Functional assessment of a water skiing injury
Introduction
The aim of this blog is to outline a case study on a lower back injury sustained from waterskiing and the importance of performing a thorough functional assessment. After completing my Masters I developed a framework for performing a initial musculoskeletal assessment, which I could apply to almost all presentations. For this presentation however my main focus was on the functionally task and mechanism of injury.
Patient history.
27 y.o male recreational waterskiing was pulling out of the water when his shorts filled up with water creating a large amount of drag and while holding on, the person developed sharp right sided upper lumber pain. On presentation the athlete described sharp right upper lumber pain with a block in movement into right trunk rotation. The pain was intermittent and settled quickly after returning to neutral. There was no referred pain or other symptoms.
Getting out of the water:
- Mostly left leg forward.
- Right leg in the water or placed in the back binding.
- Main resistance through the left leg while the trunk is maintained in neutral, holding on with both arms.
Objective assessment
Functional assessment: I got the patient to sit on the edge of the plinth and best demonstrate the posture of getting up on a slalom ski.
Trunk active range of movement:
- Lateral flexion was unimpaired.
- Flexion and extension was unimpaired.
- Right trunk rotation 0 degrees.
- L trunk rotation 80 degrees.
Straight leg raise 70/70 left = right R2 hamstring, no change in back pain.
Palpation: local spasm and tenderness over T12 L1, no significant hypomobility.
Clinical reasoning
Day 1 I decided to explore the effect of various manual treatments in the form of mini treatments to try gauge a better understanding of irritability.
Treatment 1: soft tissue release of the over-lying erector spinae // no change in rotation.
- Treatment 2: Gr IV R PAIVMS T12 L1 // again no change in right trunk rotation.
- Treatment 3: Left rotation MWM with R PA T12 x 10 repetitions // right rotation 50 degrees, L rotation 0 degrees…. Oh dear….
Always be prepared to challenge your list of hypotheses.
The sudden shift in ability to rotate to the right but not back to the left suddenly made me re-evaluate what I thought was causing this movement impairment. There was minimal change with muscular and articular focussed treatments. I was cautious of the sudden shift in movement from one side to the other.
The patient was young, health, his general health unremarkable, no other red flags and mechanical pain. So what else could it be?
I wondered if there was neurodynamic impairment contributing to this problem. So I took myself back to the functional position. In sitting I asked the patient to extend his left knee and hold it straight while re-examining trunk rotation, and suddenly both left and right trunk rotation were 70-80 degrees and there was a significant reduction in reported pain. (The same effect wasn’t achieved with right knee extension or double leg extension.)
The functional position of skiing, having the left leg extended and rotating the trunk to the right allowed the movement to be unrestricted and repeated rotations lead to a carryover in range when the knee was flexed.
Is this a neurodynamic impairment? If it is, then is there a problem with the nerve physiology or mechanics of movement? My impression is that it that there was a restriction in movement causing a block of right thoracic rotation. With the addition of knee extension (causing a caudal movement of the spinal cord), the joint restriction improved. Therefore there is a problem at the interface in the upper lumbar/lower thoracic spine which is not blocked by spasm or joint stiffness, but my pathoneurodynamics.
The fact that the leg it sustained in extension during skiing suggested that holding the knee extended rather than performing a ‘sliding’ technique would be more functionally specific. This doesn’t exactly define the problem as either sliding or tension dysfunction.
Day 1 treatment and home exercise program:
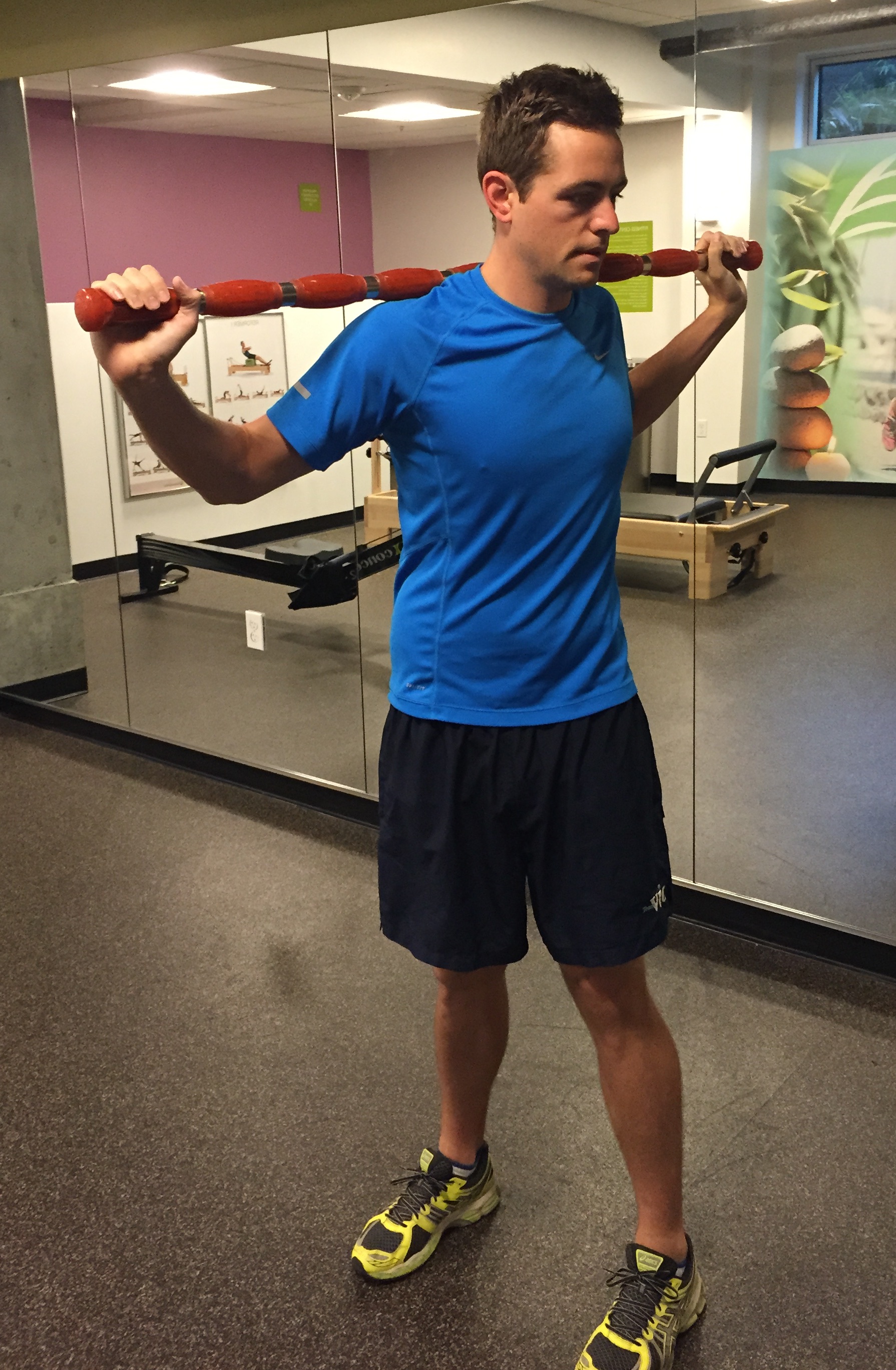
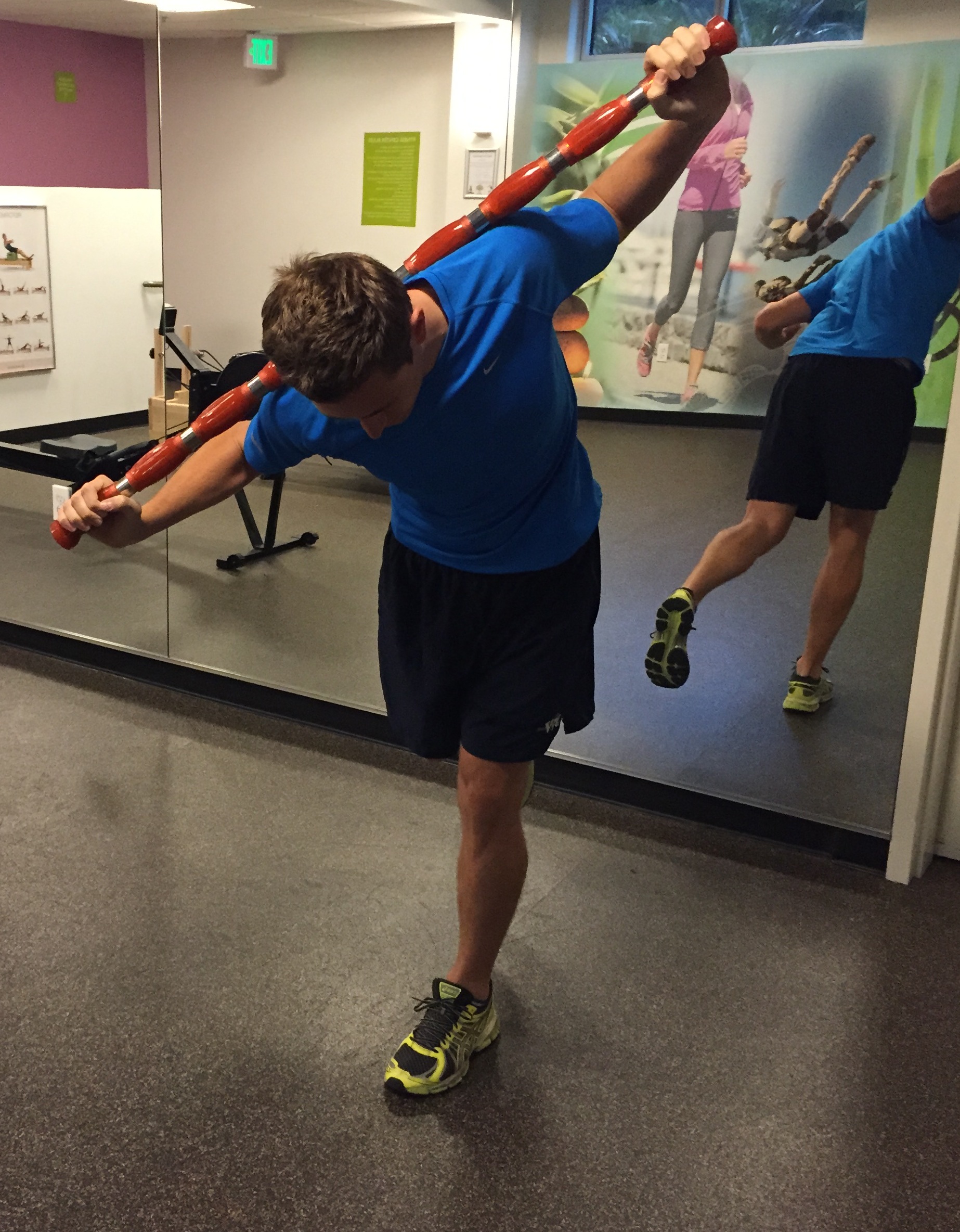
Asking the patient to hold a bar across his shoulders, balance on the left leg and with the knee straight bend forward into a single leg dead lift position and in the position perform trunk right rotation.
The patient found this easy to complete as a home exercise program and within two days of regular stretches during the day, his trunk rotation was restored to normal.
Clinical impression
This case study is an example of when I needed to chase the functional impairment and without having a clear understanding of the exact cause of the pain, use my understanding of neurodynamics and a biomechanical assessment to directly address the problem and provide a home exercise program which addressed the functional aggravating movement and the physical impairments.
Together with the help of the patient we worked through the problem together and within one session, his movement was restored. I would love to hear your thoughts on this case presentation and how you might have approach the same problem differently.
Here is a sequence of pictures outlining how this patient independently assesses in trunk rotation and actively mobilises to maintain his range of movement.








This is my first blog from my new home in San Francisco, Sian




