Hip: Athletic Groin Pain Part 2
Welcome back to part two of the Athletic Groin Pain series. Here we discuss how the clinical assessment of groin pain correlates with MRI and what biomechanical analysis tells us about the AGP population. This blog is following on from Part 1.
Following the clinical examination, each patient was referred for an MRI to see how the clinical examination correlates with medical imaging. Here are the stats (Falvey, et al., 2015, p. 4):
- ~34% of cases had 2 abnormal findings and ~30% had >3 abnormal findings on MRI. Only 7% of cases had 'normal image findings'.
- Pubic bone marrow oedema was reported on nearly 70% of cases.
- <40% of cases had abnormal adductor image findings and about half of cases had abnormal PA image findings.
Following the MRI each patient was given a diagnosis from the categories above and this data showed that PA injury is by far the most common source of pain in patients with AGP (Falvey, et al., 2015, p. 4).
- Pubic aponeurosis injury ~63%
- Adductor injury ~21%
- Hip joint injury ~15%
- Hip flexor injury ~3%
- Inguinal injury <1%
"This is the largest prospective cohort of patients with athletic groin pain in the literature to date, and the first to directly combine clinical and MRI findings in making a diagnosis" (Falvey, et al., 2015, p. 5). What this has shown is that there is a close correlation between what the examiners found/suspected to be the diagnosis and what the MRI showed. In fact, this study showed that when MRI is combined with clinical tests, the probability the diagnosis being correct increases from 62-93% (Falvey, et al., 2015, p. 6). So when referring a patient for a scan be sure to know first what you're expecting to find and how this information relates to your patient and can assist in diagnosis.
Another interesting point from this study was the interpretation of the adductor squeeze test, which again was painful in >80% of cases. The authors found that the SQ was closely associated with TOP over the adductor origin and pubic aponeurosis (PA) and bone marrow oedema on MRI, but not specific to loading the adductor origin. As a stand alone test it lacks diagnostic validity and we should expect to find this test positive in most cases. The SQ test is not sensitive to ruling out PA injury which indicates that "pain-free direct palpation of the adductor origin is the most accurate clinical test to exclude adductor pathology" (Falvey, et al., 2015, p. 5).
A final point from the first paper that the authors raises was how the adductor squeeze test guides exercise prescription. They ask the question does pain on the SQ test mean we need to give our patients isometric adductor strength exercises? Furthermore, does pain on loading mean there is a strength deficit? Perhaps we should interpret the findings of this test as an indication there is poor tolerance to load over the public tubercle and that further examination of biomechanics will help us understand why tissue overload is occurring?
PART 2 - HOW DOES BIOMECHANICS CHANGE WITH AGP?
The second part of the article was published less that four months ago and focusses on the biomechanical patterns that patients with AGP demonstrate with change-of-direction movements. To date, biomechanical segmental coordination is not a consideration in research around the clinical assessment of AGP, yet you'd commonly see it in the research for ACL injuries or PFJS.
The concept that biomechanical overload can lead to tissue failure is not a new concept in Physiotherapy, and yet, with AGP we might still be stuck trying to find the source of the pain rather than the cause. This paper aimed to study the movement patterns implemented by people with AGP and related this pattern to the five anatomical diagnoses from article 1.
Franklyn-Miller et al (2016) designed a maximal multidirectional test where a participant ran 5m forward as fast as they could, planted their outer foot, and made a single turn of 110 degrees before running 5m in the new direction as fast as they could.
DO PEOPLE WITH AGP PRESENT WITH A SPECIFIC MOVEMENT PATTERN?
In this study 322 male participants were used (from 382). Each patient was examined and diagnosed as seen in part 1. Then the maximal multidirection test (described above) was performed and the authors used force plates and vicon motion systems to collect data on ground reaction forces and movements.
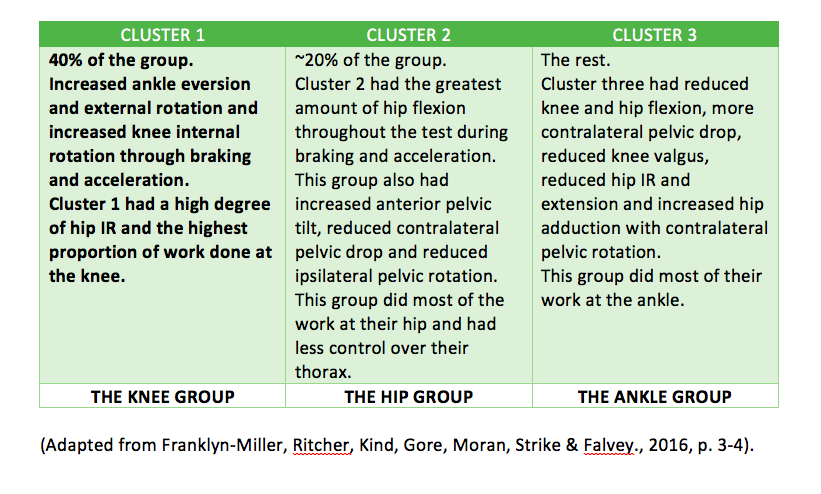
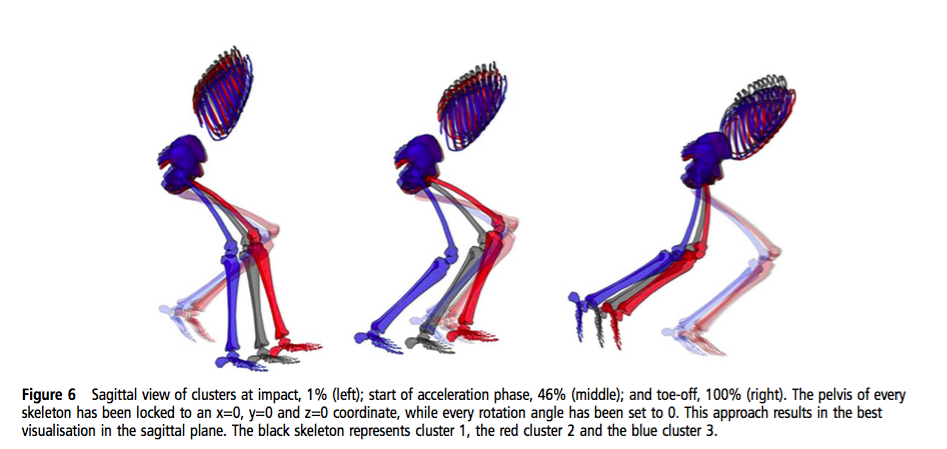
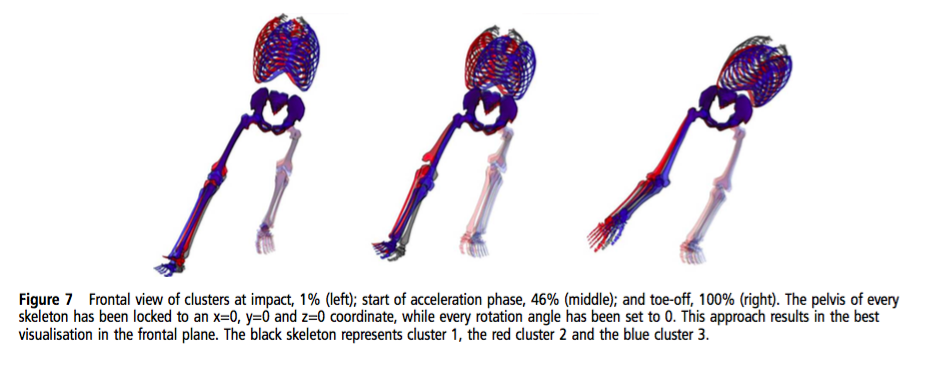
"Three distinct movement strategies (clusters) were identified with differences in braking and acceleration phases by joint and plane of movement kinematics and kinetics by joint and plane" (Franklyn-Miller, et al., 2016, p. 2).
(Franklyn-Miller, et al., 2016, p. 6)
(Franklyn-Miller, et al., 2016, p. 7)
The outcomes from this study did not identify a consistent weakness and three clusters were found to be present in AGP. This raises the questions of "what is an optimal movement pattern?" Franklyn-Miller and colleagues (2016) are hoping that future research might help us understand this further.
What about the trunk?
"The thorax accounts for upwards of 35% of body mass, its position is influenced by pelvic orientation and controlled in part by the abdominal muscles... which form the inguinal ligament superiorly and join the tendinous fascia of the common adductors inferiorly to form an aponeurosis at the pubic symphysis" (Franklyn-Miller et al., 2016, p. 4-5). What this explains is that 1/3 of body weight is positioned above the groin and over 60% of participants identified this proximal site as their primary area of pain!
Summary
In summary, AGP is an umbrella term that encompasses many possible pathologies around the anterior groin and hip. When assessing patients with AGP it is also important to use a battery of tests and specific palpation to understand where the painful tissues are. Even though there are many causes of AGP, most rehab protocols look similar, and in the 2-part series by Franklyn-Miller et al, the authors provide convincing evidence to suggest that a one size fits all approach is not going to be effective, specifically in regards to coaching of change-of direction movements and biomechanics.
- "No significant relationship exists between movement clusters and the anatomical diagnosis" (Franklyn-Miller et al., 2016, p. 4).
- The amount of hip flexion differed significantly between each cluster. "The different hip flexion angles found among clusters are likely to alter the hip shearing force and suggest different sites of load" (Franklyn-Miller et al., 2016, p. 4).
- The ankle is not considered often enough in hip and knee examination.
- "The position of the trunk must be considered" (Franklyn-Miller et al., 2016, p. 5).
When I read articles like the ones discussed in this blog I am excited to learn more about the topic. I love it when papers succinctly summarise many rambled thoughts I've had, or explain clinical observations that I'm yet to fully understand, and in the meantime raise clinical questions about where further research is needed. It not only expands my knowledge but also demands me as the reader to be more intrigued and curious with my patients, and to think more critically and analytically as to why their problem as occurred and how best I can help them.
Sian
References
All the articles from this blog are open source through BMJ so please read them for yourselves!