Reducible discogenic low back pain
In a previous post on lumbar disc herniation with radiculopathy, I explored the clinical reasoning process I used over two treatment sessions for a patient with lower back and radicular leg pain.
In that case study, Sally presented with lower back and leg pain that was not reducible with flexion or extension mechanical loading strategies, but did respond well to lateral glides in standing. This too is a case study but the difference is in the reducible nature of the pain and the quick progression of treatment goals.
Patient introduction
Let me introduce Harry, a mid-twenties male who developed a sharp cramp-like pain in his lateral right calf and a shooting pain through his right buttock after a long flight.
Harry had a past history of left sided lumbar L5 disc herniation with radiculopathy 2 years prior and was managed with a microdiscetomy. His injury was left sided originally and fully recovered.
This was the first episode of right sided pain but followed the same distribution of pain as the previous one. You can imagine that for Harry, this was distressing knowing what experience he had originally and was worried that he was heading for another surgery.
How did it happen originally? Lifting boxes and helping a friend move house. This time? He was sick and coughing a lot and one night coughed in bed while in a slumped position and then next morning woke with the pain. [Both of these MOI are commonly associated with discogenic LBP.]
- He complained of only buttock and calf pain, nothing in his back and nothing through the back of his leg.
- It was aggravated with flexion, coughing, sit to stand and relaxing into a chair.
- His pain was alleviated with keeping his back straight.
- There was no P&N or N and the pain was intermittent.
Day 1 physical examination
- Right sided buttock and lateral calf pain (along the L5 distribution).
- Gr 5- right SLCR x 5 versus Gr 5+ on the left.
- SLR R1 30 deg and R2 45 bilaterally, no change with cervical flexion.
- Neuro exam: sensation, other MMT and reflexes in tact.
- Slight ipsilateral lumbar list – leg pain eased with correction to centre and exacerbated when increased (hips further to left).
- Lumbar flexion P1 knees with visible hypertonicity through the lumbar spine ES and a lack of the flexion relaxation response.
- Lumbar extension increased right sided buttock pain. R2 5 degrees.
- Nil top through the calf, hamstring or buttock.
- Right sided hypomobility R L45 L5S1 with associated muscle guarding. No reproduction of leg pain on palpation.
day 1 problem list & treatment strategies
- Education of the problem.
- Mechanisms of pain i.e. Radicular pain versus radiculopathy, acute pain versus chronic pain, nocicpetive vs. radicular vs. central pain.
- Triggering the pain neuromatrix i.e pain that is felt compared to actually tissue damage.
- MOI, distribution of symptoms, outcome of physical examination all as supporting evidence for the diagnosis of radicular pain.
- Management of aggravating factors such as sitting/ standing time.
- Importance of keeping moving.
- How the immune system is involved in inflammatory pain.
- Reduction of list with R sided hip gliding against the wall.
- Reduction of excessive muscle guarding with taping the lower back.
- Management of inflammation and pain with an explanation about appropriate medications and dosage. In this case the starting medication for pain relief was ibuprofen.
Looks pretty similar to the day 1 from the case of Sally. That’s because it was. Although the diagnosis may vary slightly, the physical impairments and problems for day 1 were very similar. There was a big difference between Sally and Harry though. Sally was fearful of the pain, while Harry was worried, he was more inquisitive about how it could be different to his previous injury and everything he could do to understand it more and manage it better.
Day 2 examination (3 days later)
- Harry was feeling better. His leg pain felt more like an ‘almost about to cramp’ than severe pain.
- The aggravating factors were still slumping into sitting, sit to stand, coughing and the easing factors were still keeping his back straight.
- Both the tape and ibuprofen were helpful.
- Harry asked “why am I doing side glides (which help) rather than bending backwards?”
- A: Because while the list remains, it might be more comfortable to move in a range which is more controlled. Bending backwards was when performed with a list reproduced his right buttock pain.
- A: Lower back injuries heal quickest through regular movement as movement promotes blood flow, circulation of healing chemicals and nutrition transfer. Not all movement is good and not all movement is bad. The challenge is to find a direction that allows you to move well and without provoking pain and still minimising stiffness.
- His list continued but was reduced.
- Right calf SCLR Gr 5+ (strength returned).
- SLR 45/45.
- Lx flex below knees – lack of flexion relaxation response. This was filmed and showed to Harry to help him understand what “keeping his back straight while bending forward” looked like.
- Q: Is that bad?
- A: Yes. There should be a normal flexion relaxation response seen in the back extensor muscles. Without this relaxation the back extensors continue to load the spine through flexion, which inturn increasing the load on your back.
- Q: Can I change that?
- A: Yes – with exercises that encourage muscle relaxation in postures that provide offloaded lumbar flexion and also don’t have the same motor pattern as bending forward so that these patterns can be taught correctly from the start.
- Q: Why do I have that?
- A: It is not entirely certain from current research into postural problems associated with back pain as to why some people have persistent protective patterns beyond injury and why some people return to moving normally. Either way, once the pain settles it is important to ensure that you learn to move more normally again to reduce the load on your back.
- Lumbar extension R2 10 degrees with R sided buttock pain, no calf pain.
- Palpation: hypomobility R PA L45 L5S1 with muscle spasm.
- Functional assessment of sit to stand technique:
- Observation: uses hands to brace, keeps back straight, holds breath and braces through abdominals.
day 2 Problem list & treatment strategies
When performing repeated extension in standing (REIS) use your hands to support your back. You can place your thumbs over a specific level if you wish to make the movement more localised.
- Muscle spasm persists, list persists, flexion and extension range improved but still limited by pain.
- Gr III R PAIVMS L45 L5S1 // spasm and stiffness easing, SLR ISQ, lx ext painfree 10 degrees, no list, lx flexion R2 mid shins P0
- Functional movement retraining.
- It increases lumbar loading to STS holding your breathe, tensing your abs and bracing through your arms.
- Try to sit up and down just like a squat // this was pain free.
- Mechanical loading strategies.
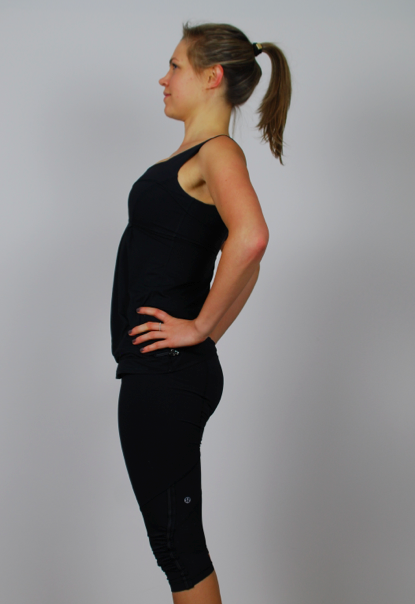
- Continue with side gliding exercises when it is applicable (see image above R).
- Add in repeated extension in standing and you can use your fingers to localise a particular level if you desire.
- Poor SLR range bilaterally
- Given hamstring sliders in supine as a starting point for increasing mobility. This completed in supine with the hip bent to 90 degrees and supported by holding behind the knee. The extend the knee/plantar flex the ankle, flex the knee/dorsiflex the ankle.
- Reduction of excessive muscle tone and restoration of the flexion relaxation response.
- Correction of apical breathing to basal and abdominal breathing.
- Flexion relaxation exercises (see series below, without the single leg hip flexion):
- Single leg hip flexion with breathing.
- Double leg hip flexion with breathing.
- 4PK childs pose rocking with breathing.
- Seated roll downs with breathing
- Standing roll downs with breathing.
- Please note this is the progression of positions that I use when retraining a flexion relaxation response and it often takes 6+ weeks to go through these postures. Most importantly, no patient is progressed to the next level until they are painfree in that position). For this particular patient he given hip flexion within 1-2 weeks post injury and progressed to 4PK rocking by week 3+.
- Re-application of tape to improve proprioception of slumping so that Harry didn’t have to move around with his back excessively straight all the time.
- Education about functional exercise:
- Its great to exercise as much as feels good.
- Where possible try to keep the movements functional which mean replicating daily tasks. An example of this is do squats, dead lifts and step ups over leg press and leg extension. Do push ups over bench press. Work on upper and lower body strength. Incorporate cardio into your program.
- Education about medication and list correction:
- Both of these are strategies I use for acute pain in the early days. Use them when you feel you are flaring up a bit or feeling stiff.
We chose right side gliding in standing (this image is in the left direction).




DAY 3 EXAMINATION (week 3)
- NSAIDS 4-5 tablets a day, tried to wean down but got sore again.
- Pain has shifted out of calf and more prominent in hamstring and buttock
- If coughing in sitting then sore, if standing ok. Sitting main agg.
- No post rx sorriness, felt much better after rx.
- Exercises going well, still feeling a bit skew
- Office chairs are too deep therefore not leaning back
Obj ax:
- No list.
- Flex P1 (buttock) at level of knees, then eases, R2 mid shins.
- Lx ext, LF and Rot all painfree to end of range with overpressure.
- SLR R1 45 deg R2 60 deg (with release of ankle DF)
- Not top R lx spine but stiff L5S1 centrally.
- Hip passive IR/ER L=R - just a quick screen of the hip, not a clearing test or full examination.
Day 3 problem list & treatment strategies
- Pain with flexion range of movement
- Gr III central PA caudal direction 3 x 60 sec // Lx flex improved quality and relaxation of Lx ES
- Lx rot PPIVMS with SLR RHS only // dec pain Lx flex, almost painfree
- Progression of home-exercise program 4PK child's pose, lumbar rotation combined with hamstring slider, and repeated extension in standing (all of which were painfree during treatment and resulted in less pain on lumbar flexion post treatment).
Day 4 exercises. Single leg lumbar rotation with active knee flexion/extension slider, double leg lumbar rotation in supine and child's pose.
Conclusion
The aim of this blog was to explore the way I use developed and progressed a treatment plan for a patient with reducible discogenic low back pain and leg pain. It was encouraging that each session required so much reassessment and progression and a beautiful tool for demonstrating improvement to Harry. How do we keep progressing forward and know when to change our treatment approach from manual to exercise, from offloading to loading, and what combination of treatments works best? It all comes from the assessment and reassessment. This is a great example of when back pain can be very severe and painful to start but also tolerate being pushed and recover quickly.
Thank you to Harry for allowing me to share his treatment path and exercise picture.
Sian :)