Neurodynamic solutions for the upper quadrant
I recently attended a course run by Michael Shacklock called "Neurodynamic Solutions for the Upper Quadrant". The concept of clinical neurodynamics started to emerge in the 1980's with the research conducted by world-renown physiotherapists such as David Butler, Michael Shacklock, Clifford Woolf, Lorimer Moseley and Louis Gifford. I'm sure there are many other authors who have contributed to the research and clinical application of pain science. These are the authors I am drawn towards when furthering my knowledge on this topic. Michael has been the driving force being the development of clinical neurodynamics and its integration in physiotherapy practice worldwide.
The course with Michael Shacklock was truly eye opening. I learnt so much about the research behind the development of clinical neurodynamics and the neurophysiological basis of the tests and treatments. Although it was a course which focused on the upper quadrant, the principles can be applied generally throughout the body.
"Clinical neurodynamics is the clinical application of mechanics and physiology of the nervous system as they relate to each other and are integrated with musculoskeletal function" (Shacklock, 2005, p. 2).
"An important aspect of this approach is that healthy mechanics of the nervous system enable pain-free posture and movement to be achieved. However, in the presence of pathomechanics of neural tissues (e.g. nerve entrapment), symptoms may be provoked during daily activities" (Shacklock, 1995, p. 9).
"Clinical neurodynamics is for clinicians dealing with musculoskeletal disorders with peripheral neurogenic pain mechanisms, including those of the nerve root and peripheral nerve" (Shacklock, 2005, p. xii). My aim with this blog is to share some of the key concepts I learnt during the course. In the second blog I will give a clinical example of how I applied these new clinical tools to an interesting case of a patient with posterior shoulder pain.
During the course, Michael taught us about two main concepts:
1. Pathoneurodynamics
The gold standard of neurological examination is nerve conduction studies. In many cases however there can be pathoneurodynamics without conduction loss within the nerve. Neurodynamic assessment techniques allow us to look for these changes, especially when neurological examination is normal.
Coming back to this quote
"Clinical neurodynamics is the clinical application of mechanics and physiology of the nervous system as they relate to each other and are integrated with musculoskeletal function" (Shacklock, 2005, p. 2).
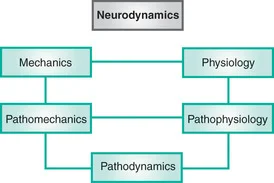
The movement of the nervous system is known as mechanics and pathomechanics, while the health of the nervous system is referred to as physiology and pathophysiology. Pathoneurodynamics is often a combination of both pathomechanics and pathophysiology.
Having an overt positive response on a neurodynamic test does not differentiate the cause of the problem and we still have to identify whether there are faulty mechanics or faulty physiology within the neural tissue. We also have to understand if the problem lies within the nervous tissue itself, the tissues it innervates, or the surrounding interface of soft tissue structures.
From, Shacklock M, Clinical Neurodynamics, Elsevier, Oxford, 2005.
From, Shacklock M, Clinical Neurodynamics, Elsevier, Oxford, 2005.
2. Levels of assessment & treatment
When performing a test first decide if you are performing a neurodynamic test or a musculoskeletal test. The aim firstly is to exclude neural tissue involvement in the problem, hence the the tests need to be performed precisely and accurately. If a response is elicited then apply structural differentiation. A response can be symptom evocation but also a physical effect such as difference in ROM, resistance, muscle spasm and protective movements. Chapter 5 of Clinical neurodynamics outlines diagnosis with neurodynamic tests and the definition of position response (covert & overt) and normal responses.
Once the assessment has been conducted and an overt abnormal response (positive test finding implicating pathoneurodynamics) has been found, clinical reasoning is then used to determine the cause. This may include pathophysiology or pathomechanics. Once we determine that treatment is safe and indication, we must determine if we treat mechanical open/closing dysfunction, neural sliding/tension dysfunction, or physiological dysfunction.
From there a level of suitable treatment can be determined.
Level 0 - neurodynamic examination is contraindicated.
"Another example that leads to neurodynamic tests being inappropriate is severe pain in which an examination would be too intrusive and provoke the patient's symptoms unnecessarily. Also, it may be inappropriate to perform neurodynamic tests in cases where there is a heavy bias toward psychosocial issues. Any contraindication that exists for manual therapy generally also applies to neurodynamic testing" (Shacklock, 2005, p. 108).
Level 1 - limited examination.
"The level 1 (limited) examination is performed when care not to provoke symptoms is the primary concern. Some of the components of a neurodynamic test may be omitted so that only minimal forces are applied to the nervous system. It may also be necessary to modify the sequence of movements to achieve the desired goals. In the level 1 examination, the full neurodynamic tests are not completed" (Shacklock, 2005, p.108).
- Level 1a - position out of tension with the ipsilateral side and position further out of tension with the contralateral side.
- Level 1b - position out of tension with the ipsilateral side (same as Level 1a) and move out of tension with the contralateral side.
- Level 1c - position in tension with the ipsilateral side and move out of tension with the contralateral side.
- Level 1d - position out of tension with the contralateral side and move into tension with the ipsilateral side.
- Level 1e - position in tension with the contralateral side and move into further tension with the ipsilateral side. Level 1e is essentially a standard/level 2 examination.
If you're still struggling to understand how these positions work, Michael has shared this video explaining the movements described above.
Level 2 - standard neurodynamic examination.
"This examination consists of use of the standard tests for musculoskeletal and neural structures and, as in the level 1 examination, tests the three key components (interface, neural, innervated tissue) separately. The neurodynamic tests are performed to a comfortable production of symptoms. If sufficient information has been gathered without much in the way of symptoms, all the better. It is not necessary that the tests be taken to their end range but it is permissible, as long as this is clinically appropriate. The neurodynamic position is only held for a matter of seconds" (Shacklock, 2005, p.109).
Many of us are familiar with the standard tests and therefore they are not described in this blog.
Level 3 - advanced neurodynamic examination.
"The term 'sensitization' refers to making testing of the nervous system more able to detect changes in nervous system function. Hence, even though sensitization is a generic term that applies to all levels of examination above standard testing (level 2), specific features apply to higher levels that are reflected in the following. Furthermore, it is at level 3 that specific 'types' of examination are applied and these are based on the method of sensitization and the causal mechanisms" (Shacklock, 2005, p. 110).
- Level 3a - neurodynamically sensitised. Defined as adding more neural tension to the standard neurodynamic test through the addition of sensitising movements i.e. 'more of the same technique'.
- Level 3b - localised neurodynamic sequencing to emphasise a particular part of the nervous system.
- Level 3c - multi-structural examination where neural structures are assessed in combination with musculoskeletal tests.
- Level 3d - Symptomatic movements are used to make the test more specific to the symptomatic activity.
- Level 3e - performing the examination with the aggravating activity being repeated prior to assessment.
As you can see from the levels of testing outlined about, we have a large variation in examination available for clinical use. Prior to attending Michael's course I hadn't understood the role of each level of assessment and how to interpret the findings and apply the information to planning and application of treatment.
The next blog is a clinical example of thinking outside the square with a patient with posterior shoulder pain.
Sian
References
Shacklock, M. O. (2005). Clinical neurodynamics: a new system of musculoskeletal treatment. Elsevier Health Sciences.