Are we underestimating the importance of sleep?
Sleep is a function of the brain and a behaviour vital to the survival of all mammals. There is no single region of the brain, single neurotransmitter, or single neural pathway that is dedicated to sleep and wakefulness. States of sleep and wakefulness are generated by complex interactions between multiple neurotransmitters and neuromodulators. Recently I completed an online course through University of Michigan on Sleep: Neurobiology, Medicine and Society. It was such a well run course hosted through Coursera. I learnt so much about the importance of sleep, how sleep works and it made me think one thing over and over again “How closely does sleep relate to chronic pain disorders?”
I didn’t know a lot about sleep before taking the course. Aside from it being one of my favourite past times, I realised that throughout University and further education, I had been taught little about sleep hygiene, what are normal and abnormal sleep behaviours, how sleep works in the brain, and how medications can impact sleep. These topics are what I wish to share with you. The purpose of writing these next few blogs is not to provide an evidence-based review on sleep and pain. The purpose is to explore the questions that I began to think of while studying this course about the close interaction between pain states and sleep disorders. It’s a collation of notes and ideas from the past three months.
I’m starting to wonder if we are completely underestimating the importance of quality sleep, or at least not doing enough to improve it with our patients?
History
One of the first things to note about sleep science, neurobiology and medicine, is that it is a very young and developing field of research. As technology evolves and our ability to study the active and sleeping human brain improves, our understanding of sleep expands. Previously however, we relied heavily on the information gained from animal studies. Luckily sleep follows similar states and traits in all mammals.
In early research sleep was thought to be an afferent process caused by withdrawal of sensory input. Scientists thought sleep was a passive process. In one study scientists surgically cut part of the brainstem in a rat to test this hypothesis and realised that even without sensory input, animals still fluctuate in and out of sleep (but not a normal sleep). At this time scientists discovered that within the brainstem is a mechanism which generates arousal. So the hypothesis of sleep was changed from a passive process to the hypothesis of ascending reticular activating system (ARAS), meaning that arousal doesn’t depend on sensory input as originally thought.
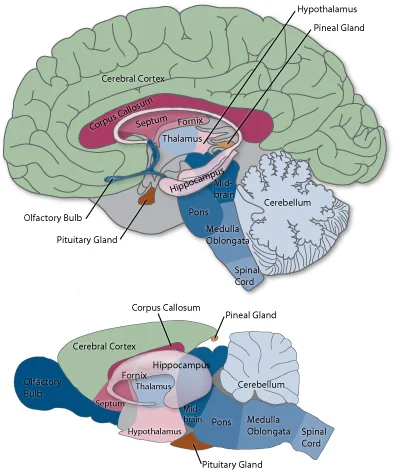
After finding the different functional regions of the brainstem (the pons, medulla and midbrain) and how they relate to sleep, scientists continued on to investigate the role of the forebrain (basal forebrain) and hypothalamus (anterior, posterior and lateral hypothalamic regions). It became a big point of focus in the early 1900s when an epidemic swept through Europe killing millions of people. It was called Encephalitis Lethargica, a viral infection of the brain causing initial headache and drowsiness that lead to coma. First described in 1917 by Neurologist Constantin von Economo and Pathologist Jean-Rene Cruchet. After post-morton brain analysis they discovered lesions in the pre-optic areas and anterior hypothalamus. People with lesions in the the pre-optic area and anterior hypothalamus died from a coma and they realised that these regions are the sleep centres and the posterior hypothalamus is the wake centre. They tested their theory on rats and found that when the pre-optic area is stimulated, animals fall asleep.
Around 1957, scientists then discovered that large amounts of brain activity occurring at particular times of sleep. This is when REM sleep was discovered along with the discovery of dreaming. Next came the discovery of the part of the brainstem that controls REM sleep. In 1962, Jouvet found that REM sleep is generated in the rostral pontine region or pons. During REM sleep parts of the brain are as active as they are during waking but the main difference between REM sleep and waking is the regions of the brain that are active. One particular difference in regional specificity is the activity of the prefrontal cortex, which during waking is involved in our decision making, and during sleep, is non-functional. Perhaps this explains why we make such poor decisions in our dreams?
After reading and learning about the history of sleep science I realised two things: that sleep science is still a very new element of medicine, and that the regions of the brain involved in sleep seem functionally very similar to those involved in pain processing. It made me wonder what cross over exists between sleep disorders and chronic pain? It was made me wonder what impact pain medications have on sleep and if this is a negative one? And if so, then the body might not have the best opportunity to recover and regenerate? To answer these questions we need to explore the neurotransmitters and functional regions of the brain involved in sleep and how medication impacts these regions.
What drugs come to mind when the term chronic pain is discussed? Tricyclic antidepressants (TCAS), Selective serotonin reuptake inhibitors (SSRIs), Opiods, Benzodiazapines, and Neuropathic medication such as Gabapentin and Pregabalin.
So let me ask this…. How often do you take careful note of the exact pain medication and dosage a patient is taking? How often do you question about quality of sleep or daytime sleepiness? How often do you question about how long it takes to fall asleep (sleep latency). Do we actually know enough about people’s sleep behaviours to make a decision whether their sleep is adequate or being affected by medication?
Medications
All central nervous system drugs affect sleep.
Tricyclic antidepressants (TCAs) (Endep) have an anti-cholinergic action which improves REM latency and can result in mood improvements. Alzheimer’s disease is treated with acetylcholine esterase i.e. an acetylcholine agonist in the forebrain to assist with memory. Drugs which promote acetylcholine promote REM sleep. TCAs are used to treat depressive disorders, mood disorders and anxiety disorders, but have largely been replaced with SSRIs, SNRIs and NRIs.
Selective serotonin reuptake inhibitors (SSRIs) are used to treat major depressive disorders and mood disorders. Their action is to increase extracellular serotonin levels, which are neurotransmitters that promote wakefulness amoung other things
Opiod medication is a mainstay analgesic prescribed from severe pain. Commonly prescribed opiods included Codeine, Fentanyl, Morphine, Mathadone, Oxycodone, and Tramadol. Addiction and tolerance are not as much a problem with Opiods as liver and renal dysfunction and lowered respiratory rate. The maximum dosage per day is 100mg/day. Side effects include drowsiness, confusion, mood changes, hallucinations, constipation, nausea, vomiting, reduced respiratory rate, urinary retention, and increased risk of falls.
Neuropathic medication is used to treat neuropathic pain i.e. when the nerve is damaged, as neuropathic pain is generally non-responsive to opiod medications. Neuropathic medications include TCAs, anticonvulsants, NMDA antagonists. Benzodiazepines have been prescribed as sedatives, hypnotics, anti-convulsants and muscle relaxants. They act on GABAa receptors. More recently benzodiazepines have been replaced with drugs such as Gabapentin (Neurotin) and Pregabalin (Lyrica) which treat neuropathic pain by acting on calcium channels rather than GABA receptors.
Opiods and Neuropathic medications cause drowsiness while TCAs and SSRIs promote wakefulness. All these pain medications have an impact on sleep. No CNS acting drug doesn’t impact sleep.
Neurotransmitters and cell locations
I hope to write a separate blog that looks in closer detail about the action and location of the main neurotransmitters involved in sleep. For now, this is a summary of the very complex sleep centres and wake centres.
Main neurotransmitters involved in sleep:
- Serotonin 5-HT
- Norepinephrine NE
- Histamine HA
- Acetylcholine Ach
- GABA
- Orexin/ Hypocretin HCRT
- Adenosine
Cell locations:
- Dorsal raphe nucleus DR
- Locus coerulus LC
- Posterior hypothalamus PH
- Anterior hypothalamus AH
- Lateral hypothalamus LH
- Pontine reticular formation PRF/Pons
- Basal forebrain BF
- Tuberomammillary nucleus TMN
- Laterodorsal tegmental area LDT
- Substansia nigra SN
- Ventrolateral pre-optic area VLPO
- Pre-optic nucleus PON
- Median pre-optic nucleus MPN
Some interesting facts I learnt about sleep.
- Reading books and attending lectures doesn’t make you sleepy. You become aware of your sleepiness because you are bored. You will only be sleepy when bored if you are sleep deprived.
- Everyone needs 7-8 hours of sleep per night. If you can’t get it then napping during the day to make up time is allowed (unless you already struggle with falling asleep at night).
The less you sleep, the more sensitive to pain you are.
The less REM sleep you get, the more sensitive to pain you are.
- If we look at the table above we see that Acetylcholine is an important promoter of REM sleep. If someone is on a drug that is to help their pain but actual is an anti-cholinergic drug, then it will inhibit REM sleep and make them more susceptible to pain sensitivity.
There are only four causes of excessive daytime sleepiness:
- Poor sleep at night and poor sleep hygiene.
- CNS disease
- CNS acting drugs
- Abnormal circadian rhythm.
- One good indicator of whether or not you are getting enough sleep is if you choose to sleep later on the weekend.
- Sleeping only 4 hours a night puts your BAC at 0.05% after one drink because being tired enhances the effect of alcohol.
- 3 nights of 4 hours sleep reduces your tolerance to sugar to the point you are pre-diabetic.
Sleep deprivation causes weight gain through reduced metabolism. Sleep deprivation increases blood pressure and cortisol levels. Sleep deprivation reduces your ability to determine when you need to eat therefore the more you sleep well, the less hungry you will feel.
- Alcohol disrupts the circadian rhythm so avoid drinking it close to going to bed.
- Caffeine reduces adenosine levels – a neurotransmitter we need to initiate sleep – so avoid it 4-6 hours before sleep.
- Try to wind down 30 minutes before going to sleep. White light interrupts the natural circadian rhythm and therefore working in the bedroom prior to going to sleep is going to disrupt your ability to fall asleep.
- Don’t fight bedtime – when you feel sleepy go to sleep. This is natural. If you fight it you wake up the circadian rhythm and you wake yourself back up.
Consequences of sleep loss.
Behavioural: sleepiness, cognitive impairment, increased risk of accidents, increased risk taking behaviours, reduced work productivity, reduced quality of life, reduced memory, reduced learning, increased stimulant seeking behaviours, altered interaction with alcohol, altered mood, and reduced awareness.
Physiological: hypoxemia, insulin resistance, weight gain, increased sympathetic activity, reduced arousal, reduced antibody production, and increased pain sensitivity.
Hopefully now you can see a few reasons why I think we might be underestimating the importance of quality sleep. The following blogs will look more closely at the functional neuroanatomy of sleep and pain as well as the clinical assessment and management of common sleep disorders.
Sian