Cervical Radiculopathy Part 2 - Assessment & Diagnosis
The first part of this blog series discussed the difference between nociceptive and neurogenic pain presentations and the subjective examination for a patient with suspected cervical radiculopathy. Now we continue on to the Physical Examination. Once you have established a hypothesis list, the next step is to determine if cervical radiculopathy is the correct diagnosis.
What can our assessment include?
- Cervical AROM
- Neurological examination
- Neurodynamic examination
- Compression and distraction tests
- Spurling test
- Shoulder abduction test
- Other shoulder clearing tests
- Thoracic spine clearing tests
- Palpation of the cervical spine
But hold on a second….. because that is way too much for day 1 and I can guarantee that if you’re dealing with an acute nerve root, your assessment needs to be kept to a minimum and you need to perform enough to confirm your diagnosis but also not aggravate your patient.
With this goal in mind, there is second consideration to be made for the physical examination. We need to prevent unnecessary aggravation but we also need to develop a cost-effective and reliable means for diagnosing cervical radiculopathy clinically. In the search of this answer, many papers have investigated clinical tests to determine if a clinical prediction rule (CPR) exists. Six tests are commonly noted to be highly specific for CR (Apelby-Albrecht., 2013; Wainner, et al., 2003). Of these tests, the first five are the ones most commonly included in the CPR:
- Reduced cervical rotation <60 degrees to the affected side.
- Reduction of symptoms with shoulder abduction
- Reduction of symptoms with cervical distraction
- Provocation of symptoms with the Spurling test
- Provocation of symptoms with the median nerve biased neurodynamic test.
- Provocation of symptoms with the Valsalva maneuver – less commonly included.
Clinical prediction rules
From this current clinical prediction rule: Spurling test, distraction test, ipsilateral rotation <60 degrees and ULTT1 have a 99% specificity when all four items are positive and 94% specificity when 3 items are positive (Waldrop, 2006). The first challenge for clinicians using a clinical prediction rule is evaluating severity and irritability as those tests alone don’t provide enough depth of information to determine this. Usually questioning during the subjective assessment tells us more about severity and irritability. The second challenge in diagnosis of cervical radiculopathy is identifying the level of root compression and again this comes from the neurological examination combined with specific localization of symptoms during the subjective examination.
Where does the neurological exam fit in?
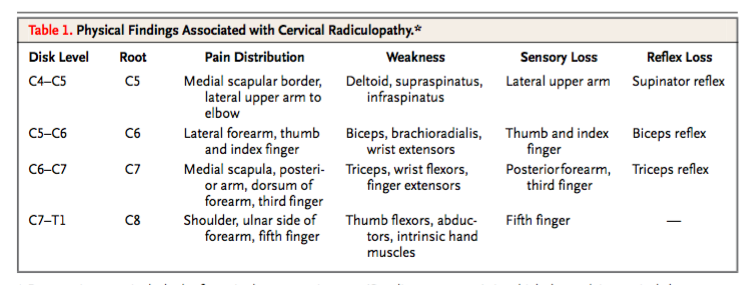
Clinically I always perform a neurological examination because it is vital to gain a base line for reflexes, strength and sensation to determine if the patient is worse/better/same other than pain distribution. Normally a neurological examination is not provocative. The next question to consider is how often you repeat these tests on subsequent treatments? If the neurological examination is normal day 1 – when and how often would you retest? For me, I retest if symptoms change. If the neurological exam is not normal but the patient is suitable for conservative treatment, I would retest quite frequently. From what I’ve experienced, reflexes are slow to return but strength and sensation much faster. It is an important part of examination of the health of the nerve.
I keep this chart with my for each assessment to compare and clarify my neurological examination findings. The table below also describes the expected abnormalities with C5, C6, C7 & C8 radiculopathies.
Physical examination findings for cervical radiculopathy (Cardette, Phil & Fehlings., 2005, p. 394).
Which neurodynamic test to choose.
There are 4 different neurodynamic tests to bias the median, ulnar and radial nerves. In 2014, I tool a course with Michael Shacklock on the neurodynamics of the upper limb. I was fortunate to learn in great depth how to perform these ‘standard neurodynamic tests’. What I also learnt from Michael is that these standard tests put the nervous system through a lot of movement. What I never completely understood (prior to taking the course) is that when a patient presents with an acute radiculopathy, it is unlikely they can achieve the full expression of these movements and to try take their upper limb to the end of range can be potentially very provocative. During the course we learnt about regressions of these tests (stage 1) and progressions (stage 3), which are described in detail in his book Clinical Neurodynamics. I would highly recommend learning these to improve your clinical assessment and prevent aggravation of your patients. I've also previously discussed each level in this blog.
ULT1 & 3 (both with a median nerve bias) have the highest specificity in diagnosing cervical radiculopathy (Apelby-Albrecht., 2013; Wainner, et al., 2003).
“A neurodynamic test is considered to be positive if the following criteria are fulfilled: a patient’s symptoms are reproducible, there are side differences, and the symptoms are increased by the use of structural differentiation” (Apelby-Albrecht., 2013, p. 627). It doesn’t ever say that the full range of movement is required for these tests to be positive so please be gentle with your radiculopathy patients and don’t stress them too much.
To differentiate from CTS and ulnar nerve entrapment you can later assess the elbow and hand and perform peripheral neuropathy special tests such as the Tinel’s test at the wrist and elbow (Cardidi, et al., 2011).
consideration for assessment
1. Always keep in mind your differential diagnosis and other conditions to consider?
- CTS and entrapment neuropathies
- Thoracic outlet syndrome
- Shoulder injuries such as rotator cuff impingement
- Cervical spondylotic myelopathy
- Sinister pathology – malignancy (eg Pancoast but this isn’t the other tumour), cardiac pain, herpes
- Chronic regional pain syndrome (Corey & Comeau, 2014).
“The clinical overlap between cervical radiculopathy and peripheral nerve entrapment syndromes and their nearly ubiquitous nature makes understanding of and identification of these entities mandatory for all practitioners” (Caridi, et al., 2011, p. 265).
2. Keep in mind what each test is doing.
When looking at the cluster of tests above you will notice that some tests aim to reproduce the symptoms while other reduce them. Movements that reduce the foraminal space and lead to nerve compression often provoke pain for example; the Spurling test (lateral flexion and extension). While, cervical distraction and shoulder abduction (which reduce pressure) often alleviate pain.
3. Look for antalgic postures.
Sometimes we seen our patients sitting in unusual postures which they might say helps their pain. Often in the case of nerve root injuries this is trues and these postures are called antalgic postures. It is good to recognise them as it supports our hypothesis of radiculopathy but you can also question for them as easing positions. Below are two common positions that patients will adopt to alleviate their pain/discomfort, referred to as antalgic postures.
When to refer for imaging
XRAY is the first line of medical imaging generally used and this is not the first point of call. In fact, the diagnosis of cervical radiculopathy is largely clinical. AP and lateral views of the low cervical spine help to identify changes in cervical lordosis, osteophyte formation, neuroforaminal narrowing and appropriate levels.
If a patient fails conservative treatment and XRAY doesn’t reveal abnormality then MRI is the next line of treatment (Corey & Comeau, 2014). MRI helps to visual soft tissue structures and pathways of the nerve as it exists the foramen (Caridi, et al., 2011).
“In the absence of red flags suggesting infection or cancer or signs of myelopathy, it is reasonable to defer imaging and treat the patient’s pain with analgesics. MRI is indicated if substantial pain is still present four to six weeks after the initiation of treatment o if there are progressive neurological deficits.” (Cardette, Phill & Fehling, 2005, p. 398)
conclusion
Having looked at depth at the clinical presentation of cervical radiculopathy and the tests you may perform to confirm your diagnosis, the final blog will cover the multimodal treatment strategies suitable to use for this condition. Remember from the first blog, with neurogenic pain we need to consider both the health of the nerve and the movement of the nerve within its container. Keeping these two points in mind helps significantly to select the most appropriate treatments.
Sian :)
References
Apelby-Albrecht, M., Andersson, L., Kleiva, I. W., Kvåle, K., Skillgate, E., & Josephson, A. (2013). Concordance of upper limb neurodynamic tests with medical examination and magnetic resonance imaging in patients with cervical radiculopathy: a diagnostic cohort study. Journal of manipulative and physiological therapeutics, 36(9), 626-632.
Carette, S., & Fehlings, M. G. (2005). Cervical radiculopathy. New England Journal of Medicine, 353(4), 392-399.
Caridi, J. M., Pumberger, M., & Hughes, A. P. (2011). Cervical radiculopathy: a review. HSS journal, 7(3), 265-272.
Cheng, C. H., Tsai, L. C., Chung, H. C., Hsu, W. L., Wang, S. F., Wang, J. L., ... & Chien, A. (2015). Exercise training for non-operative and post-operative patient with cervical radiculopathy: a literature review. Journal of physical therapy science, 27(9), 3011.
Corey, D. L., & Comeau, D. (2014). Cervical radiculopathy. Medical Clinics of North America, 98(4), 791-799.
Kuijper, B., Tans, J. T. J., Schimsheimer, R. J., Van Der Kallen, B. F. W., Beelen, A., Nollet, F., & De Visser, M. (2009). Degenerative cervical radiculopathy: diagnosis and conservative treatment. A review. European Journal of Neurology, 16(1), 15-20.
Raney, N. H., Petersen, E. J., Smith, T. A., Cowan, J. E., Rendeiro, D. G., Deyle, G. D., & Childs, J. D. (2009). Development of a clinical prediction rule to identify patients with neck pain likely to benefit from cervical traction and exercise. European Spine Journal, 18(3), 382-391.
Wainner, R. S., Fritz, J. M., Irrgang, J. J., Boninger, M. L., Delitto, A., & Allison, S. (2003). Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy.Spine, 28(1), 52-62.
Waldrop, M. A. (2006). Diagnosis and treatment of cervical radiculopathy using a clinical prediction rule and a multimodal intervention approach: a case series. Journal of Orthopaedic & Sports Physical Therapy, 36(3), 152-159.