Injuries to the posterolateral corner of the knee
The posterolateral corner of the knee (PLC) is an inherently complex region both anatomically and functionally, and in recent times has been 're-discovered' for the role it plays in knee function and stability. In fact, the PLC of the knee has 28 seperate components, all of which play a vital role in both static and dynamic stability to prevent excessive hyperextension, tibial external rotation and varus angulation (LaPrade et al., 2014; LaPrade, Ly, Wentorf, & Engebretsen, 2003; LaPrade & Terry, 1997).
Injuries to the posterolateral corner (PLC) of the knee account for 16% of knee ligament injuries (LaPrade, Wentorf, Fritts, Gundry, & Hightower, 2007), and are often overlooked during diagnosis. A retrospective study showed that in 68 patients with PLC injuries, 72% were not correctly diagnosed at initial presentation, and the delay to correct diagnosis was on average 12 months. Perhaps this is due to the general lack of understanding of the role of the PLC and awareness of accurate assessment procedures (Pacheco, Ayre, & Bollen., 2011).
Clinically, posterolateral knee pain is very complex and often considered a diagnostic conundrum. Therefore the purpose of this blog is to explore the anatomy and biomechanics, and review the literature around diagnosis and management.
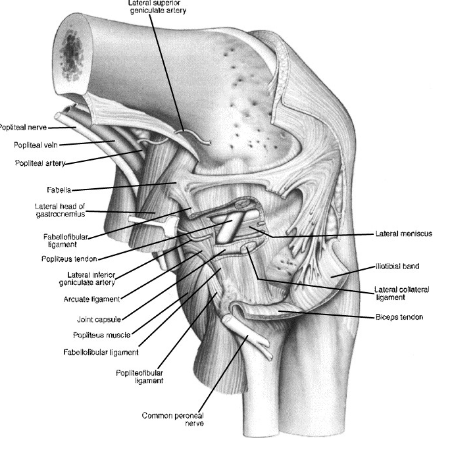
Image courtesy of Google Images, retrieved March 8th, 2016
PLC anatomy & Biomechanics
The PLC is especially important to the stability of the knee at angles of less than 45° knee flexion during weight bearing (Lunden et al., 2010).
The three most important stabilising structures of the PLC are the popliteus tendon, popliteofibular ligament and fibular collateral ligament (FCL)(LaPrade & Wentorf, 2002; Lunden et al., 2010).
- The popliteus tendon acts as a static and dynamic stabilizer against knee external rotation (LaPrade, Wozniczka, Stellmaker, & Wijdicks, 2010).
- The popliteofibular ligament assists with resisting varus stress and is considered the primary restraint for external rotation forces at the knee (Gollehon, Torzilli, & Warren, 1987; LaPrade & Wentorf, 2002). It is regarded a crucial stabilizer to the PLC and is typically surgically reconstructed when torn (Davies et al., 2004; Lunden et al., 2010).
- From 0-30 degrees knee flexion the primary static stabilizer to varus opening is the fibular collateral ligament (Sanchez, Sugalski, & LaPrade, 2006).
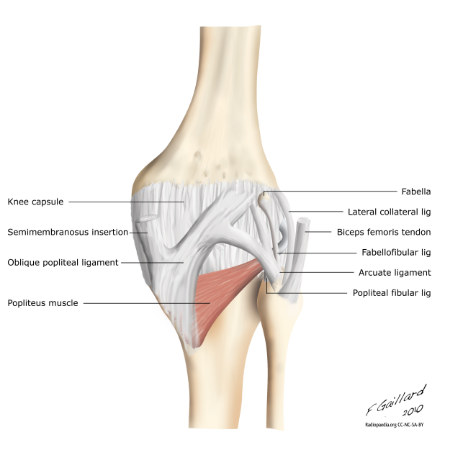
Other structures to consider are the posterolateral joint capsule, coronary ligament, oblique popliteal ligament and fabellofibular ligament also contribute to static stability of the PLC. Many of the static stabilizing ligaments are in fact a thickening of the capsule. The posterolateral joint capsule surrounds the knee like a blanket which the ligaments support (Lunden et al., 2010).
Image courtesy of Google Images, retrieved March 8th, 2016.
In addition to the primary static stabilisers there are numerous other dynamic stabilisers required for normal functioning of the knee. As mentioned above the popliteus complex contributes to both static and dynamic PLC stability. This is further enhanced by the lateral gastrocnemius tendon which blends with the posterior capsule and popliteofibular ligament. The iliotibial band (ITB) provides lateral knee stability in conjunction with the lateral capsule and ligaments to prevent varus in positions of knee extension. Finally the biceps femoris short and long head assist in knee flexion and lateral rotation, resist varus angulation and work synergistically with the rest of the hamstring complex to prevent excessive anterior translation of the tibiofemoral joint (Lunden et al., 2010).
Patient history & Clinical presentation
PLC injuries may present acutely or chronically, and often are accompanied with a mechanism of injury involving a fall, sports trauma or motor vehicle accident (Covey, 2001; Davies et al., 2004). Another strong MOI is knee hyperextension injuries, especially when the hyperextension mechanism is combined with varus forces to the knee (Baker, Norwood, & Hughston, 1983; Davies et al., 2004). Commonly, this is a result of a blow to the anteromedial aspect of the knee when the knee is close to full extension (LaPrade & Terry, 1997). It is not uncommon to have concurrent anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL) tears during this hyperextension mechanism. Injuries may be contact or non-contact and aside from hyperextension, can also originate from valgus force applied during knee flexion and severe tibial external rotation during knee flexion or extension (LaPrade & terry, 1997; Lunden et al., 2010).
Clinically, an acute PLC injury will present with swelling, pain in the posterolateral aspect of the knee and occasionally, numbness and weakness in the foot as a result of peroneal nerve disruption (Baker et al., 1983; Davies et al., 2004). Peroneal nerve injury can occur in up to 13% of injuries and should be carefully considered and screened for during assessment (LaPrade & Terry, 1997).
To expand on this further, numbness will be along the first dorsal web space and dorsum of the foot. Weakness in ankle dorsiflexion and eversion and great toe extension will be present and appear as a foot drop (Hughston & Jacobson, 1985).
Other clinical features may be a sensation of instability or giving way during weight bearing in extension during walking or on stairs.
Image courtesy of Google Images, retrieved March 8th 2016
Patient examination
Let's go through some of the aspects of physical examination pertinent to the diagnosis of a PLC injury.
1. Observation
Acutely injured knees will often have heat and swelling of the joint. Gait analysis should be routinely assessed and is useful in both chronic presentations and acute injuries, which will often have an antalgic gait. Pay careful attention to stance to determine if there is a varus thrust with or without hyperextension. This would be caused by a disruption to the lateral compartment structures resulting in an opening of this region. In some cases, patients may walk with a flexed knee to avoid stressing the joint and capsule in extension (Davies et al., 2004; Noyes & Barber-Westin, 1996).
2. Palpation
Accurate palpation is important to localise structures and assist in differential diagnosis. Acute PLC injuries will usually be tender to palpation over the posterolateral aspect of the knee joint and localised pain at the fibular head (Delee, Riley, & Rockwood, 1983; Lunden et al., 2010).
3. Special tests
Special tests for PLC injuries will include assessment of rotational and varus laxity at various degrees of flexion. There are multiple special tests used to assess for PLC injuries, however there is little evidence on their sensitivity/specificity. The following tests are considered by experts to be the most reliable for diagnosing injuries to the PLC and require skilled handling and interpretation (LaPrade & Wentorf, 2002).
- Anterior/posterior translation
- Posterolateral drawer test
- Dial test
- External rotation recuvartum test
- Varus stress test
The anterior/posterior translation test is performed at 30 and 90 degrees of knee flexion. You are looking for excessive posterior laxity at 30 degrees. If it is lax at both 30 and 90 degrees knee flexion, then a PCL injury should be suspected (Gollenhon et al., 1987). The ACL should be routinely tested with the Lachman’s test and pivot shift (Katz & Fingeroth, 1986; Wroble & Lindenfeld, 1988).
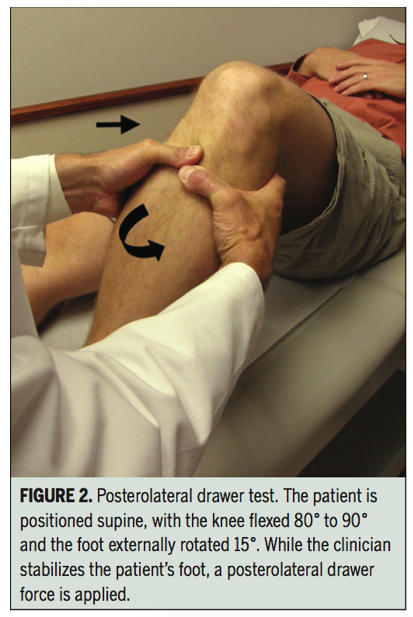
The posterior drawer test is performed in supine with the knee flexed to 80-90 degrees and the foot externally rotated to 15 degrees. A positive test is indicated by increased posterolateral rotation compared to the contralateral knee. The sensitivity and specificity of this test has not been reported.
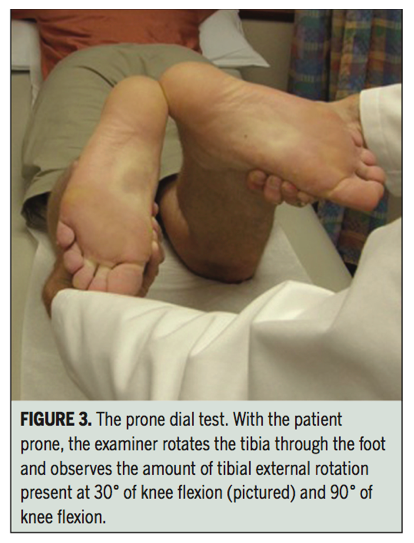
The dial test is performed in prone at 30 or 90 degrees flexion. The therapist externally rotates the tibia through the foot, comparing the range of external rotation between sides. A point to consider is that there is a wide variation of external rotation between knees. Therefore, an increase in 15 degrees or more on the injured side is considered pathological (Davies et al., 2004). If positive at 30 degrees, it is suggestive of a popliteus injury. If positive at both 30 & 90 degrees, it is suggestive of PLC and PCL injury (Lunder et al., 2010). Sensitivity and specificity values have not been reported however this test has been shown to have substantial agreement within and between testers (Jung, Lee, Jung, & Nam, 2009).
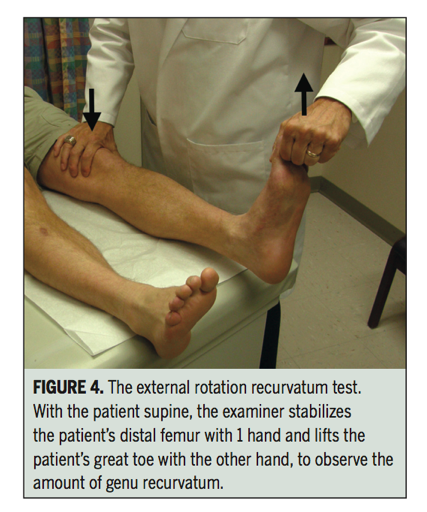
The external rotation recuvartum test is performed in supine. The therapist stabilises the distal thigh and lifts the leg into extension by holding the great toe. The amount of hyperextension is measured by the distance the heel lifts off the table and is compared with the contralateral side. This test has a sensitivity of 30% and specificity of 100% with a positive test usually occurring in the presence of a combined ACL and PLC injury, and is not isolated to PLC injuries (LaPrade, Ly, & Griffith, 2008).
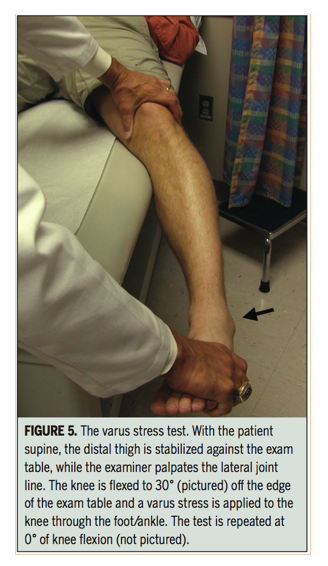
And finally, the varus stress test is performed in supine, with the proximal femur stabilised against the table and the knee flexed to 30 degrees. A varus stress is applied through the knee at the foot, while palpating the lateral joint line with the proximal hand. This is then repeated at 0 degrees. An increase in translation compared with the uninjured knee at 30° indicates a tear in the FCL. If there is increased joint opening at 0° the injury is more severe involving the capsule, popliteus tendon and FCL, however there is no data on sensitivity or specificity values.
Images below are of the posterolateral drawer test, prone dial test, external rotation recurvatum test and varus stress test (Lunden, et al., 2010). The tests outlined about are only part of a full knee examination and should be performed in conjunction with other special tests to rule out other causes of posterolateral knee pain.
Imaging
Due to the complex anatomy and close proximity of structures, imaging can assist in identifying specific anatomical structures injured, particularly in acute presentations where the physical examination may be equivocal due to pain and swelling. Magnetic resonance imaging (MRI) is the preferred modality however is operator dependent (Davies et al., 2004). LaPrade, Gilbert, Bollom, Wentorf, and Chaljub (2000) demonstrated that it is possible to identify the majority of individual structures in the PLC of the knee. Complete tears of two or more structures of the PLC is suggestive of instability (Morelli et al., 2013). Imaging can aid the clinician in making a diagnosis and should be used if severe PLC injury or concominant cruciate ligament injury is suspected. In chronic injuries it can be useful if conservative management is not improving symptoms.
Classification of injury
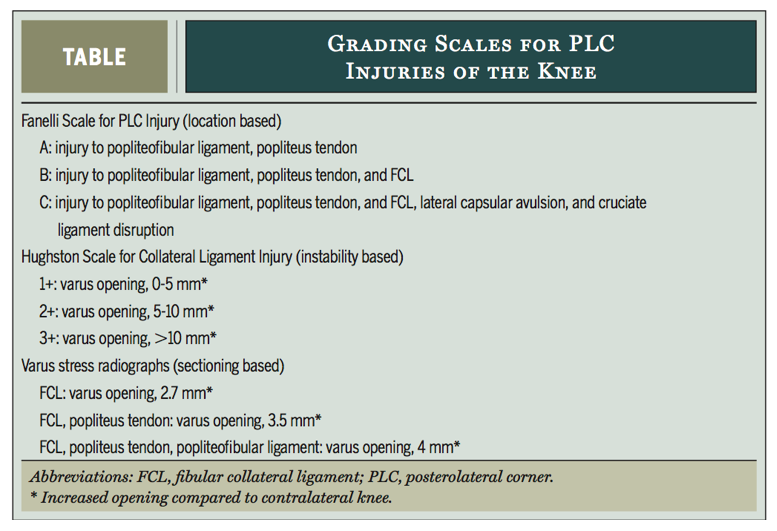
Classification of the severity of PLC injuries is important for directing clinical decision making, however it can be somewhat confusing as there are three classification systems used in the literature; the Fanelli scale, which is location based, the Hughston Scale, which is instability based, and Varus stress radiographs, which are sectioning based. The third classification system is a newer approach being used to assess chronic PLC injuries. Varus stress radiographs are taken with the knee at 20°. An increase of 4mm of lateral compartment gapping compared with the uninjured knee is considered a grade 3 injury (LaPrade, Heikes, et al., 2008).
Grading scales for PLC injuries of the knee (Lunden et al., 2010).
Treatment of PLC injuries
When an injury to the PLC has been detected it can be difficult in deciding which patients should have surgical reconstruction and who should attempt conservative management. Unfortunately, there is a lack of conclusive evidence and only small studies into the management of this population. Hughston grade 3 and Fanelli type C injuries to the PLC have been found to do poorly with non-operative treatment and have a negative effect on ACL reconstruction if left untreated (Dhillon, Akkina, Prabhakar, & Bali, 2012; Kannus, 1989; LaPrade & Terry, 1997).
A conservative approach can be effective and is warranted in less serious injuries. The recommended treatment for grade 1 to 2 PLC injuries is to immobilise the knee in a hinged brace locked in extension for 3-4 weeks and keep the leg non-weight-bearing. After this period of immobilisation rehabilitation is commenced to restore range of motion, increase weight bearing and functional strength of the knee (LaPrade & Wentorf, 2002; Rue, Kilcoyne, Dickens, & Kluk, 2011). This is based on expert opinion as currently there are no randomised controlled trials comparing conservative treatment protocols.
Treatment of PLC injuries has proved challenging. In the past reconstructive procedures used were neither anatomically based or biomechanically validated. This has resulted in recurrent laxity and failures (LaPrade et al., 2014). The development of new anatomically based reconstructive techniques have improved the outcomes of surgery and posterolateral knee stability (LaPrade, Johansen, et al., 2010). Grade 3 PLC injuries should be managed within the first 12 weeks of injury. Acute repair within two weeks of injury is considered to be superior than reconstruction at a later stage. However due to the high frequency of missed diagnosis (Pacheco et al., 2011) it is unlikely those who are suitable will be referred in time. Hence a greater appreciation and ability to diagnose PLC injuries can improve outcomes if managed timely and appropriately.
Despite the surgical literature advocating surgery for treatment of isolated grade 3 injuries, there are no randomised controlled trials suggesting that this results in best outcomes. Acute repair is claimed to be more successful than a delayed reconstruction however there is no high quality evidence supporting this claim. The literature does report good outcomes of acute repair in case series and case reports (Delee et al., 1983; Pavlovich & Nafarrate, 2002). Surgical treatment of chronic instability and symptoms associated with PLC injury is supported by evidence in large series of 95 patients with good results in 80% of cases (Hughston & Jacobson, 1985).
Injuries to the PLC are very commonly associated with injury to the ACL, PCL or both (Fanelli & Larson, 2002; LaPrade & Wentorf, 2002). Where concominant injuries exist it is advisable to seek an orthopaedic opinion (Davies et al., 2004). It is current practice to repair both areas due to the possibility of cruciate graft rupture.
In conclusion
In summary, this blog has explored the aspects of clinical examination that can help improve accuracy of diagnosis, as well as the role of MRI and reviewed the literature surrounding efficacy of surgical and conservative treatment options. During the initial stages of examination, careful questioning of mechanism of injury and symptoms helps to direct the assessment of posterolateral knee pain. Currently, the literature is difficult to assess due to the lack of standardisation, particularly regarding classification and reconstruction techniques. There is a scarcity of level one evidence making conclusions on best management problematic. Protocols for advanced conservative management have yet to be developed.
This is Grant's fourth contribution to Rayner & Smale. He has provided such interesting and well-research topics to discuss and learn about. We are all driven and passionate to learn about different facets of our profession and through sharing of information, our knowledge base grows. So thank you Grant for sharing your knowledge and learning experience with us.
Sian
References
Baker, C., Norwood, L., & Hughston, J. (1983). Acute posterolateral rotatory instability of the knee. The Journal of Bone & Joint Surgery, 65(5), 614-618.
Covey, D. C. (2001). Injuries of the posterolateral corner of the knee. The Journal of Bone & Joint Surgery, 83(1), 106-106.
Davies, H., Unwin, A., & Aichroth, P. (2004). The posterolateral corner of the knee: anatomy, biomechanics and management of injuries. Injury, 35(1), 68-75.
Delee, J. C., Riley, M. B., & Rockwood, C. A. (1983). Acute posterolateral rotatory instability of the knee. The American journal of sports medicine, 11(4), 199-207.
Dhillon, M., Akkina, N., Prabhakar, S., & Bali, K. (2012). Evaluation of outcomes in conservatively managed concomitant Type A and B posterolateral corner injuries in ACL deficient patients undergoing ACL reconstruction. The Knee, 19(6), 769-772.
Fanelli, G. C., & Feldmann, D. D. (1999). Management of combined anteriorcruciate ligament/posterior cruciate ligament/posterolateral complex injuries of the knee. Operative Techniques in Sports Medicine, 7(3), 143-149.
Fanelli, G. C., & Larson, R. V. (2002). Practical management of posterolateral instability of the knee. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 18(2), 1-8.
Gollehon, D. L., Torzilli, P., & Warren, R. (1987). The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. The Journal of Bone & Joint Surgery, 69(2), 233-242.
Hughston, J. C., Andrews, J., Cross, M., & Moschi, A. (1976). Part II. The lateral compartment. J. Bone Jt Surg. A, 58, 173-179.
Hughston, J. C., & Jacobson, K. (1985). Chronic posterolateral rotatory instability of the knee. J Bone Joint Surg Am, 67(3), 351-359.
Hughston, J. C., & Norwood Jr, L. A. (1980). The posterolateral drawer test and external rotational recurvatum test for posterolateral rotatory instability of the knee. Clinical Orthopaedics and related research, 147, 82-87.
Jung, Y.-B., Lee, Y. S., Jung, H.-J., & Nam, C.-H. (2009). Evaluation of posterolateral rotatory knee instability using the dial test according to tibial positioning. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 25(3), 257-261.
Kannus, P. (1989). Nonoperative treatment of grade II and III sprains of the lateral ligament compartment of the knee. The American journal of sports medicine, 17(1), 83-88.
Katz, J. W., & Fingeroth, R. J. (1986). The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries. The American journal of sports medicine, 14(1), 88-91.
Krukhaug, Y., Mølster, A., Rodt, A., & Strand, T. (1998). Lateral ligament injuries of the knee. Knee Surgery, Sports Traumatology, Arthroscopy, 6(1), 21-25.
LaPrade, R. F., Gilbert, T. J., Bollom, T. S., Wentorf, F., & Chaljub, G. (2000). The Magnetic Resonance Imaging Appearance of Individual Structures of the Posterolateral Knee A Prospective Study of Normal Knees and Knees with Surgically Verified Grade III Injuries. The American journal of sports medicine, 28(2), 191-199.
LaPrade, R. F., Griffith, C. J., Coobs, B. R., Geeslin, A. G., Johansen, S., & Engebretsen, L. (2014). Improving outcomes for posterolateral knee injuries. Journal of Orthopaedic Research, 32(4), 485-491.
LaPrade, R. F., Heikes, C., Bakker, A. J., & Jakobsen, R. B. (2008). The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuriesAn in vitro biomechanical study. The Journal of Bone & Joint Surgery, 90(10), 2069-2076.
LaPrade, R. F., Johansen, S., Agel, J., Risberg, M. A., Moksnes, H., & Engebretsen, L. (2010). Outcomes of an anatomic posterolateral knee reconstruction. The Journal of Bone & Joint Surgery, 92(1), 16-22.
LaPrade, R. F., Ly, T. V., & Griffith, C. (2008). The External Rotation Recurvatum Test Revisited Reevaluation of the Sagittal Plane Tibiofemoral Relationship. The American journal of sports medicine, 36(4), 709-712.
LaPrade, R. F., Ly, T. V., Wentorf, F. A., & Engebretsen, L. (2003). The Posterolateral Attachments of the Knee A Qualitative and Quantitative Morphologic Analysis of the Fibular Collateral Ligament, Popliteus Tendon, Popliteofibular Ligament, and Lateral Gastrocnemius Tendon*. The American journal of sports medicine, 31(6), 854-860.
LaPrade, R. F., & Terry, G. C. (1997). Injuries to the posterolateral aspect of the knee Association of anatomic injury patterns with clinical instability. The American journal of sports medicine, 25(4), 433-438.
LaPrade, R. F., & Wentorf, F. (2002). Diagnosis and treatment of posterolateral knee injuries. Clinical Orthopaedics and related research, 402, 110-121.
LaPrade, R. F., Wentorf, F. A., Fritts, H., Gundry, C., & Hightower, C. D. (2007). A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 23(12), 1341-1347.
LaPrade, R. F., Wozniczka, J. K., Stellmaker, M. P., & Wijdicks, C. A. (2010). Analysis of the Static Function of the Popliteus Tendon and Evaluation of an Anatomic Reconstruction The “Fifth Ligament” of the Knee. The American journal of sports medicine, 38(3), 543-549.
Lunden, J. B., Bzdusek, P. J., Monson, J. K., Malcomson, K. W., & Laprade, R. F. (2010). Current concepts in the recognition and treatment of posterolateral corner injuries of the knee. journal of orthopaedic & sports physical therapy, 40(8), 502-516.
Morelli, V., Bright, C., & Fields, A. (2013). Ligamentous Injuries of the Knee: Anterior Cruciate, Medial Collateral, Posterior Cruciate, and Posterolateral Corner Injuries. Primary Care: Clinics in Office Practice, 40(2), 335-356.
Noyes, F. R., & Barber-Westin, S. D. (1996). Treatment of complex injuries involving the posterior cruciate and posterolateral ligaments of the knee. The American journal of knee surgery, 9(4), 200.
Pacheco, R., Ayre, C., & Bollen, S. (2011). Posterolateral corner injuries of the knee A SERIOUS INJURY COMMONLY MISSED. Journal of Bone & Joint Surgery, British Volume, 93(2), 194-197.
Pavlovich, R. I., & Nafarrate, E. B. (2002). Trivalent reconstruction for posterolateral and lateral knee instability. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 18(1), 1-3.
Rue, C. J.-P., Kilcoyne, C. K., Dickens, C. J., & Kluk, C. M. (2011). Diagnosis and Treatment of Injuries to the Posterolateral Ligament Complex. Journal of Knee Surgery, 24(3), 143.
Sanchez, A. R., Sugalski, M. T., & LaPrade, R. F. (2006). Anatomy and biomechanics of the lateral side of the knee. Sports medicine and arthroscopy review, 14(1), 2-11.
Wroble, R. R., & Lindenfeld, T. N. (1988). The Stabilized Lachrnan Test. Clinical Orthopaedics and related research, 237, 209-212.