Hip: Post Hip Arthroscopy Rehab Phase 3 & 4
Welcome back to the second blog discussing rehabilitation following hip arthroscopy. If you missed part 1, you can catch up on what was discussed here.
Before looking at the remaining phases of rehabilitation I wanted to take a moment to recognise a Melbourne Physiotherapy-led specific rehab trial known as the FAIR trial. This trial focusses specifically on retraining the deep hip rotators, the quadratus femoris, obturator internus and gemelli. It has greatly impacted how I approach hip rehabilitation and offers a step-by-step program and I haven't seen this work published in such detail else where. The reason I feel these exercises are so valuable is because they directly target the deep rotators which lie in close proximity to the acetabulum and hip joint and have significant potential to control the position and movement of the hip. In phase I & II many protocols suggest clams, bridges, side lying abduction, hip extension exercise etc, which are all great hip exercises for global control of movement, however none are specifically addressing deep hip rotation.
The exercises and descriptions can be found here in further detail. They begin with isometric contractions, progress through active range of movement through to resisted and then functional exercises. Clinically what I have found is that patients learn much more about the positioning of their hip and where muscle activity is coming from when these exercises are included in their rehab. For example, the exercise below demonstrates a later progress of resisted hip external rotation in kneeling. This exercise involves aspects of weight bearing, centring of the femoral head, positioning of pelvic tilting and the patient can use their hands to palpate their hip to determine which muscles (hamstrings, TFL, deep hip rotators etc.) are performing the movement. For me, these exercises are the missing piece in hip rehab protocols and I hope that future programs will see these exercises taught with more emphasis beginning in phase I with isometrics.
Phase 3
Phase III is the functional phase where exercises are progressed towards a more life-focussed and sport-focused direction. You can begin this phase when PROM is symmetrical and painfree and gait is normal with no trendelenburg sign. There still should be no pain as movement and strength improves. You can begin stretching into end of range, use a wheelie stool to allow PROM activities in an upright and partial weight bearing position.
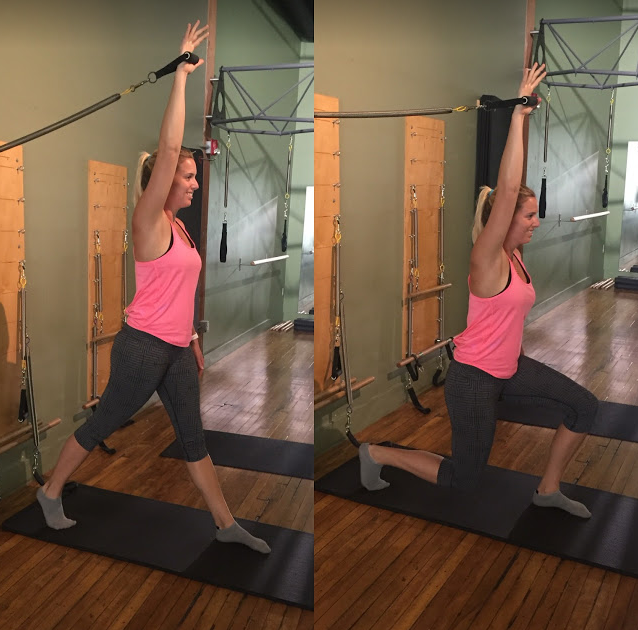
All ADLs are performed at a premorbid level and cardio is progressed to 30 minutes of low to moderate intensity. By the end of phase III patients are beginning to do some running and progressing into agility and plyometric work and targeting strengthening exercises to the sport to which the patient wants to return. Phase III usually sits from 2-3 months. Below are examples of exercises I've read included in phase III.
When can patient's return to running?
This wasn't clearly defined in any paper I read, however you can use similar criteria to other injury rehab programs which may include: good eccentric control of lowering into a squat, single leg step down and landing from a hop, strength >4/5 in hip manual muscle testing, asymptomatic pool running and no flare ups post activity.
Progression from phase III-IV when:
- No asymmetry with ADLS and recreational activity,
- Passing sport-specific performance tests,
- Demonstrates proprioceptive and neuromuscular control and symmetry. Aiming for hip muscle strength >90% of the uninvolved side.
- What you will notice is the criteria start to become less specific and will depend on the requirements and goals of each patient (Grzybowski, et al., 2015) .
Phase 4
By 4 months most programs have merged into Phase IV, the return to sport phase, meaning the program is functionally specific to the patient. You can progress to phase IV when they demonstrate mastery of harder strength exercises, have symmetrical painfree ROM, normalised gait and tolerance of low impact aerobic exercise (Spencer-Garner et al., 2014).
They have begun practice/training, continue to build cardio and strength and build on balance, proprioception, agility, plyometrics and dynamic movements. During this phase you need to consider training step ups, lateral step ups, squats, deadlifts and lunges to develop strength. “Although both evidence based and empirical clearing tests for return to sport exist, it is important to note that regardless of the pathology, a competitive person will never feel completely recovered until they can consistently and painlessly repeat the movement responsible for the mechanism of injury” (Edelstein, et al., 2012, p. 21).
These criteria for progression between phases are summarised from the systematic review by Grzybowski et al (2015), which explored the diversity of hip rehabilitation from 18 studies. Below are some of the exercises that will continue into Phase IV. Even though sport-specific training is occurring, strength and control needs to be maintained.
Progression from phase 4 to phase 5 (unrestricted sport) when:
- Painfree in a competitive state,
- Passing all return to sport tests,
- Dynamic functional control,
- Physical clearance for fitness,
- Full practice without restriction and without pain.
Phase 5
Phase V isn’t described in many programs but refers to the phase in rehabilitation where the patient returns to unrestricted play without any issues. As phase IV is sport-specific you need to achieve mobility, strength and balance for normal life before entering this phase and realistically “it is not uncommon for return to pre operative activity levels to approach six months post operatively” (Spencer-Garner et al., 2014).
In phase IV the goals are:
- Return to full activity and sport.
- Demonstrate measures for vertical leap, hop for distance and three hop for distance that are within 90% of the value of the uninvolved side (Spencer-Garner et al., 2014).
- You should also aim to have addressed biomechanical issues that were pre-existing and ensure that no movement pattern dysfunctions carry back into sport/activity.
Realistically these five phases will take around 6 months to complete and prior to having the surgery, patients may find this a daunting process. If you take the time to carefully explain the steps involved I am sure their perspective will shift as they realise how much work is going to be required to reach phase V in 6 months.
Remember, there are so many exercises that we can choose to incorporate within each phase of recovery and it should reflect a dynamic and progressive process. The question is not what exercise to include, but more so how are we teaching them and how is the patient performing them. Being specific about exercise performance is the key to getting the most out of rehab. The last thing you want is for the patient to punch through endless repetitions with poor quality of movement and reinforce old movement patterns and muscle recruitment patterns that will land up causing inappropriate load through their hip again. Below are some links to previous blogs that I've written, which might be of interest to read about the specificity of gluteal exercises and hip rehabilitation.
- Exercises that target the gluteal muscles over TFL.
- Making functional exercises more specific.
- Turning down TFL.
- Training without hip flexor overload.
SUMMARY
Research continues to state that strong evidence is still lacking and this comes back to study design, heterogenity of subjects and the generalisability to other hip pain diagnoses and surgical procedures. As no two patients are the same, it continues to be difficult to design high quality trials to assess the efficacy of rehabilitation. We do know that it is a very important part of recovery. We also know that Physiotherapists are incredibly well positioned to take the lead in this area.
As there is no clear criteria for selecting the ideal surgical candidate, therapists need to rely on their assessment and clinical reasoning to make the most informed decision. Unfortunately, I felt there was a distinct lack of discussion about assessment and the reasoning behind selection of exercises. What I fear is that this might cause the reader/therapist to prescribe exercises from protocols without a sound base of clinical assessment and without developing a strong list of objective asterisks to measure change. So my hope is that these blogs have highlighted the key criteria for each phase of rehabilitation and where assessment can be done to monitor change and progress.
Here are a few key points that I took away on this topic in regards to the entire process:
- In the first phase protection is important to allow for biological healing. Don't rush to exit this phase and ensure you communicate with the surgeon to understand what procedure was performed and how long phase I should be.
- When try to prevent adhesions circumduction of the hip is a great movement to use in PROM exercises.
- Take care to educate patients about flexion loads in the hope of avoiding a hip flexor tendinopathy.
- Use the iHOT-33 to measure and document patient-reported outcomes.
- Hip rehabilitation is not a linear process and should not follow a time-driven program.
- Try not to change multiple variables in a single session.
- Aim to continue rehab to phase IV and work to develop a maintenance program.
The exercises from the FAIR trial have significantly impacted my approach to hip rehabilitation in general, not just post surgical, and I would encourage you to consider incorporating these exercises into your approach.
Sian :)
REFERENCES:
Alessandro, A., Marco, G., Francesco, P., & Alessandro, M. (2015). Rehabilitation after Hip Arthroscopy. J Orthop Res Physiother, 1(001).
Bennell, K. L., O’Donnell, J. M., Takla, A., Spiers, L. N., Hunter, D. J., Staples, M., & Hinman, R. S. (2014). Efficacy of a physiotherapy rehabilitation program for individuals undergoing arthroscopic management of femoroacetabular impingement–the FAIR trial: a randomised controlled trial protocol. BMC musculoskeletal disorders, 15(1), 1.
Edelstein, J., Ranawat, A., Enseki, K. R., Yun, R. J., & Draovitch, P. (2012). Post-operative guidelines following hip arthroscopy. Current reviews in musculoskeletal medicine, 5(1), 15-23.
Enseki, K. R., Martin, R. L., Draovitch, P., Kelly, B. T., Philippon, M. J., & Schenker, M. L. (2006). The hip joint: arthroscopic procedures and postoperative rehabilitation. Journal of Orthopaedic & Sports Physical Therapy, 36(7), 516-525.
Garrison, J. C., Osler, M. T., & Singleton, S. B. (2007). Rehabilitation after arthroscopy of an acetabular labral tear. N Am J Sports Phys Ther, 2(4), 241-50.
Grzybowski, J. S., Malloy, P., Stegemann, C., Bush-Joseph, C., Harris, J. D., & Nho, S. J. (2015). Rehabilitation following hip arthroscopy–a systematic review. Frontiers in surgery, 2, 21.
Spencer-Gardner, L., Eischen, J. J., Levy, B. A., Sierra, R. J., Engasser, W. M., & Krych, A. J. (2014). A comprehensive five-phase rehabilitation programme after hip arthroscopy for femoroacetabular impingement. Knee Surgery, Sports Traumatology, Arthroscopy, 22(4), 848-859.
Stalzer, S., Wahoff, M., Scanlan, M., & Draovitch, P. (2005). Rehabilitation after hip arthroscopy. Operative Techniques in Orthopaedics, 15(3), 280-289.
Tijssen, M., van Cingel, R. E. H., Staal, J. B., Teerenstra, S., de Visser, E., & Nijhuis-van der Sanden, M. W. G. (2016). Physical therapy aimed at self-management versus usual care physical therapy after hip arthroscopy for femoroacetabular impingement: study protocol for a randomized controlled trial. Trials, 17(1), 1.
Waho M, Dischiavi S, Hodge J, Pharez JD. (2014) Rehabilitation after labral repair and femoroacetabular decompression: criteria-based progression through the return to sport phase. Int J Sports Phys Ther 9: 813-826.