Treatment of Achilles tendinopathy with combined loading programs
Introduction into Achilles tendinopathy
Achilles tendinopathy is an overuse injury characterized by dysfunction and local tendon pain with loading (Malliaras et al., 2013). Changes occur in tendon structure resulting in a tendon that is less capable of sustaining repeated load. Injury to the Achilles can severely impact upon everyday and recreational activities as it is one of the major locomotor tendons in the body (Malliaras, Barton, Reeves, & Langberg, 2013). It is more prevalent in sports that involve a large running component however occurs in all sports and at all levels of participation. Achilles tendinopathy has also been found in sedentary individuals (J. L. Cook, Khan, & Purdam, 2002).
Eccentric muscle strengthening has become the primary conservative management approach for Achilles tendinopathy and popularized by the Alfredson program, however up to 45% of patients do not respond to this approach (Alfredson, Pietilä, Jonsson, & Lorentzon, 1998; Malliaras et al., 2013). Other loading programs such as Silbernagel-combined loading program incorporates eccentric-concentric, eccentric and then faster loading (K Grävare Silbernagel, Thomee, Thomee, & Karlsson, 2001). This would seem a more logical approach to rehabilitation as functionally humans utilize the calf muscle in both a concentric and eccentric manner on a daily basis. To only re-train the eccentric portion of movement is effectively only re-training half of the legs function. Just to walk the gastrocnemius and soleus are required to act eccentrically in load absorption and then concentrically for forward propulsion. There are not many activities that would only require an eccentric calf contraction.
The purpose of this blog is to evaluate the Silbernagel loading program and its application in Achilles tendinopathy. The previous blog reviewed the continuum of tendon pathology and explained how tendinopathy occurs with overload and compression. Load is not a bad thing though and what you'll notice about this program and other Achilles tendinopathy treatment programs, is that load is what is used to help the injury heal.
Tendon and the response to load
Load is the primary stimulus that drives the tendon forwards or backwards along the continuum (J. Cook & Purdam, 2009). Exercise needs to be targeted and specific to the individual, depending where they sit on the continuum of tendon pathology. Administering an exercise program without sub classifying the stage of pathology may explain the conflicting and variable findings in the literature regarding different exercise approaches. For example an acute reactive tendon has the potential to revert to normal if the overload is adequately reduced or if there is ample time between loading sessions (J. Cook & Purdam, 2009). If load is not properly managed in this phase and further loading ensues, there is a high risk of pushing the pathology further down the scale into a state of dysrepair. Hence research which uses exercise as an intervention must ensure they classify which subgroup of tendinopathy they are trying to treat. Unfortunately, this is not always the case.
Load management and exercise can stimulate matrix structure, allowing for some reversibility of tendon dysrepair pathology (Öhberg, Lorentzon, & Alfredson, 2004). However, the Achilles tendon has been shown to remain thicker than normal for several years even after improvement in tendon structure and pain following an eccentric exercise program (Öhberg et al., 2004). Tendons with less severe pathology have a better clinical prognosis, therefore it is thought to be clinically beneficial to improve abnormal tendon pathology if at all possible (Malliaras, Purdam, Maffulli, & Cook, 2010). Training with maximum load eccentric contractions may be more likely to attain greater adaption (normalization) and remodelling within the tendon however this has only been shown in studies evaluating the patellar tendon (Malliaras et al., 2013). Nonetheless, this approach may be better suited to some patient sub-populations who are not irritable or have degenerative Achilles tendinopathy where maximum tendon adaption is desirable. Depending on sporting demands certain athletes may benefit from this approach too.
Achilles tendinopathy patients who present with significant concentric weakness need to receive specific rehabilitation exercises to address this deficit due to muscle contraction type specificity (Malliaras et al., 2013). Muscle training improvements are known to be specific to the joint angle, speed and type of contraction used in training (Morrissey, Harman, & Johnson, 1995). This group may not recover with isolated eccentric loading and require a combined eccentric-concentric approach to improve their strength deficits.
The Silbernagel- Combined Loading Treatment Protocol
Intensity and number of reps base on patient status. Start at 3 sets of maximum reps tolerated building up to 15 reps (Karin Grävare Silbernagel, Thomeé, Eriksson, & Karlsson, 2007; K Grävare Silbernagel et al., 2001).
Phase 1: Weeks 1-2
- Perform exercises once per day
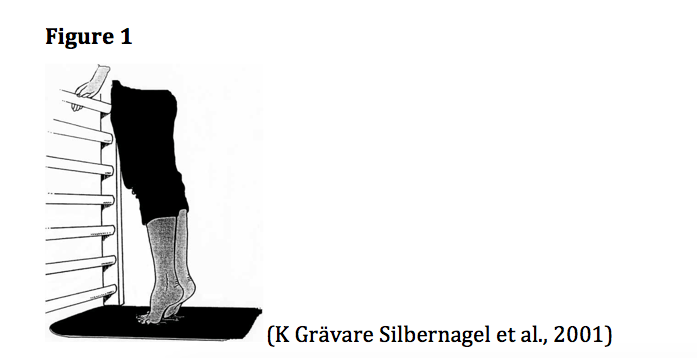
- Double leg calf raises standing on floor 3 x 10-15 (Figure 1)
- Single leg calf raise standing on floor 3 x 10
- Seated calf raise 3 x10
- Eccentric calf raise standing on floor 3 x10 (up on two feet, down on one) (Figure 2)
Phase 2: Weeks 2-5
- Perform exercises once per day
- Double leg calf raises standing on edge of step 3 x 15
- Single leg calf raise standing on edge of step 3 x 15
- Seated calf raise 3 x15
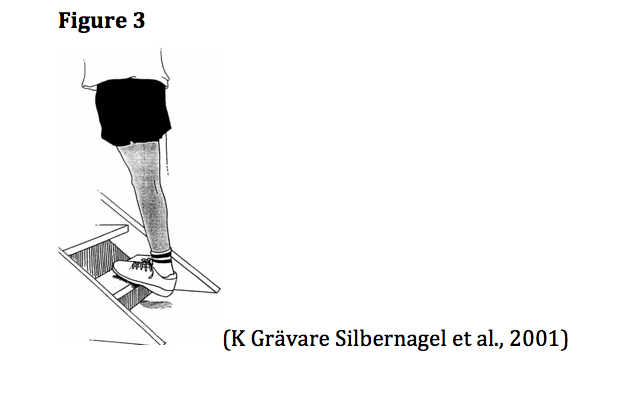
- Eccentric calf raise standing on edge of step 3 x 15 (up on two feet, down on one) (Figure 3)
- Quick-rebounding double leg calf raise 3 x 20 (do quick calf raises as if you are jumping without the toes leaving the floor. Turn back up when the heel is approximately 1cm from the floor)
Phase 3: Weeks 3-12 (longer if required)
- Exercise intensity can be increased by increasing the speed of loading or adding load using a backpack or weight machine.
- Perform exercises once per day and exercise with a heavier load 2-3 times/week
- Single leg calf raise standing on edge of step with added weight 3 x 15
- Seated calf raise 3 x15
- Eccentric calf raise standing on edge of step with added weight 3 x 15 (up on two feet, down on one)
- Quick-rebounding calf raise 3 x 20 (progress to single leg as able)
- Plyometric training- progression of this training is monitored by the treating physiotherapist. Incorporate jump rope skipping, hopping and jumping on/off small step/box. Movement must be controlled and explosive, build up to 3 x 20.
Phase 4: Week 12- 6 months (longer if required)
- Maintenance phase where patient has minimal symptoms and able to participate in sport without difficulty. Continue this phase until patient has no symptoms.
- Perform exercises 2-3 times/week
- Single leg calf raise standing on edge of step with added weight 3x 15
- Eccentric calf raise standing on edge of step with added weight 3x15 (up on two feet, down on one)
- Quick-rebounding calf raise 3x20
Jason Shane, from Shane Physiotherapy in British Columbia demonstrates the exercises in the Silbernagel protocol. Jason Shane, MPT, B.A., Functional Dry Needling/IMS graduated with a Masters Degree in Physical Therapy from the University of British Columbia (UBC). He has a special interest in orthopaedics and sports injury rehab by using a manual therapy and exercise-based approach to treatment. It's wonderful to see other like-minded Physiotherapists promoting this program for Achilles Tendinopathy and collaborating on the blog.
Evidence for eccentric tendon loading
The Alfredson eccentric loading program is a prevalent clinical treatment for Achilles tendinopathy however Malliaras et al. (2013) determined that there is limited evidence for its use when comparing it to other loading programs. There is evidence the Silbernagel-combined loading program results in superior outcomes compared to eccentric-concentric calf raises and stretching (K Grävare Silbernagel et al., 2001). It is important to note that there is a much evidence for the Silbernagel combined program as there is for the Alfredson eccentric approach when comparing to other loading interventions in Achilles tendinopathy (Malliaras et al., 2013). Pain and/or weakness may prevent some patients from being able to complete the Alfredson eccentric program, however the Silbernagel method allows for a gradual progression from eccentric-concentric to eccentric and then into faster loading which may be tolerated better by patients in the reactive/dysrepair stage. There is a lack of good quality evidence for Achilles tendinopathy although there is unequivocal benefit from loading interventions that utilize eccentric-concentric muscle contractions (Malliaras et al., 2013).
There is much debate and conflicting findings surrounding whether improved clinical outcomes are associated with a range of imaging measures. A high quality study by de Jonge et al. (2008) showed that improved clinical outcomes are not associated with the proportion of doppler signal within tendons and does not predict outcomes. Another high quality study demonstrated there to be no change in anteroposterior tendon diameter despite a reduction in symptoms (Rompe, Nafe, Furia, & Maffulli, 2007). Unfortunately ultrasound imaging is operator dependent and other low quality studies in the literature have reported conflicting findings which may also be due to a lack of adequately sub grouping tendon pathology (Malliaras et al., 2013). There is very limited and low quality evidence that improved clinical outcomes are associated with increased collagen (type 1) synthesis and reduced capillary blood flow within the Achilles tendon (Knobloch, 2007; Langberg et al., 2007). What this means is that often improvements seen clinically on functional testing and pain will no longer correlate with the medical imaging and this is ok. We can use outcome measures and other tests to continue to evaluate improvement and treatment effectiveness.
Eccentric and Silbernagel-combined tendon loading has been shown to improve neuromuscular function (peak torque and 1 rep maximum) (Alfredson et al., 1998; Karin Grävare Silbernagel et al., 2007; K Grävare Silbernagel et al., 2001). In healthy individuals eccentric loading has also been shown to yield greater muscle strength gains and hypertrophy than concentric loading, but not when the load is equalized (Roig et al., 2008). This indicates load intensity may in fact be the stimulus rather than the type of contraction. Therefore, eccentric training in tendinopathy might not result in greater neuromuscular improvements as load intensity is rarely maximized (Malliaras et al., 2013), perhaps due to pain and symptom irritability. However, there are other possible mechanisms where by eccentric muscle contractions may improve tendinopathy, but have received little research in this population. This includes greater neural changes (faster neural adaption), greater strength improvements in the contralateral limb and increased cortical excitability (Enoka, 1996; Hortobágyi et al., 1996).
The use of Outcome Measures
Pain is the key clinical feature that the physiotherapist seeks to alter, and pain response to treatment is a fundamental indicator of treatment success. Treatment progressions and outcomes will likely be more effective if pain levels and response to load are considered with the stage of pathology (J. Cook & Purdam, 2009). Optimal interventions are clinical treatments focused at inducing change in tendon structure and pathology, however as pain is the common clinical presentation, a case can be made for concentrating on pain reduction as a valid outcome measure (J. Cook & Purdam, 2009).
The literature evaluating intervention programs in Achilles tendinopathy commonly use both the VISA-A and visual analogue scale (VAS) pain scores as indicators of treatment effectiveness. These tools are not limited for use in research situations and can be used in the clinical setting to monitor patient progress. Due to the heterogenous nature of Achilles tendinopathy these tools may be useful to track if a patient is not responding to a particular exercise intervention and allow an alternative approach to be implemented promptly.
The Victorian Institute of Sport Assessment-Achilles (VISA-A) questionnaire is a disease-specific outcome measure with good reliability (Robinson et al., 2001). The VISA-A has good test-retest (r=0.93), interrater (r=0.9) and intrarater (r=0.9). The mean scores have been compared in patients with Achilles tendinopathy ranging in severity and with controls and demonstrated good construct validity (Robinson et al., 2001).
Conclusion
There is much more to tendon rehabilitation than purely using eccentric loading programs. To achieve maximum clinical effectiveness, exercise needs to be targeted to the individual, the stage of pathology and functional demands of the patient. Malliaras et al. (2013) concluded there to be little clinical evidence for isolating the eccentric component during Achilles tendon rehabilitation. Instead they propose eccentric-concentric loading should be used instead of or alongside eccentric training programs. Unfortunately there is a paucity of high quality studies and there remains alternative potential mechanisms of loading interventions yet to be investigated. This includes central nervous system changes and neural adaption. Unfortunately the literature rarely reports the severity and irritability of Achilles tendons, so the sample population may be at different points along the reactive-degenerative spectrum which will inherently impact the response to load (J. Cook & Purdam, 2009). This may explain the conflicting findings in the research. Assessment and modification of duration, frequency, intensity and type of load is paramount to successful treatment of Achilles tendinopathy (J. Cook & Purdam, 2009).
Grant Freckleton
References
Alfredson, H., Pietilä, T., Jonsson, P., & Lorentzon, R. (1998). Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. The American journal of sports medicine, 26(3), 360-366.
Benjamin, M. (2002). Tendons are dynamic structures that respond to changes in exercise levels. Scandinavian journal of medicine & science in sports, 12(2), 63-64.
Cook, J., & Purdam, C. R. (2009). Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. British journal of sports medicine, 43(6), 409-416.
Cook, J. L., Khan, K. M., & Purdam, C. (2002). Achilles tendinopathy. Manual therapy, 7(3), 121-130.
de Jonge, S., de Vos, R.-J., Van Schie, H. T., Verhaar, J. A., Weir, A., & Tol, J. L. (2008). One-year follow-up of a randomised controlled trial on added splinting to eccentric exercises in chronic midportion Achilles tendinopathy. British journal of sports medicine, bjsports52142.
Enoka, R. M. (1996). Eccentric contractions require unique activation strategies by the nervous system. Journal of Applied Physiology, 81(6), 2339-2346.
Hortobágyi, T., Barrier, J., Beard, D., Braspennincx, J., Koens, P., Devita, P., . . . Lambert, J. (1996). Greater initial adaptations to submaximal muscle lengthening than maximal shortening. Journal of Applied Physiology, 81(4), 1677-1682.
Knobloch, K. (2007). Eccentric training in Achilles tendinopathy: is it harmful to tendon microcirculation? British journal of sports medicine, 41(6), e2-e2.
Langberg, H., Ellingsgaard, H., Madsen, T., Jansson, J., Magnusson, S., Aagaard, P., & Kjær, M. (2007). Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scandinavian journal of medicine & science in sports, 17(1), 61-66.
Magnusson, S. P., Narici, M. V., Maganaris, C. N., & Kjaer, M. (2008). Human tendon behaviour and adaptation, in vivo. The Journal of physiology, 586(1), 71-81.
Malliaras, P., Barton, C. J., Reeves, N. D., & Langberg, H. (2013). Achilles and patellar tendinopathy loading programmes. Sports Medicine, 43(4), 267-286.
Malliaras, P., Purdam, C., Maffulli, N., & Cook, J. (2010). Temporal sequence of greyscale ultrasound changes and their relationship with neovascularity and pain in the patellar tendon. British journal of sports medicine, 44(13), 944-947.
Morrissey, M. C., Harman, E. A., & Johnson, M. J. (1995). Resistance training modes: specificity and effectiveness. Medicine and Science in Sports and Exercise, 27(5), 648-660.
Öhberg, L., Lorentzon, R., & Alfredson, H. (2004). Eccentric training in patients with chronic Achilles tendinosis: normalised tendon structure and decreased thickness at follow up. British journal of sports medicine, 38(1), 8-11.
Robinson, J., Cook, J. L., Purdam, C., Visentini, P., Ross, J., Maffulli, N., . . . Khan, K. (2001). The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. British journal of sports medicine, 35(5), 335-341.
Roig, M., O'Brien, K., Kirk, G., Murray, R., McKinnon, P., Shadgan, B., & Reid, D. W. (2008). The effects of eccentric versus concentric resistance training on muscle strength and mass in healthy adults: a systematic review with meta-analyses. British journal of sports medicine.
Rompe, J. D., Nafe, B., Furia, J. P., & Maffulli, N. (2007). Eccentric Loading, Shock-Wave Treatment, or a Wait-and-See Policy for Tendinopathy of the Main Body of Tendo Achillis A Randomized Controlled Trial. The American journal of sports medicine, 35(3), 374-383.
Scott, A., Cook, J. L., Hart, D. A., Walker, D. C., Duronio, V., & Khan, K. M. (2007). Tenocyte responses to mechanical loading in vivo: a role for local insulin‐like growth factor 1 signaling in early tendinosis in rats. Arthritis & rheumatism, 56(3), 871-881.
Silbernagel, K. G., Thomeé, R., Eriksson, B. I., & Karlsson, J. (2007). Continued Sports Activity, Using a Pain-Monitoring Model, During Rehabilitation in Patients With Achilles Tendinopathy A Randomized Controlled Study. The American journal of sports medicine, 35(6), 897-906.
Silbernagel, K. G., Thomee, R., Thomee, P., & Karlsson, J. (2001). Eccentric overload training for patients with chronic Achilles tendon pain–a randomised controlled study with reliability testing of the evaluation methods. Scandinavian journal of medicine & science in sports, 11(4), 197-206.