Painful Plica - do they exist?
WHEN I FOUND MY FIRST PLICA
That heading makes it sound like a precious jewel... haha... well for me learning about plicas was learning a precious piece of information about a rare condition.
It was 2010 and my husband was a few months post his first ACL reconstruction. He sustained a lovely 'knee explosion' landing from a high vertical jump at volleyball. Having played competitive elite volleyball since the 14 of age, his training and biomechanics were not to blame for the injury. Simply, he jumped excessively high and landed on a straight leg. He tore his ACL, MCL, LCL, medial meniscus and sustained tibial plateau fractures. Typical to many ACL injuries, the crowd heard it 'snap'. I was in my first year out of University and honestly, a little scared to take on his rehab and juggle all the healing timeframes and rehab goals for all these structures. So he completed his Physiotherapy and rehab with Mr. Darren Ross, Musculoskeletal Physiotherapist and Partner at Physica Spinal and Physiotherapy Clinic.
His first surgery was a hamstring graft. Within the first two weeks following surgery his hamstring ruptured leaving him with a permanent hole in the back of his leg the size of my fist. This is a rare adverse event following an ACL reconstruction.
Otherwise, he was recovering very well and meeting all the goals after the surgery. We went to a beach house for a week of sun and sand, and spent hours each day walking along the beach. It was lovely... until one day he tells me he has this severe pain on the inside of his knee and he can't bend it under load i.e. can't walk, can't go up/down stairs, can't sit to stand. I tried everything I knew to assess his knee thinking it might be his patellofemoral joint and yet nothing I did even reproduced his symptoms. I couldn't even find them?? With both of us worried, we returned to see his Physiotherapist. Within minutes, Darren has found the source of the problem. "It's a painful Plica" he tells me and I replied "A what?".
Having only seen a few painful plicas during my years of practice, I believe it to be a rare cause of knee pain but what I've realised is that many people don't even know it exists. Yet in all the musculoskeletal and sports physiotherapy textbooks we are encouraged to consider the plica as a source of anteromedial knee pain in our differential diagnosis. This blog is a review of the anatomy and clinical presentation of the painful plica syndrome.
The medial plica was first mentioned in 1555 by Vesalius and was named at that time the ligament mucosum (Dupont, 1994, p. 5). What we know now is that the synovial plicas are remnants from embryonic development. The knee cavity is formed during weeks 9-12 of embryonic development and residual tissue forms a synovial plica in 90% of healthy knees (Kan, Arai, et al., 2015; Smallman, et al., 2015).
The plica were largely ignored until the 1960s, when arthroscopic techniques developed. In 1994 Dupont opened the paper Synovial plicae of the knee with the statement "the concept of the symptomatic synovial plica is controversial" (1994, p. 5) and this statement continues to be repeated throughout the literature today as little agreement exists about the classification, prevalence and presentation of the painful plica. Never the less - should you diagnose a symptomatic plica in a patient with anteromedial knee pain - treatment strategies are required.
What is a Plica?
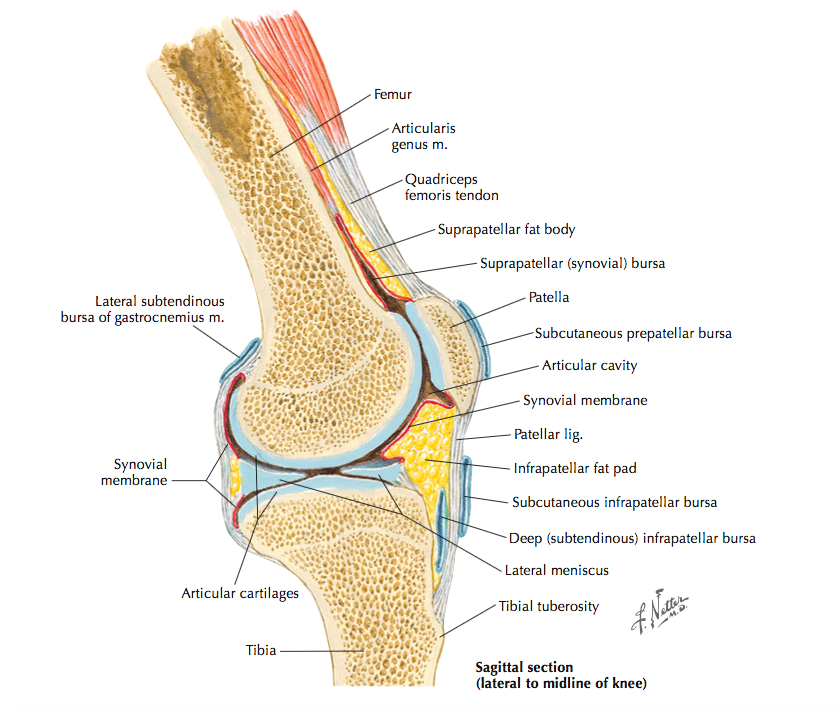
Image courtesy of Google Images
There are four reported plica that exist around the knee: superior, medial, lateral and infrapatella. The most commonly symptomatic plica is the medial plica which extends from the medial joint line to the infrapatella fat pad.
The medial plica is often thought of as an intrarticular ligament, providing a mechanical link between the femoral condyle and the infrapatella fat pad (Smallman, et al., 2012). The medial plica undergoes distortion at end of range knee flexion and extension and is relatively lax during mid ranges and due to its attachment to the fat pad, places a tensile load and distorts this structure. When the plica is released arthroscopically, less fat pad distortion occurs during active and passive knee range of movement (Smallman, et al., 2012). A thorough differential diagnosis is required to ascertain if the plica is the primary cause of knee pain.
Axial graphic shows a thickened and elongated medial parapatellar plica interposed between the patella and trochlea. The plica undergoes repetitive trauma in this location. (Andrew Sonin, StatDx, retrieved August 24th, 2015)
Axial PDWI FS MR shows a thick, irregular, and undulating medial parapatellar plica extending deep into the trochlear notch, and interposed between the medial trochlea and patella. Such plicae can become inflamed and thickened due to repetitive trauma during knee motion, setting up a vicious cycle of trauma and inflammation. (Andrew Sonin, StatDx, retrieved August 24th, 2015)
How does it present?
It has been reported that the medial plica exist in 64-85% of healthy knees (Kan, Arai, et al., 2015) and it may be symptomatic in 2.8% of cases of knee pain (Williams, Lloyd, et al, 2015).
When symptomatic local symptoms include:
- Anteromedial knee pain in 75% of cases,
- Clicking in 50% of cases,
- Tenderness on palpation,
- Reduced knee range of movement in 8% of cases
- And difficulty with loading tasks (Kan, Arai, et al., 2015).
As you can see from this list, these symptoms are not particularly specific to plica syndromes and can present with many other causes of knee pain.
Why does it become painful?
Plica become symptomatic following mechanical injury, trauma or overload (Kan, Arai, et al., 2015). Like many other smaller structures in the body, tibialis posterior compared to calf, TFL compared to gluteals, the Plica becomes painful when it's placed under too much load and the primary muscles controlling that movement are deficient and poor biomechanics occurs.
From my experience, a painful Plica is very common after knee arthroscope but not usually right away. It's more common when people start ramping up their activity levels and don't that the gluteal, hamstring, quadricep and calf control for the task at hand. There are uncontrolled rotatory forces at the knee loading up structures. It can also become painful, inflammed, thickened from the arthroscopic insertion if there is scar tissue formation after that.
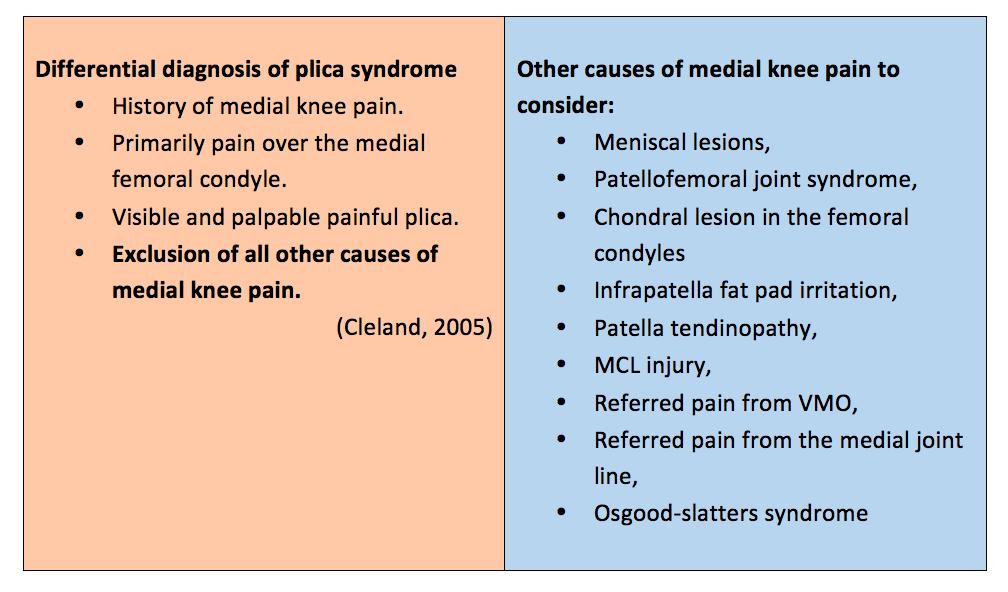
How do we differentiate it from other causes of medial knee pain?
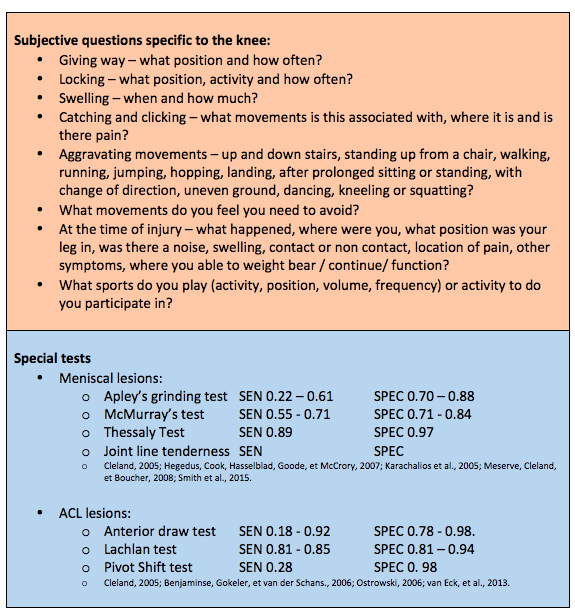
What I hoped you might take away form the story at the start is that Painful Plica Syndrome is a diagnosis of exclusion, like most conditions names as 'syndromes'. Clearly my husband had sustained injury to several structures around and in his knee and I didn't know initially how to differentiate one from another. It is difficult to rely on clinical examination alone and usually patients require MRI, arthrography, dynamic U/S or CT scan to assist with differential diagnosis (Williams, Lloyd, et al., 2015). Below is an outline of the special questions involved in the subjective assessment to help differentiate causes on knee pain as well as the sensitivity and specificity of some of our special tests for the knee. There are few special tests specific to the plica that have been validated to date.
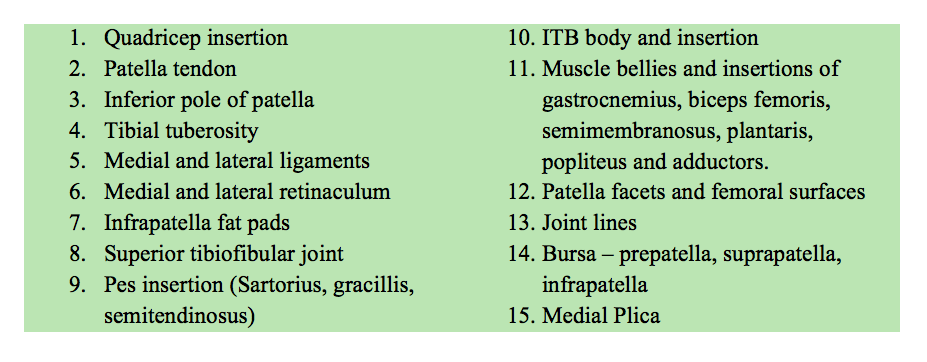
For me, palpation is the best way to localise where the pain is coming from.
In those that a symptomatic plica is present, you can feel it as a thickened band running diagonally and about 1.5 cm long. When you flick over it, it feels thick and sometimes swollen, and reproduces the patient's pain. There are a lot of different structures that need to be palpated too in the differential diagnosis of anteromedial knee pain.
Gold standard for diagnosis
It currently remains that the gold standard for diagnosis is arthroscopic examination but there is no clear consensus about arthroscopic appearance nor clear guidelines for when a surgical resection may occur (Morelli & Braxton, 2013; Shetty, et al., 2007; Williams, et al., 2015). Surgery is generally indicated after 6-8 weeks of conservative treatment has failed, pain and clicking is present and all other possible causes of knee pain are excluded (Dupont, 1994; Kan et al., 2015; Williams, et al., 2015). I feel this is quite a vague guideline.
Many studies use the Sakakibara classification to describe what type of plica is present (but each article I read this in described it slightly differently)(Dupont, 1994; Kan et al., 2015; Hashi et al., 2013; Shetty et al., 2007):
- Type A: cord-like elevation in the synovial wall under the medial retinaculum (1.8%).
- Type B: shelf-like appearance but does not cover the anterior surface of the medial femoral condyle and does not impingement on the medial femoral condyle (15.8%).
- Type C: large shelf-like appearance which covers the anterior surface of the medial femoral condyle (73.7%).
- Type D: double insertion into the medial wall (8.8%).
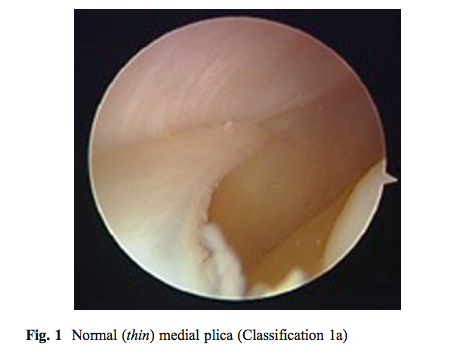
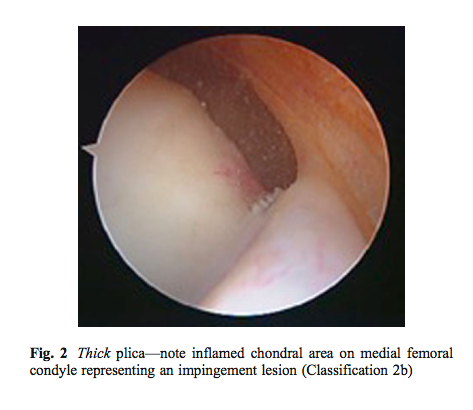
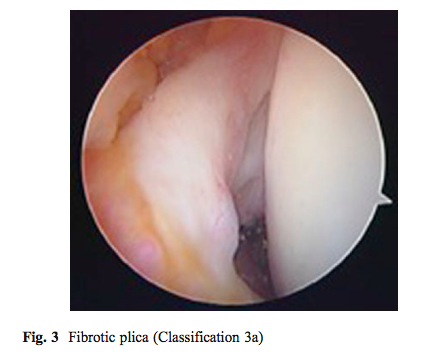
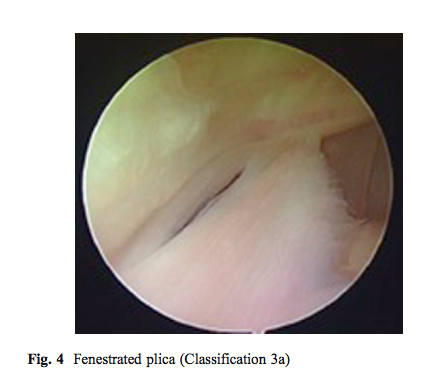
As you can see this classification describes the shape and size of the plica, not the presence of pathology. Williams et al (2015) described a different classification which involved three components; the presence of plica as Type 1a (thin), 2a (thickened but not inflammed) and 3a (fibrotic and fenestrated).
One of the risks of using arthroscopic examination is the over-eagerness to surgically resect the plica on a basis of "just in case" philopsophy. Unfortunately this may lead to "adverse effects of haemarthrosis, joint stiffness and iatrogenic lateral patella subluxation" (Williams, et al., 2015, p. 46).
Kan & colleuges (2015) hypothesised that medial synovial plica symptoms would be associated with cartilate damage (measured on the International Cartilage Research Society classification ICRS). Interestingly that found that there was no association between plica and bone marrow lesions. Type c & D were more highly associated with cartilage damage and cartilage damage was found in 29.8% of knees (Kan et al., 2015).
Medical imaging
The best medical imaging for visualising the plica are MRI and dynamic US.
On MRI you can look for thickening in the plica, subchondral bone changes in the medial femoral condyle, joint effusion, and chondral thickening. All of which may be possible causes of anteromedial knee pain. Hayashi and collegues (2013) examined the frequency of MRI-detected medial synovial plica at the knee and performed a cross-sectional association with MRI detected cartilage damage and bone marrow lesions. Again there was no associated between plica and bone marrow lesions. In this study type A and B were more highly associated with medial patella cartilage damage. But how does MRI findings correlate with the Sakakibara classification?
- MRI type 1 = Type A
- MRI type 2 = Type B
- MRI type 3 = Type C
- Nothing for Type D
One of the benefits of MRI is the ability to clearly grade degrees of cartilage damage (Hayashi et al., 2013):
- 0 = normal thickness
- 1 = focal swelling of cartilage without thickness loss
- 2.0 = partial-thickness focal defect < 1 cm in greatest width
- 2.5 = full-thickness focal defect <1 cm in greatest width
- 3 = multiple areas of partial-thickness (grade 2.0) defects intermixed with areas of normal thickness, or a grade 2.0 defect wider than 1 cm but <75% of the region
- 4 = diffuse (≥75% of the region) partial-thickness loss
- 5 = multiple areas of full- thickness loss (grade 2.5) or a grade 2.5 lesion wider than 1 cm but <75% of the region
- 6 = diffuse (≥75% of the region)
The diagnostic accuracy of an arthroscope is 91.7% with a sensitivity of 100% (Shetty et al., 2007). Dynamic ultrasound has a diagnostic accuracy of 88%, sensitivity of 90% and specificity of 83% (Paczesny et al., 2009). Unfortunately I don't have comparative scores for MRI but it's normally pretty high when compared to US and arthroscope for other injuries.
Dynamic ultrasound is performed in supine with the leg extended and quadriceps relaxed. Symptomatic plica is confirmed in all of the following criteria are met (Paczesny et al., 2009):
- Presence of continuous echo sliding of the medial femoral condyle which confirms the presence of the medial plica but not that it is pathological.
- Determine if there is contact between the plica and the patella.
- If there is pain or discomfort during the examination.
How is it treated?
Conservative treatment generally involves rest, limiting aggravating factors, addressing biomechanical issues, NSAIDS and cryotherapy (Morelli & Braxton., 2013). Not often do I find a plica being the only problem at someones knee - so treatment is a combined approach. For the Plica specifically though - I've found gentle soft tissue release and continuous ultrasound to be helping in reducing pain on palpation. Ice cube massage can provide a focal treatment as well as using gladwrap (plastic wrap you cover food with) to seal off a 10c clump of anti-inflammatory gel.
The plica should definitely be considered as a source of anteromedial knee pain with patients who report pain under load, clicking and difficulty with loading tasks of knee flexion. Performing a thorough assessment of the knee takes time as each structure has a battery of special tests. Don't be discouraged though and use special questions during the subjective assessment to gain a strong hypothesis of what you suspect might be the problem. Although it is not a common condition, the painful plica does exist and we have our clinical examination as well as medical imaging and arthroscopic interventions to help assist our diagnosis and guide our treatment.
Sian
References
Benjaminse, A., Gokeler, A., & van der Schans, C. P. (2006). Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. Journal of Orthopaedic and Sports Physical Therapy, 36(5), 267-288.
Çalpur, O., Tan, L., Gürbüz, H., Moralar, Ü., Copuroğlu, C., & Özcan, M. (2002). Arthroscopic mediopatellar plicaectomy and lateral retinacular release in mechanical patellofemoral disorders. Knee Surgery, Sports Traumatology, Arthroscopy, 10(3), 177-183.
Cleland, J. A., & Koppenhaver, S. (2011). Netter's Orthopaedic Clinical Examination: An Evidence-Based Approach (2nd ed.). Philadelphia, Pennsylvania: Saunders Elsevier.
Dupont, J. Y. (1994). Synovial plicae of the knee. The Knee, 1(1), 5-19.
Hayashi, D., Xu, L., Guermazi, A., Kwoh, C. K., Hannon, M. J., Jarraya, M., ... & Roemer, F. W. (2013). Prevalence of MRI-detected mediopatellar plica in subjects with knee pain and the association with MRI-detected patellofemoral cartilage damage and bone marrow lesions: data from the Joints On Glucosamine study. BMC musculoskeletal disorders, 14(1), 292.
Hegedus, E. J., Cook, C., Hasselblad, V., Goode, A., & McCrory, D. C. (2007). Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. Journal of Orthopaedic and Sports Physical Therapy, 37(9), 541-550.
Kan, H., Arai, Y., Nakagawa, S., Inoue, H., Hara, K., Minami, G., ... & Kubo, T. (2015). Characteristics of medial plica syndrome complicated with cartilage damage. International orthopaedics, 1-6.
Karachalios, T., Hantes, M., Zibis, A. H., Zachos, V., Karantanas, A. H., & Malizos, K. N. (2005). Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. The Journal of Bone and Joint Surgery, 87(5), 955-962.
Meserve, B. B., Cleland, J. A., & Boucher, T. R. (2008). A meta-analysis examining clinical test utilities for assessing meniscal injury. Clinical Rehabilitation, 22(2), 143-161.
Morelli, V., & Braxton, T. M. (2013). Meniscal, plica, patellar, and patellofemoral injuries of the knee: Updates, controversies and advancements. Primary Care: Clinics in Office Practice, 40(2), 357-382.
Muse, G. L., Grana, W. A., & Hollingsworth, S. (2010). Arthroscopic treatment of medial shelf syndrome. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 26(3), 391-392.
Ostrowski, J. A. (2006). Accuracy of 3 diagnostic tests for anterior cruciate ligament tears. Journal of Athletic Training, 41(1), 120-121.
Paczesny, Ł., & Kruczyński, J. (2009). Medial Plica Syndrome of the Knee: Diagnosis with Dynamic Sonography1. Radiology.
Shetty, V. D., Vowler, S. L., Krishnamurthy, S., & Halliday, A. E. (2007). Clinical diagnosis of medial plica syndrome of the knee: a prospective study. The journal of knee surgery, 20(4), 277-280.
Smallman, T. V., Race, A., & Ekroth, S. (2012). The mechanical link between the infrapatellar plica and the fat pad - role in the etiology of anterior knee pain. Journal of Bone & Joint Surgery, British Volume, 94(SUPP XXXVIII), 100-100.
Smallman, T., Shekitka, K., Mann, K., & Race, A. (2015). The Infrapatellar Plica-a New Intra-Articular Ligament of the Knee. The FASEB Journal, 29(1 Supplement), 545-3.
Smith, B. E., Thacker, D., Crewesmith, A., & Hall, M. (2015). Special tests for assessing meniscal tears within the knee: a systematic review and meta-analysis. Evidence-Based Medicine, 0(0), 1-10.
Schindler, O. S. (2014). ‘The Sneaky Plica’revisited: morphology, pathophysiology and treatment of synovial plicae of the knee. Knee Surgery, Sports Traumatology, Arthroscopy, 22(2), 247-262.
Strover, A. E., Rouholamin, E., Guirguis, N., & Behdad, H. (1991). An arthroscopic technique of demonstrating the pathomechanics of the suprapatellar plica. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 7(3), 308-310.
van Eck, C. F., van den Bekerom, M. P. J., Fu, F. H., Poolman, R. W., & Kerkhoffs, G. M. M. J. (2013). Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of physical examinations with and without anaesthesia. Knee Surgery, Sports Traumatology, Arthroscopy, 21(8), 1895-1903.
Williams, A. M., Lloyd, J. M., Watts, M. C., & Myers, P. T. (2012). The arthroscopic features of the pathological medial plica of the knee: a classification based on an analysis of 3,017 arthroscopies. European Orthopaedics and Traumatology, 3(1), 43-47.