The pain of social disconnection
I began writing this blog in August 2014 when I came across an interesting article written by Associate Professor in Social Psychology, Naomi Eisenberger, who works in the Department of Psychology at the University of California in LA. Naomi asks a single question which I feel is so applicable to clinical practice as a physiotherapist "Why is it that negative emotions have such a profound effect on our emotional wellbeing?" In her research on social and affective neuroscience, one particular paper publish by Eisenberger in 2012 is titled "The pain of social disconnection: examining the shared neural underpinnings of physical and social pain". The reason it has taken me so many months to revisit this topic, is that I was so drawn to the title and intrigued about the paper, but I didn't know what message I was going to or needed to share.
Until recently.
The exact event that reignited my interest in this topic was neither drastic or unfamiliar. It was a young active women (one of my American friends) who is in her mid twenties, and she developed an overuse injury from completing a half marathon. It was a tibial stress fracture. I was disturbed by witnessing the devastation that unravelled when she was told by her treating doctor, that she wouldn't be able to run again for two months and wouldn't be able to participate in a fun run she had set up as a fundraiser for her birthday (being held in 6 days times).
For most, this news would come as a disappointment, but for this particular individual, the idea of not running, not participating in a the most positive activity in her life, was completely devastating.
When completing my undergrad studies, we were taught about paradigm shift that was occurring in our profession, from a bio-medical model to a bio-psycho-social model of care. What this meant is that research and clinicians were discovering that the best management for a person had to look beyond their physical impairments and into understanding the role of cognitive and behavioural factors, as well as the impact on participation restrictions and other social factors. At the time my naive and confident self thought "well dah - that's just common sense"... but what i've come to learn, is applying this model of care isn't always that easy.
This is a diagramatic representation of the WHO-ICF framework developed by the World Health Organisation for the International Classification of function, disability and health. What it highlights is the key areas of :
- Physical impairment in body structure & function.
- Activity limitation
- Participation restriction
- Contextual influences such as personal factors and environmental factors.
As mentioned previously, this framework is used to teach health practitioners about the bio-psycho-social aspects of disease, but after a few years of clinical practice, I've come to believe that we are taught how to thoroughly assess and manage and 'psycho' and 'social' aspects of our patients' care.
Below is a summary of the key learning points and ideas shared by Eisenberger in this paper.
Social & Physical Pain are interconnected and may be processed by similar neural networks.
- The most obvious representation of the connect between social and physical pain is the common language used to describe both situations e.g. broken bones & broken heart.
- The definition of social pain reflects the same broad expressions as physical pain, where social pain is defined as "the unpleasant experience that is associated with actual or potential damage to one's sense of social connection or social value" (Eisenberger, 2012, p. 1).
- The most widely accepted definition of pain is "an unpleasant experience associated with actual or potential tissue damage".
- It is hypothesised that social pain is processed mentally by some of the same neural networks that process physical pain, which might explain the similarities in definition as well as the language we choose to describe physical and social pain.
- An interesting point to reflect on is the physical sensations you might feel when in emotional or social distress? I find this to be another representation of the connection between the two.
Neural substrates and pathways in the brain.
- Neuro-imaging has been used in human studies to observe the regions of the brain which are activated in both physical and social pain.
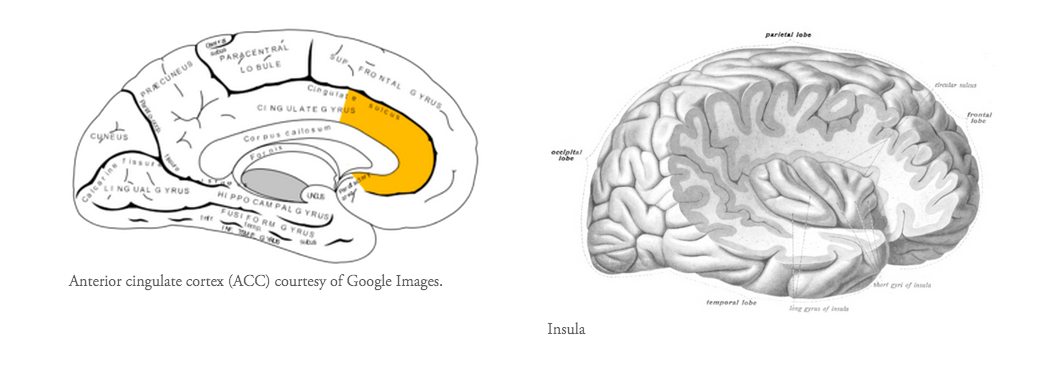
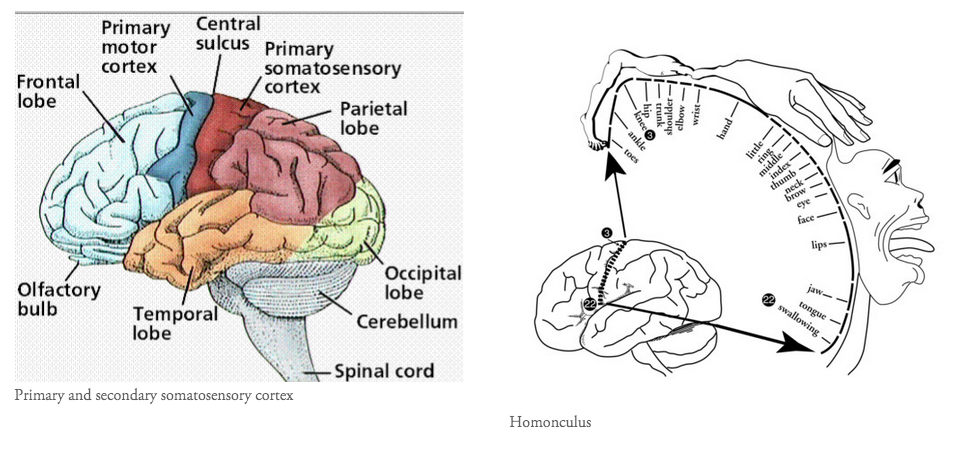
- The anterior cingulate cortex and anterior insula are regions of the brain shared in both pain states.
- In social pain the subgenual anterior cingulate cortex is also activated and in physical pain, regions such as the primary and secondary sensory cortices and thalamus are active. There isn't a perfect overlap but definitely the presence a shared pathway.
- The anterior cingulate cortex is part of the cingulate gyrus and is thought to be responsible for autonomic functions (regulating heart rate and blood pressure) and cognitive functions (reward anticipation, decision making, empathy, impulse control and emotion). Moseley (2003) describes it as the action centre which causes humans to think "what should I do?" In relation to pain, the ACC is thought to provide an emotional description of pain and to coordinate an appropriate response.
The insula cortex is found within the deep folds of the cerebral cortex and is involved in linking emotion to action. These functions may include perception, self-awareness, cognitive function, and motor control i.e it is involved in understanding the physiological functioning of the entire body.
- In a previous blog I've explored the regions of the pain which activate during physical pain, commonly referred to as the pain neuromatrix. This blog explores the function of each region of the brain, but in short, the pain matrix is thought to consist of the dorsolateral prefrontal cortex, insula cortex, anterior cingulate cortex, primary and secondary sensory cortices, and the thalamus (Moseley, 2008). Every individual has a unique pain experience (an unique neuromatrix), but there are some areas of the brain (listed above) which are seen to be more frequently active on brain functional imaging.
- So there is a shared link in neural pathways and the paper continues on to discuss the shared link in neurochemicals as well. The paper describes how research has shown that there is down-regulation of pain through endogenous brain opiod systems in both pain states.
- To help you visual where all these parts of the brain are, I've put some pictures below. What is interesting to note is that no single region of the brain is involved in pain, instead parts from all over the brain activated in specific networks to process efferent message and produce the afferent output of pain.
Consequences of shared circuitry
- It is hypothesised that there are two main consequences of social and physical pain sharing the same circuitry.
- The first is that if an individual is more sensitised to one type of pain they may be more sensitive to the other.
- The second is that increased levels of one type of pain will result in increased levels in the other.
- But if we flip this consequence, what these hypotheses suggest is that increasing participation and social inclusion is likely to have an inhibitory effect on pain. This is a concept that I personally find very interesting and I think it specifically relates to the patient described in this blog. Promoting self esteem, self efficacy and other components of emotional wellbeing will have an inhibitory effect of physical pain.
Coming back to the scenario described above and to expand a bit further... I was sharing my discomfort with another friends as a means on decompression and as I explained the scenario I broke it down into two main problems. The first is the actual tissue damage that requires time to heal and the second was the implication this had on both running recreationally and an imminent 'fun run'. As I was explaining the situation to a non-health professional I broke down the WHO-ICF framework and discussed that I had no way of impacting the physical impairment and therefore didn't know how to change the distress of activity limitation. The response I received was 'to postpone the fun run until healing had occurred so that they don't feel like they are missing out and to make a care package and go for a girls night out to cheer her up'. Honestly, a solution I had not considered. The most brilliant solution too. Enhancing aspects of self efficacy, self confidence and social inclusion to reduce the impact of the physical pain. (Luckily the person I'm using as an example is my friend, so there is no breach of ethical boundaries but choosing this solution - but its a great example of a non-physio way to approach a problem).
The main message I want to share with my readers is that....
- The link in neural circuitry is both a detrimental link between social and physical pain and positive link as it allows management/treatment of pain through social reconnection.
- Focussing on the overlap that exists between social and physical pain provides new approaches for the treatment of factors that contribute to physical pain.
- It encompassing the approach of cognitive behavioural therapy and functional reintegration as concepts of pain management.
So what prompted me to come back to this topic is that as physiotherapists there will be times when we can offer nothing to a patient to change their injury or speed their recovery, but, we can help our clients understand and breakdown what impact the problem has on their life, and strategise ways minimise both the activity limitation and participation restriction they may experience.
If there is a neural connection existing between social and physical pain I'd like to challenge you by asking "To what extent does your current practice reflects a true biopsychosocial approach, and accommodates for the actual or potential negative effects of social isolation in pain states?
The interesting thing about this story is the scientific evidence that supports the connection that lies between both pain states. I believe this research can be of real advantage to Physiotherapists as they approach treatment from a biopsychosocial approach.
Sian
References:
Eisenberger, N. I. (2012). The pain of social disconnection: examining the shared neural underpinnings of physical and social pain. Nature Reviews Neuroscience, 13(6), 421-434.
Moseley, G. L. (2008). Pain, brain imaging and physiotherapy—Opportunity is knocking. Manual therapy, 13(6), 475-477.