The role of the scapula in Shoulder Impingement Syndrome: part 2
Welcome back for the second part of the shoulder impingement syndrome series. The previous blog discussed the current definition of shoulder impingement and presented an algorithm for assessment. What you may have realised is that the assessment of the shoulder is incredibly complex and you cannot just rely on the impingement tests for your diagnosis. That is why we included the algorithm in the previous blog, which helps clinicians hypothesis what the main cause of shoulder pain might be. The scapula has a big role to play in many shoulder conditions, which leads us onto the next blog. This blog takes a closer look at normal biomechanics of the scapula and focusses on the finer details of assessment of the scapula.
Q: What is normal movement?
The scapula has 8 movements: elevation, depression, upward rotation, downward rotation, anterior tilt, posterior tilt, protraction and retraction.
During elevation the scapula needs to upwardly rotate, posteriorly tilt and internally or externally rotate depending on what position the arm moves into. For flexion the scapula will tend towards internal rotation and during abduction it will externally rotate (Ludewig & Braman, 2011). The clavicle will rotate posteriorly about 30 degrees, retract 15 degrees, and elevate 10 degrees during almost all shoulder planes of movement into elevation, except extension. The reason I’m mentioning movement of the clavicle is because positioning of the scapula is the end result of combined movement at the acromioclavicular joint and scapulothoracic joint.
One thing to bear in mind is that the degrees of movement are based on the ideal positioning of the scapula relative to the clavicle…. so if your patient has an abnormal resting posture to start with, these movements are going to be altered from the start!
One of the primary movements that we need to be able to observe, measure and rehabilitate is upward rotation of the scapula and this movement is pivotal in enabling full elevation and reach through the shoulder. Hence, many articles which measure scapula kinematics look primarily at the muscles involved in upward rotation; upper trapezius, lower trapezius and serratus anterior.
An American study (Phadke & Ludewig, 2013) compared muscle activation patterns and joint kinematics between individuals with impingement pain and asymptomatic shoulders during repeated unloaded and loaded shoulder elevation. What they found was that across both conditions in the painful subjects, there was increased activation of upper trapezius with lifting and early deactivation of serratus anterior on lowering. What this means is that when retraining upward rotation you may need to focus on timing and activation patterns of both the up and down phase of movement in order to retrain the movement accurately (Phadke & Ludewig, 2013).
As mentioned above there are many movements and muscles controlling the scapula and the shoulder complex. We cannot view the scapula as 8 seperate movements because it moves simultaneously about 3 axis of rotation and translates as well (Kibler, et al, 2002).
Image courtesy of Google Images (http://cardiovascularcausesofshoulderpa.weebly.com/uploads/1/2/5/6/12564003/1341679419.jpg) retrieved December 1st, 2015.
Q: What is the resting position of the Scapula?
It is important to observe the scapula, at rest and through movement, from the front and side. The resting position is typically observed with the patient’s arms are by their sides. The normal expected position of the scapula is:
- 10 degrees of upward rotation, 40 degrees of internal rotation, and 10 degrees anterior tilt (Struyf, et al., 2015).
- The spine of the scapula is aligned with T3, T4,
- Inferior angle of scapula aligned with T7, T8, T9 or even T10
- The medial border is parallel to the thoracic midline.
- The dominant scapula normally sits further laterally than the non dominant side, approximately 6cm from spine to the medial/lateral portions (Struyf, et al., 2014).
It might be useful to assess scapula position with arms by side, hands on hips, and in 90 degrees abduction to determine the static posture in each position prior to looking at the quality of movement through range (Struyf, et al., 2014).
Q: How does this change in Abduction?
- There should be 50-60 degrees of upward rotation and the scapula should shift inferiorly about 3-4 cm during 0-180 degrees of abduction.
- The scapula should posteriorly tilt 30 degrees and externally rotate 25 degrees, with the majority of movement occurring above 90 degrees.
- The inferior angle moves up and out approximately 8cm laterally and 3cm superiorly.
- The medial aspect of the spine of scapula moves down and out approximately 3cm inferiorly and 1.5cm laterally.
- The acromion moves up and in approximately 4cm superiorly and 3cm medially.
- There is a 2:1 ratio of movement between the glenohumeral joint and scapula known as scapulohumeral rhythm (McClure 2001; Bourne 2007; Watson, Pizzeria & Balster., 2010).
Q: How do we assess the scapula?
Looking above you will realise that there are many muscles and movements involved in overall scapular function and scapulohumeral rhythm. Which begs the question - should we be able to assess each one individually? In recent years many specialists have moved away from this individualised assessment as the science showed us that during each movement, no single muscle can be individually targeted and therefore a holistic assessment might provide greater insight.
The current gold standard for scapula assessment, based off information gained from the 2013 Scapula Summit, includes clinical observation, scapula assistance test and scapula retraction tests, not individual manual muscle testing (Kibler, et al., 2014). What does clinical observation actually mean?
- Visual observation of resting posture and static positions with hands on hips and 90 degrees abduction.
- 4-point palpation to confirm the resting position seen (I've previously explained this in detail in the thoracic outlet blog).
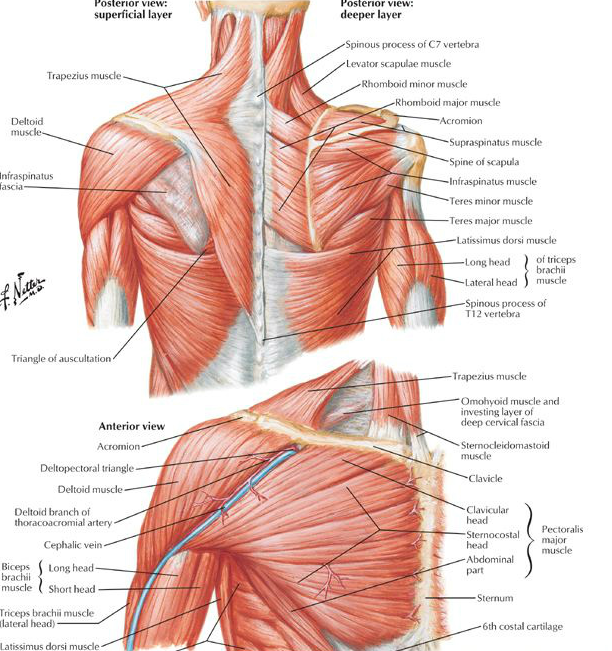
- Observe muscle bulk in the upper trapezius, supraspinous fossa, infraspinous fossa, levator scapula, rhomboids, middle and lower trapezius, posterior cuff, serratus anterior.
- Clavicular height, humeral head positioning and check for a sulcus sign.
- Observe the contribution to scapulohumeral rhythm through AROM - functional aggs, flexion, and abduction.
- When does the pain begin?
- What is the comparison in AROM and PROM and comparison from left to right?
- How are the muscles contributing to each range of movement, particularly in the painful posture?
- What happens when you manually correct scapula position?
- Scapula assistance test and scapula retraction test (Kibler, 2006).
Q: WHAT IS SCAPULA DYSKINESIS?
Scapula dyskinesis is a collective term which allows Physiotherapists to speak a common language. The term scapula dyskinesis describes alterations in scapula resting posture and movement, however it does not distinguish between types of scapula positions and movements (Kibler, et al., 2002).
The gold standard for scapula assessment in visual observation however, in the past little agreement existed about what practitioners see and how they define & interpret their observations (Kibler, et al., 2002). To enhance the reliability of assessment and provide clearer direction for treatment, further steps should be taken to define the predominant movement pattern seen (Kibler, et al., 2002). Kibler and colleagues (2002) conducted a study to understand what the more prominent patterns of scapula dyskinesis were.
Q: How do we interpret what we see?
So the first step in scapula assessment is observation of resting posture. Second step is to observe the scapula through active movements and decide:
Is scapula dyskinesis absent or present?
What type of scapula dyskinesis is present?
Type 1 - Infero-medial border prominence at rest, and during arm motion the inferior angle tilts dorsally and the acromion tilts forward over the top of the thorax.
Type 2 - Whole medial border prominence at rest and during arm movement the scapula tilts dorsally off the thoracic spine.
Type 3 - Supero-medial border prominence and the scapula can be displaced anteriorly and during movement the shoulder will shrug without winging.
Type 4 - The scapulae are symmetrical from left to right and move rhythmically and symmetrically during elevation.
The images below help to visually demonstrate each type of scapula dyskinesis (Kibler, et al., 2002, p. 551-552).
What effect does scapula repositioning or assistance have on the painful movement pattern?



Q: HOW DOES THIS RELATE TO SHOULDER IMPINGEMENT?
The mostly commonly observed deficits associated with impingement are:
- Reduced posterior tilt,
- Reduced upward rotation,
- Increased internal rotation,
- Increased clavicular elevation,
- Reduced serratus anterior activity, and
- Increased upper trapezius activity (Kibler, et al., 2002, p. 554; Ludewig & Reynolds, 2009; Ludewig & Braman, 2011; Phadke & Ludewig, 2013).
These movement aberrations may result in increased proximity between the rotator cuff tendons and surrounding structures. Additionally it has been noted that subjects with shoulder impingement will have increased superior or anterior humeral head translation, which may result in a reduction of the subacromial space (Ludewig & Braman, 2011).
- Increased protraction increases tension on the antero-inferior gleno-humeral ligaments.
- Altered scapula motion places increased demands on the rotator cuff muscles with reaching forward and reduces maximal rotator cuff muscle strength.
- Loss of posterior tilt is associated with impingement symptoms (Kibler, et al., 2002, p. 554).
It could be suggested that these changes occur due to pain inhibition, structural deficits such as tendon tears, soft tissue tightness, thoracic posture, muscle fatigue and altered motor control. This altered motor control changes the kinematics at the scapula, which plays a vital role in positioning and controlling the shoulder complex.
Scapula dyskinesis not only occurs in impingement but has also been seen in shoulder instability, rotator cuff disease and other conditions. Therefore the tips covered in this blog will be generalisable to scapula assessment and rehabilitation. Scapula dyskinesis is not a diagnosis but a label used to identify impairment in normal function of the shoulder complex.
Clinical tips
Visual observation goes beyond looking at the scapula and also includes looking at thoracic kyphosis and shoulder drooping. Bear in mind that the pattern is often more prominent during lowering because of the increase demands during eccentric activation of the muscles. While video-taping is helpful to record movement, it often only captures the movement from directly behind. It may be beneficial to view the movement from different positions to change your visual point of view.
It may be necessary to ask your patients to hold a small weight in their hand in order to accurately visual their control under load, particularly in stronger shoulders or patients who have higher physical/sporting demands. And remember…. what you might see is a mixed presentation with one type seen on lifting and another on lower the arm.
Studies often assess the scapula in flexion, scaption and abduction as the muscles activation patterns vary through these planes of movement. These studies often observe the scapula during repeated movements (at least 3) and at a rate of 45 degrees per a second i.e it will take four seconds to get to the top of elevation and 4 seconds to come down. So it is important to consider how fast do you ask your patients to move and how many times they repeat the movement.
Things to consider when you are assessing the scapula (Cools, et al., 2014; Kibler, et al., 2002):
- Scapula dyskinesis is not specific or indicative of one single pathology and often multiple pathologies can exist concurrently. The description is clinically useful but not diagnostically specific.
- Scapula dyskinesis is often a result of muscle imbalance and/or abnormal activation patterns.
- Scapula dyskinesis can be a result of pain inhibition and is an acquired adaptation independent of the specific diagnosis.
- The benefit of using these four categories described above is that it is relatively quick, doesn’t require equipment, is non invasive and helps clinicians speak a common language about what aberrant movements they are seeing.
- Regardless of the cause and effect relationship between pain and scapula dyskinesis, this abnormal scapula movement will jeopardise optimal shoulder function and therefore should be a focus in the treatment of shoulder pain and even neck pain.
- Scapula dyskinesis causes:
- Change in the transference of energy, production of force and equilibrium of the kinetic chain.
- Change in the the width of the subacromial space.
- Alteration in the fulcrum of the humeral head based on its position relative to the glenoid fossa.
- Compressive or shear forces on the cervical spine.
- Increased shear forces or reduced maximal strength of the rotator cuff muscles.
When trying to understand why scapula dyskinesis is occurring we need to consider both the muscles that might be weak or have poor activation patterns, but also consider what soft tissue structures might have deficits in flexibility (Cools, et al., 2014). Let's take a look at part 3: scapula rehabilitation programs and see how Physiotherapists such as Lyn Watson and Anne Cools approach exercise prescription.
Sian
References:
Cools, A. M., Cambier, D., & Witvrouw, E. E. (2008). Screening the athlete’s shoulder for impingement symptoms: a clinical reasoning algorithm for early detection of shoulder pathology. British journal of sports medicine, 42(8), 628-635.
Cools, A. M., Declercq, G., Cagnie, B., Cambier, D., & Witvrouw, E. (2008). Internal impingement in the tennis player: rehabilitation guidelines. British journal of sports medicine, 42(3), 165-171.
Cools, A. M., Witvrouw, E. E., Declercq, G. A., Vanderstraeten, G. G., & Cambier, D. C. (2004). Evaluation of isokinetic force production and associated muscle activity in the scapular rotators during a protraction-retraction movement in overhead athletes with impingement symptoms. British journal of sports medicine, 38(1), 64-68.
Ludewig, P. M., & Braman, J. P. (2011). Shoulder impingement: biomechanical considerations in rehabilitation. Manual therapy, 16(1), 33-39.
Kibler, W. B., & McMullen, J. (2003). Scapular dyskinesis and its relation to shoulder pain. Journal of the American Academy of Orthopaedic Surgeons,11(2), 142-151.
Kibler, W. B., Sciascia, A. D., Bak, K., Ebaugh, D., Ludewig, P., Kuhn, J., ... & Cote, M. (2013). Introduction to the second international conference on scapular dyskinesis in shoulder injury—the ‘Scapular summit’report of 2013. British journal of sports medicine, bjsports-2013.
Phadke, V., & Ludewig, P. M. (2013). Study of the scapular muscle latency and deactivation time in people with and without shoulder impingement. Journal of Electromyography and Kinesiology, 23(2), 469-475.
Struyf, F., Nijs, J., Mottram, S., Roussel, N. A., Cools, A. M., & Meeusen, R. (2014). Clinical assessment of the scapula: a review of the literature. British journal of sports medicine, 48(11), 883-890.
Watson, L. A., Pizzari, T., & Balster, S. (2010). Thoracic outlet syndrome part 2: conservative management of thoracic outlet. Manual therapy, 15(4), 305-314.
Watson, L., Balster, S. M., Finch, C., & Dalziel, R. (2005). Measurement of scapula upward rotation: a reliable clinical procedure. British journal of sports medicine, 39(9), 599-603.