Cervical Radiculopathy or Infected Root Canal?
The bidirectional relationship of pain between the jaw/face and cervical spine is a clinical challenge for many therapists. It requires a sound understanding of pain mechanisms, behavioral patterns of referred pain and the clinical tools to assess what the primary contributing factors are. This is a case study covers the pain presentation of a patient with concurrent neck pain, arm pain and jaw pain.
History of presenting complaint
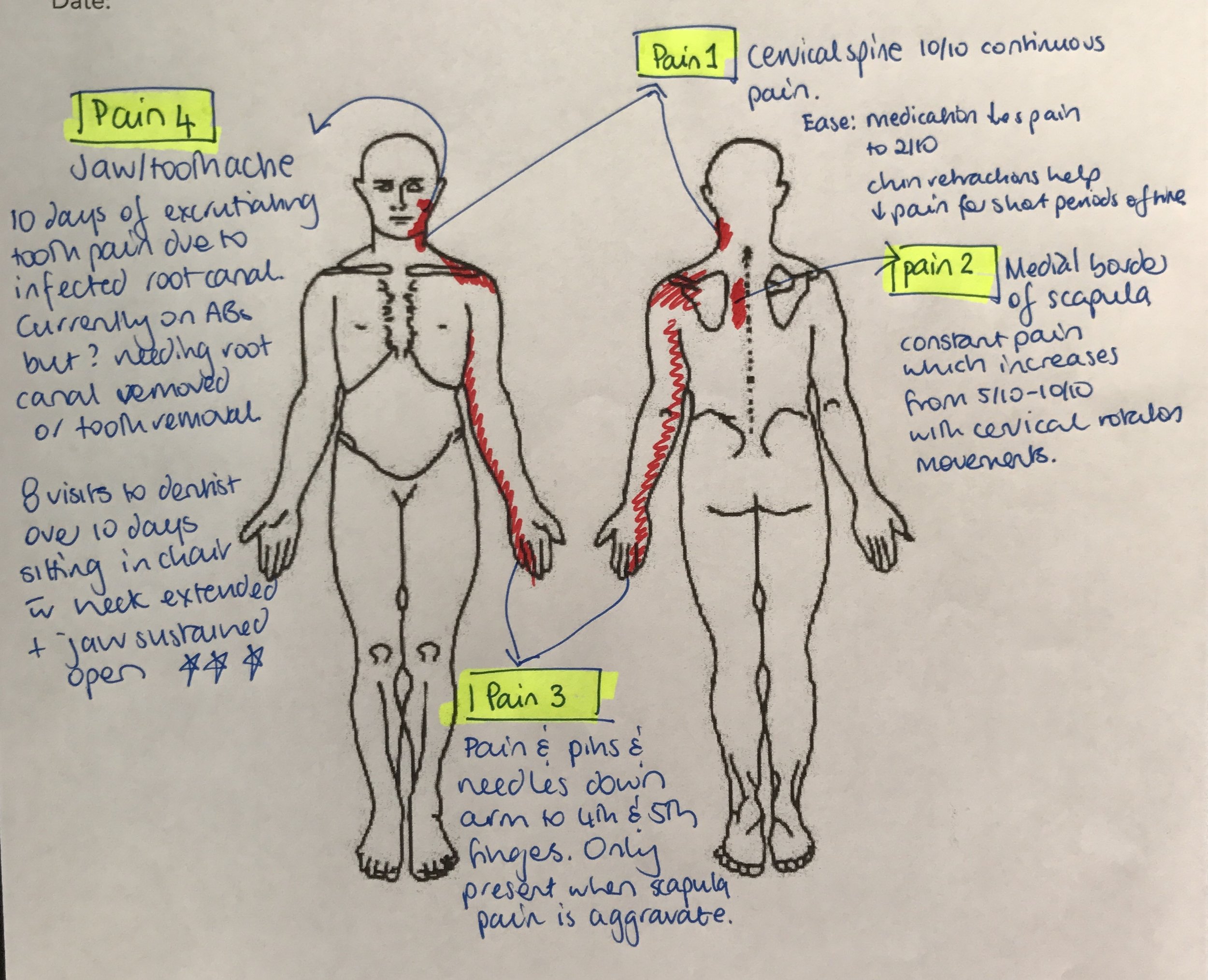
Mrs. P presented with excruciating left sided neck pain, left medial scapula pain and pain radiating down her left arm into her 4th and 5th fingers. She was distressed by the severity of her pain and worried that her neck had 'given way' because there was no mechanism of injury she could attribute to the onset of her symptoms. I was informed that previous cervical MRI had detected bony spurs around the C5 vertebrae and she was now booked in for a repeat MRI and appointment with a neurosurgeon to discuss further treatment options for her pain.
Upon further questioning the patient revealed that her primary pain was on the left side of her neck. Constant in nature and fluctuating between a 5-10/10 in severity. This pain was limiting her ability to move her neck and when she did, a second sharp pain came on in the medial border of her scapula.
There was a third pain which came on her medial scapula pain had been present for 20-30 minutes and it radiated down her arm to the 4th and 5th fingers.
I thought that this completed the pain presentation and then asked "What about your jaw - do you have any pain there? And are you experiencing any headaches?"
Mrs. P replied "yes and yes".
The patient had not thought there was a connection between her two weeks of jaw pain, headaches and the symptoms in her neck and arm. Two weeks prior she had developed a terrible pain in her left jaw and the dentist diagnosed this as an infected root canal. She had been to the dentist 8 times in the past two weeks and spent considerable time in a dental chair for treatment prior to coming to Physical Therapy. During her dental visits her neck was rested in right lateral flexion, rotation and extension and the a jaw was sustained in a maximally opened position.
Body Chart
hypothesis list
Before generating a hypothesis list there were a few questions that came to mind about the unusual presentation of this patient's pain.
- Could the pain be a cervical radiculopathy? It doesn't follow the pain distribution of a C5 radiculopathy but are there other neural signs? Also, there is no prior history of cervical radiculopathy.
- Is the pain originating from the cervical spine, temporomandibular joint or infected root canal. The onset of the pain coincides with the development of tooth pain and during this time the jaw was kept open for prolonged periods and the neck sustained in a position of lateral flexion and extension away from the left side.
- Bony spurs can be a normal part of ageing seen in the cervical spine, so how important is that information to this pain presentation?
- Is this scapula pain a cloward sign?
- Is this a somatic referral or neuropathic referred pain?
- Is the arm pain coming from the thoracic spine or cervical spine?
- Are the cervical spine pain and jaw/tooth pain directly linked or concurrent?
- Where do I direct my treatment day 1?
Hypothesis list (what's going to make it into the top 3?):
- Cervical radiculopathy
- Temporomandibular joint dysfunction (TMD)
- Infected root canal with referred pain to the cervical spine
- Cervical spine zygopophyseal joint dysfunction
- T4 syndrome
- Cervical discogenic neck pain with a cloward sign and nerve impingement
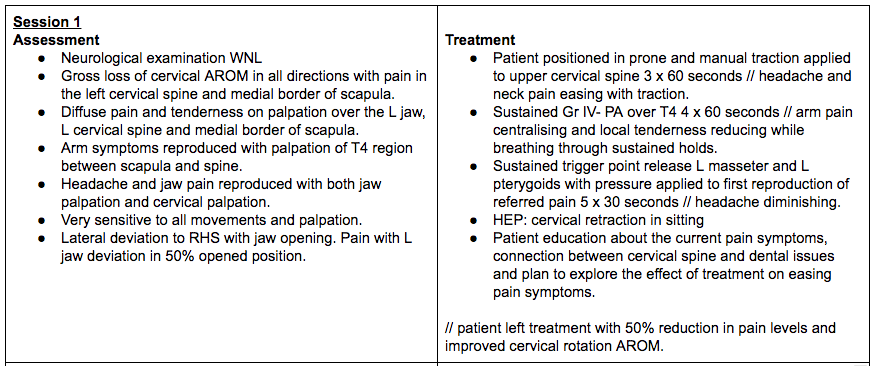
Systematically I needed to assess the jaw, neck and thoracic spine all together in one day. Try collect enough data to link or unlink pain areas and to find a point to treat. This is definitely a challenge for a patient with severe pain day 1. If you read through the tables (at the bottom) you will notice that while I did assess and treat a lot, I was very careful with the grade of movement and amount of pain reproduction I was hunting for. Keeping severity, irritability and nature in mind the whole time while trying to decipher the clues.
Where to begin?
Day 1, I really wanted to find out if this patient had a cervical radiculopathy, if C5 was the main level contributing to her pain, and if there was any connection between her tooth/jaw symptoms and her neck pain. The treatment was focussed on manual cervical traction, sustained GR IV- PA over T4, sustained trigger point release left masseter and lateral pterygoids and a HEP over cervical retraction in sitting. The tables of treatment for day 1-3 are below the references if you'd like to see the specific details but, the summary is that I treated jaw, neck and thoracic spine all on day 1 and reassessed the asterisks after each treatment to evaluate the effectiveness of each.
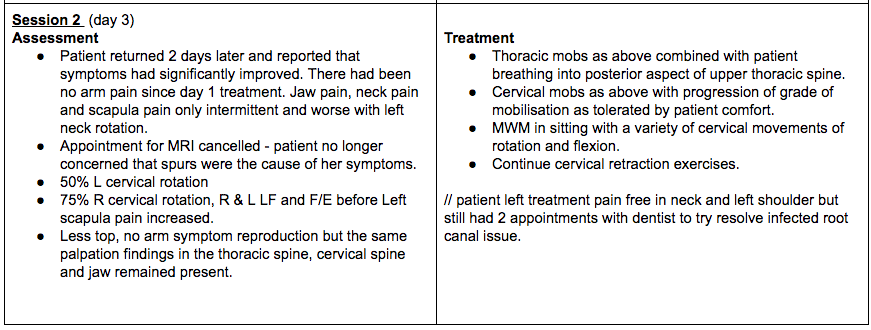
The patient returned 2 days later and she was very happy with the amount of pain relief she had experienced since the treatment and more confident that either the time sitting in the dental chair, or the dental procedures were significantly increasing her pain. Despite her pain continuing, she felt more reassured that her C5 hadn't 'given up on her' and that we were able to address her pain with treatment directed at the thoracic spine, cervical spine and jaw. The treatment for day 2 was a continuation from day 1 with the addition of MWM in sitting. Mrs P responded well to a combination of treatments but the most pain relief was achieve with cervical spine mobilisation.
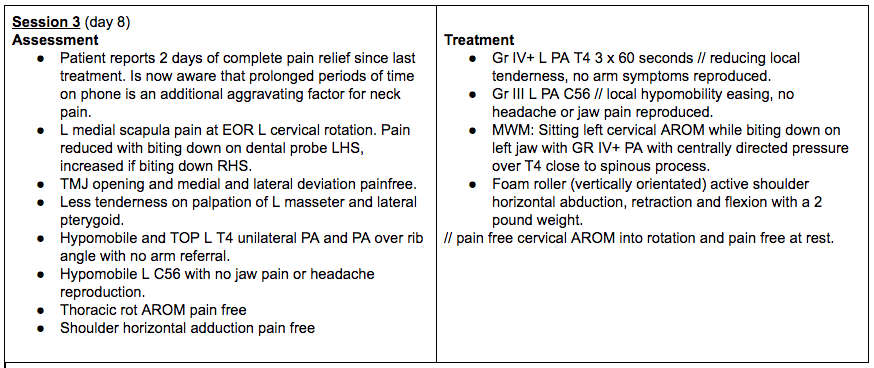
Day 3, the following week, was really interesting. At this time the patient had experienced 2 days of complete pain relief and while her tooth continued to be infected and painful, she could tolerate more assessment and load. I was curious to understand if her jaw pain was limiting her neck movement. Using a tongue depressor I asked the patient to bite down on the right side and turn her head to the left. This significantly increased her left neck pain. The bite down on the left (to a comfortable level for the tooth) and turn to the left - no neck pain.
It the past many teachers have encouraged me to check the TMJ in neck patients but never fully explained what that might involve. Does checking the TMJ involve palpation, assessing active range of movement, doing palpation and movement in combination with neck movements? Usually I assess opening, left and right lateral movements and check for deviations and clicking during range. This was the first time I looked at active bite and it's impact on movement and both the patient and myself were excited by what we found.
Day 4, the patient returned 2 weeks later and reports that her pain had completely resolved. Following the previous treatment she used the cervical rotation with tongue depressor as an exercise two times a day for 4 days. Her tooth pain had settled somewhat and she was scheduled for a root canal in 2 weeks but the pain in her neck, shoulder, arm were completely clear. The patient also described that she had been practicing her thoracic mobility exercises daily and replaced her pillow to support her neck while sleeping in side lying. Overall we were both very happy with the improvement and recovery. The patient was relieved that no MRI was needed and now saw the connection between her tooth symptoms and neck symptoms and how both contributed to her overall pain, and how a combination of Physiotherapy and Dentistry would help address these problems.
Mal-occlusion and posture
This was the first time I have used occlusion to address a cervical mobility problem and have spent considerable time reading literature trying to understand the neurophysiological and biomechanical reason for why it worked. Generally, everything I read about cervical spine disorders and TMD suggests that the muscles of mastication are overactive and need to reduce in work load. For this patient the treatment was the complete opposite. Maybe it comes down to the mechanism of injury? Or maybe it was the unusual high frequency of jaw opening in a patient with pre-existing neck stiffness lead me to think that the jaw needed to be closed back down again?
A study by Visscher, Slater & Naeije (2000) on the kinematics of the human mandible for different head postures showed that there is movement of the incisal points when the head changes between a forced upright (military), neutral and forward head posture. “According to this study, the opening movement path of the incisal point with the head held in a military posture is shifted anteriorly relative to its path in a natural head posture. In a forward head posture its path is shifted posteriorly. During lateroflexion, the movement path of the incisal point deviates to the side the head is movement to” (2000, p.303).
With Mrs. P, her head was held in right lateral flexion therefore the incisal points will have moved to the right side. These changes are at maximum 0.19mm, so the clinical relevance of these small changes remains to be determined, however it can be speculated that with a forward head posture and right lateral flexion the intra-articular distance in the TMJ would be increased.
Points of interest
The link between the tooth pain and limited cervical rotation was an interesting aspect of this case study. You can argue that neurophysiologically these two regions are linked via their afferent input via the trigeminocervical nucleus. While this link existed on day 1 & 2, by day 3 the somatic referral was no longer reproducible. Biomechanically however, the tooth pain was preventing this patient from using their left jaw and this was altering the load of the left cervical spine in movement. Using a tongue depressor was a simple differentiation tool that allowed us to explore if her mouth movements were impacting neck movements, and the pain was rapidly reduced in left cervical rotation when the patient was cued to gently bite down the left teeth onto the piece of wood. Not enough to cause tooth pain but enough to get some muscle activation and see what role inhibition had in this pain presentation.
Most treatment options discussed in the literature refer to restoring opening and reducing activity in the muscles of mastication. It seems that all evidence points towards occlusion reducing cervical rotation through overactivity of muscles of mastication yet in this case study it did the opposite. Does this mean this is an edge case or does this mean if could be a new approach for treatment?
Another interesting point from this case study was that there were multiple concurrent issues blending into a pain pattern. Sometimes we can find a single root for a pain presentation and addressing that root, addresses all the others. This time it was not the case. I can't change the fact this patient has an infected nerve in her tooth and that she needs either a root canal or tooth removal. But I can address the biomechanics of her jaw movements and treat the other pain areas resulting from this initial problem to provide pain relief and restoration of function. It wasn't that simple to find and required a multi-modal approach.
Summary of research
I wanted to share this case study because it raises many questions:
- Is there a causal relationship between occlusion and neck pain?
- What is the neurophysiological relationship between occlusion and cervical rotation?
- What is the best way to quantify postural abnormalities?
- What is the significant of this information regarding balance, occlusion and posture in addressing the patient’s problem of neck pain?
There is a huge amount of interest around the topic of occlusion and posture yet the amount of high quality evidence is lacking. I read articles ranging from neuroscience, physical therapy, dental and osteopathic journals and they all say the same thing - we don’t fully understand this complex system even though intuitively we know how linked the stomagnathic and cervical regions are. Secondly, there is no easy way to explain the complex relationship and interaction between somatosensory, vestibular and visual inputs.
Posture is a state of biomechanics equilibrium with visual, vestibular and sensory input (Ciancaglini, et al., 2009). After input from these three main system there is complex processing within the central nervous system and multiple parts of the brain. It is difficult to say poor posture is caused by a single factor and delineate such an interdependent system. As such, there is no commonly agreed upon neurophysiological and biomechanics model explaining the connection between the posture of the jaw and cervical spine and how posture alters pain.
"At the present, there is no scientific evidence to support a correlation between occlusal and postural problems from either a functional or morphological view. Therefore, there is even less evidence for a cause-effect relationship. This does not exclude the opportunity to study with a rigorous and meticulous scientific protocol the problem of the relationship between occlusion and posture, both in healthy subjects and in patients" (Ciancaglini, et al., 2009).
Overall tips from research
You have to assess the neck.
Don't confuse pain and posture. We know a lot about the bidirectional relationship of pain through the trigeminocervical nucleus (Walczynska-Dragon, et al., 2014) but we are still learning about wether altered jaw occlusion causes postural problems and vice versa. Make sure you assess the neck in patients with jaw pain.
Consider posture as a part of the whole picture.
When looking at the jaw during a forward head posture, the incisor point and both temporomandibular condyles move posteriorly. Lateral movement and vertical movement is not effected as much with forward head posture. Ohmure et al (2008, p. 798) found the condyle can move on average 1.1mm posteriorly during a forward head posture. This is thought to add an additional posterior force to muscles and passive structures of the TMJ. Another study found that “prolonged altered head posture due to a cervical dysfunction leads to asymmetric EMG activity in the jaw muscles (particularly masseter)” (Ballenbeger, et al., 2012, p. 315). Therefore, head posture needs to be a consideration in TMJ patients.
It is a valid approach to treat the neck with manual joint mobilisation and deep cervical neck flexor training in patients with TMD (La Touche, et al., 2009). La Touche et al (2009) look at the effect of treatment which is directed at the cervical spine and the impact it has on TMD. Their treatment protocol included only interventions for the cervical spine including: upper cervical flexion mobilisation in supine, central PA mobilisation over C5 in prone, deep cervical neck flexor training with a biofeedback cuff in supine. Following this treatment there was an immediate increase in pain pressure threshold, reduced fascial pain and increased mouth opening by 4.5mm. This study included a small sample size and the “cervical” treatment wasn’t the approach I would have taken but the results did validate that cervical spine directed treatments immediate have a hypoalgesic effect on orofascial pain.
The presence of limited cervical rotation and pain on palpation of the shoulder and neck muscles is not a differentiating feature between a cervical spine disorder and TMD. In fact, De Laat et al (1998) found in their study that TMD patients were highly likely (between 77-93% of patients) to display limited cervical rotation C0-C4, while these limitations were only found in 20-46% of control subjects. What this means is that neck ROM has to be a consideration in TMD.
As it currently stands, it is difficult to delineate all of the systems that contribute to posture and balance and clearly identify the amount of contribution each has. "The convergence of all the proprioceptive information on supra spinal motor centres and spinal circuits allows a series of reflex controls on the posture of the entire body, included the stomatognathic system" (Ciancaglini, et al., 2009, p.90). This is a complex system with both medullar and supra spinal control. Understanding what role occlusal information plays in maintaining postural control is hard to delineate from other inputs and processing centres. There is no way to easily separate occlusion and therefore quantify it’s involvement from a neurophysiological perspective.
Nothing I read talks about using occlusion as a treatment strategy but the mechanism of injury for this patient pointed to that as a treatment direction. The patient demonstrated a 100% recovery in 4 sessions, which we were both very happy about. She also went on to have a root canal after her neck pain resolved. Somethings we do can’t yet be explained by EBP. Just because there isn’t an EBP to prove efficacy doesn’t mean the treatment isn’t effective. Not everything can be tested in a randomised controlled trial.
I hope this case study helps to explain my clinical reasoning and approach to managing a patient with severe neck pain and jaw pain, discuss the questions and thoughts I had about this pain presentation and enlighten you on the key ideas I found in the research about occlusion, posture and pain. SS
References
Alpini, D. C., Di Berardino, F., Mattei, V., & Cesarani, A. (2012). The correlation between dental occlusion and posture is different in trained versus nontrained subjects. Sport Sciences for Health, 7(2-3), 83-86.
Baiatilde, M., de Vasconcellos Vilella, O., & da Silva, G. C. H. (2012). Posture alterations related to temporomandibular joint dysfunction. Journal of Dentistry and Oral Hygiene, 4(1), 1-5.
Ballenberger, N., von Piekartz, H., Paris-Alemany, A., La Touche, R., & Angulo-Diaz-Parreño, S. (2012). Influence of different upper cervical positions on electromyography activity of the masticatory muscles. Journal of manipulative and physiological therapeutics, 35(4), 308-318.
Bartley, J. (2011). Breathing and temporomandibular joint disease. Journal of Bodywork and movement therapies, 15(3), 291-297.
Ciancaglini, R., Cerri, C., Saggini, R., Bellomo, R. G., Ridi, R., Pisciella, V., ... & Heir, G. (2009). On the symposium: consensus conference posture and occlusion: Hypothesis of correlation. international journal of stomatology & occlusion medicine, 2(2), 87-96.Chicago
Corrêa, E. C. R., & Bérzin, F. (2005). Temporomandibular disorder and dysfunctional breathing.
Cuccia, A., & Caradonna, C. (2009). The relationship between the stomatognathic system and body posture. Clinics, 64(1), 61-66.
Grondin, F., Hall, T., & von Piekartz, H. (2016). Does altered mandibular position and dental occlusion influence upper cervical movement: A cross–sectional study in asymptomatic people. Manual Therapy.
Grossi, D. B., & Chaves, T. C. (2015). Physiotherapeutic treatment for temporomandibular disorders (TMD). Brazilian Journal of Oral Sciences, 3(10), 492-497.
Hanke, B. A., Motschall, E., & Türp, J. C. (2007). Association between orthopedic and dental findings: what level of evidence is available?. Journal of Orofacial Orthopedics/Fortschritte der Kieferorthopädie, 68(2), 91-107.
Korbmacher, H., Eggers-Stroeder, G., Koch, L., & Kahl-Nieke, B. (2004). Correlations between anomalies of the dentition and pathologies of the locomotor system—a literature review. Journal of Orofacial Orthopedics/Fortschritte der Kieferorthopädie, 65(3), 190-203.
La Touche, R., FERNÁNDEZ‐DE‐LAS‐PEÑAS, C., FERNÁNDEZ‐CARNERO, J., Escalante, K., ANGULO‐DÍAZ‐PARREÑO, S., PARIS‐ALEMANY, A., & Cleland, J. A. (2009). The effects of manual therapy and exercise directed at the cervical spine on pain and pressure pain sensitivity in patients with myofascial temporomandibular disorders. Journal of oral rehabilitation, 36(9), 644-652.
La Touche, R., París-Alemany, A., von Piekartz, H., Mannheimer, J. S., Fernández-Carnero, J., & Rocabado, M. (2011). The influence of cranio-cervical posture on maximal mouth opening and pressure pain threshold in patients with myofascial temporomandibular pain disorders. The Clinical journal of pain, 27(1), 48-55.
März, K., Adler, W., Matta, R. E., Wolf, L., Wichmann, M., & Bergauer, B. Can different occlusal positions instantaneously impact spine and body posture?. Journal of Orofacial Orthopedics/Fortschritte der Kieferorthopädie, 1-11. Chicago
Mulet, M., Decker, K. L., Look, J. O., Lenton, P. A., & Schiffman, E. L. (2007). A randomized clinical trial assessing the efficacy of adding 6 x 6 exercises to self-care for the treatment of masticatory myofascial pain. Journal of orofacial pain, 21(4), 318.
Ohmure, H., Miyawaki, S., Nagata, J., Ikeda, K., Yamasaki, K., & AL‐KALALY, A. (2008). Influence of forward head posture on condylar position. Journal of oral rehabilitation, 35(11), 795-800.
Ries, L. G. K., & Bérzin, F. (2008). Analysis of the postural stability in individuals with or without signs and symptoms of temporomandibular disorder. Brazilian oral research, 22(4), 378-383.
Tecco, S., Tete, S., & Festa, F. (2007). Relation between cervical posture on lateral skull radiographs and electromyographic activity of masticatory muscles in caucasian adult women: a cross‐sectional study. Journal of oral rehabilitation, 34(9), 652-662.
Testa, M., Geri, T., Gizzi, L., Petzke, F., & Falla, D. (2015). Alterations in Masticatory Muscle Activation in People with Persistent Neck Pain Despite the Absence of Orofacial Pain or Temporomandibular Disorders. Journal of Oral & Facial Pain & Headache, 29(4).
Visscher, C. M., Huddleston Slater, J. J. R., Lobbezoo, F., & Naeije, M. (2000). Kinematics of the human mandible for different head postures. Journal of oral rehabilitation, 27(4), 299-305.
von Piekartz, H., & Lüdtke, K. (2011). Effect of treatment of temporomandibular disorders (TMD) in patients with cervicogenic headache: a single-blind, randomized controlled study. CRANIO®, 29(1), 43-56.
Walczyńska-Dragon, K., Baron, S., Nitecka-Buchta, A., & Tkacz, E. (2014). Correlation between TMD and cervical spine pain and mobility: is the whole body balance TMJ related?. BioMed research international, 2014.
Yamada, R., Ogawa, T., & Koyano, K. (1999). The effect of head posture on direction and stability of mandibular closing movement. Journal of oral rehabilitation, 26(6), 511-520.
Yeampattanaporn, O., Mekhora, K., Jalayondeja, W., & Wongsathikun, J. (2014). Immediate effects of breathing re-education on respiratory function and range of motion in chronic neck pain. Journal of the Medical Association of Thailand= Chotmaihet thangphaet, 97, S55-9.