I thought that teaching cupping (which is how I viewed it at that time) was never actually going to address the issue that many Physiotherapists are currently graduating with average handling and palpation skills. DP being who he is, always full of positivity and enthusiasm, laughed at me, applaud me for my blunt honesty and passion for being a therapist, cut me slack for having an accent, and convinced me to come and listen. So I did. This was the first lecture that opened my eyes to the vast differences between joint mobilisation (which I call manual therapy) and myofascial decompression (which he calls manual therapy).
Since that time I have had the great pleasure watching DP teach and helping on his labs with DPT students at UCSF. He is a wonderful and passionate teacher. Always willing to answer my unusual questions and teaching students about manual therapy and sports science. I’m grateful for the opportunities DP has given me to continue teaching and doing what I love while navigating the re-qualification process.
This past weekend I took the myofascial decompression level 1 course and proudly now own my own kits of cups. I would say there are two reasons it took me this long to attend a live class. The first is that there was no use until I was practicing again. The second is that I really don’t like the sensation. Similarly to when I did my training in dry needling, I really didn’t enjoy the sensation of the needles, or needling my whole body for the sake of practice. My nervous system just doesn’t like it. I don’t enjoy the feeling, I can’t relax or feel comfortable and my palms start to sweat. Well, with MFD, the impact it has on my body is the same. As soon as the cups are applied I am clinging on for the moment they are removed and feel like I can’t control my body. Of all the treatment modalities we have available that make me feel relaxed and comfortable, this makes me panic. So I finally plucked up the courage to go, because I know very well that others will benefit from me using this technique and that interjecting my personal experiences into the offering of treatment to others is fraught with danger.
I really enjoyed the didactic component of this course and the remainder of this blog shares some interesting concepts that you will learn about if you too choose to take a course through www.myofascialdecompression.com
Myofascial DECOMPRESSION therapy
MFD is the pairing of manual therapy with neuromuscular rehabilitation
Myofascial decompression is not cupping.
It is not cupping because of the treatment time (2-5 minutes for MFD), because it is active, because it involves movements, because there are no blisters, and because it is coupled with neuromuscular rehabilitation. For example, learning how to decompress the posterior shoulder for patients postoperatively or for athletes with end range impingement, is often coupled with motor control and movement retraining to promote optimal scapulohumeral rhythm. One of the interesting components of myofascial decompression therapy (MFD) is that for the short time the treatment occurs, the changes in range of motion and subjective ratings of range are immediate. This is a motivating factor for using this treatment on patients who are struggling to make gains in motion with other treatment modalities.
There is no current evidence to say it is performance enhancing, despite the fact that many athletes find benefit from this treatment, and for that, there is often a lot of negative press. Instead of focussing on this fact, the course allowed me to appreciate that out of all our manual therapy and instrument assisted soft tissue manipulation techniques, it is the only one that is a negative pressure approach or decompressive approach. To that end, we are still trying to understand the neurophysiological and biomechanical effects of compressive versus decompressive therapy.
It is used across many cultures and has been used in Chinese medicine for centuries and centuries. Another difference between cupping and myofascial decompression is that the former is often used to treat a multitude of conditions such as organ disorders, rheumatism, respiratory conditions, dermatological disorders, and psychological conditions; while MFD aims to target trigger points, create mechanical connective tissue changes, address scar tissue adhesions and facilitate cortical reorganisation.
Getting intimate with fascia
A large portion of the didactic part of the course talks about the integumentary system. The skin is actually far more complex than we often consider and understand based on the time dedicated to learning about it during our training. DaPrato’s course helped me remember that the fascia is a living and dynamic tissue, and it is the biggest organ in the body. It provides a huge amount of support to the body, connecting everything to everything. We can’t break it down and muscles would not function without being surrounded by fascia. For example, a muscle like piriformis changes action depending on what position of the hip. Anatomy is so dynamic and multifunctional and we need to understand how it is gliding, moving, and changing. Fascia is what makes the kinetic chain functional and possible.
For movement to be possible at a joint, our tissues need to be able to both glide and fold upon themselves. "Myofascial manipulation involves a stimulation of intrafascial mechanoreceptors. Their stimulation leads to an altered proprioceptive input to the central nervous system, which then results in a changed tonus regulation of motor units associated with this tissue." (Schleip., 2003, p.17). What this means is that for tissues to move and glide we need to consider both the mechanical properties of the tissues and the neurophysiological changes that occur as a result of stimulation of these tissues.
We need to steer away from the term “breaking up adhesions” because for the length of treatment time, such physiological collagen failure is unlikely and instead we are more likely to see changes in range and function by improving gliding of tissues layers and movement of fluid and viscosity of ground substance (Schleip., 2003).
Our ideas of stretching need to shift from lengthening tissues to creating more space, improving gliding and facilitation of movement through slings or chains of muscles, all of which are connect and work functionally together because of the fascia that connects them.
While we currently don’t have an standardised tool that to measures the viscosity of the ground substance in tissues we can continue to rely on our palpation finds and the quality of the tissues we feel. This is one of the beautiful things about the skin and fascia, it is so close to the surface that it can be readily palpated.
It’s all about the space that is in-between
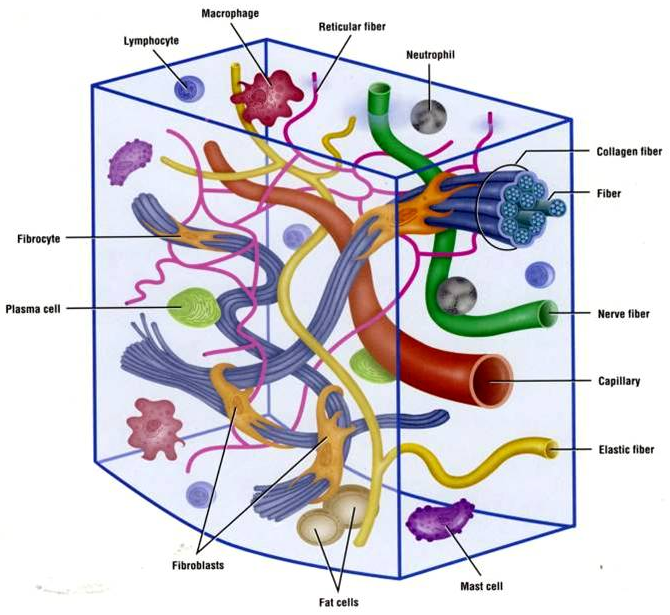
Image source from Google Images
Ground substance is the sugar-protein molecule that creates the interstitial fluid found in the extracellular matrix of our tissues, or as I like to think about it, the space that is in between everything else and the bit that is coloured white in anatomy drawings. The important part to understand about ground substance is that MFD is most likely to stimulate the sensory nerve endings found in interstitial receptors, which in turn create a change in vasodilation (Schleip., 2003). Therefore decompression therapy is likely to change viscosity of interstitual fluid, improve vasodilation and stimulate a neurobiological reaction, all of which creates a pro-inflammatory response.
Because it is the in-between substance it is very difficult to quantify in our assessment, but as we all know, when palpating tissues we often feel changes in the viscosity of tissue density through our fingers, indicating a change in the ground substance, and likely implying a change in the lymphatic drainage of that area. When ever I palpate a post operative knee and feel the layers of tissue thickening and fluid build up that isn't moving, I think of ground substance that has lost it's viscosity. Almost like a fibre based drink mixed with water that sat too long without stirring. Both ground substance and hyaluronic acid are important substances found between the layers of fascia and surrounding our cellular matrix are the reason why we have come to understand that gliding of tissues is vital for normal healthy movement. Our treatment targets the ground substance, the white stuff that suspends everything in the connective tissue and it fills the gaps and connects everything to everything else.
"It seems that a major function of this intricate network of interstitial tissue receptors is to fine tune the nervous system's regulation of blood flow according to local demands, and that this is done via very close connections with the autonomic nervous system" (Schleip., 2003, p.17).
Thixotropy and tensegrity
In order to change the viscoelastic properties of tissues we need to put energy into the system. This is known as thixotropy and refers to the energy required to create flow of fluid. I really like this term as it helps me conceptualise that our manual therapy and neuromuscular rehabilitation is creating an energy flow in and out of the body, trying to help it normalise movement and function.
Tensegrity is a made up word about tension and integrity of soft tissue structures and the adaptability of tissues to force. When applying this term to myofascial decompression we can understand that movement of a local tissue has regional effects and creates movement in fascia in other areas of the body. Because the integumentary system is a continuous interface, we are able to direct treatment and force vectors to impact a body region, without directly applying the cups on that site. This is clinically applicable in this sense because we are often encouraged to look at body regions above and below the affected area from a joint perspective, but are we looking enough at the local and regional movement of the fascia.
Final thoughts
Aside from the points discussed above which are unique to this course, there were two final messages which I need to remember and practice with patients who I choose to use this treatment with. The first is that neuromuscular rehabilitation is a must. A non-negotiable aspect of the MFD is the use of movement during treatment and using specific exercises to retrain the movement after treatment. What will take time to practice is combining MFD with AROM or PROM during treatment and then understanding which muscles to facilitate and rehabilitate after treatment. This is not something that is set in stone for each patient and comes back to our clinical reasoning of the problem which lead us to select MFD in the first place. The second is having a sound understanding of clinical anatomy and tissue pathology. You can’t apply a decompressor (cup) to any tissue. It doesn’t go well with bursas and feels very different over a superficial bone. Skin integrity, immunity, blood disorders and pregnancy are always considered in reasoning if this approach is the best option, just as we decide treatment suitability of all our other techniques.
I look forward to combing MFD with my other manual therapy approaches and adding a new tool into my tool-kit of treatments. Within my first week I have had great results with patients who were struggling to regain their ROM and look forward to challenging some of the current treatment pathways I have developed overtime, to see where MFD can be used and observe the outcomes.
SS
References
Schleip, R. (2003). Fascial plasticity–a new neurobiological explanation: Part 1. Journal of Bodywork and movement therapies, 7(1), 11-19.
Schleip, R. (2003). Fascial plasticity–a new neurobiological explanation Part 2. Journal of Bodywork and movement therapies, 7(2), 104-116.