Entrapment Neuropathies of Upper Limb
Sian and I both attended Michael Shacklock’s Neurodynamics Upper Limb Course in Melbourne in June. This was easily the most enlightening course I have attended, it completely revolutionised my thinking and treatment of neural conditions. It introduced much more sensitive treatment techniques, especially for acute and severe neural conditions. I can recommend for every physiotherapist to attend one of Michael’s courses, or purchase his book “Clinical Neurodynamics” and prepare to be astounded. For those in Melbourne, Michael is presenting course on Neurodynamic Solutions in the Lower Limb in 2015, through the APA.
Shacklock’s neurodynamics approach is too large a topic for just one blog, so I will expand on entrapment neuropathies of the radial and ulnar nerves.
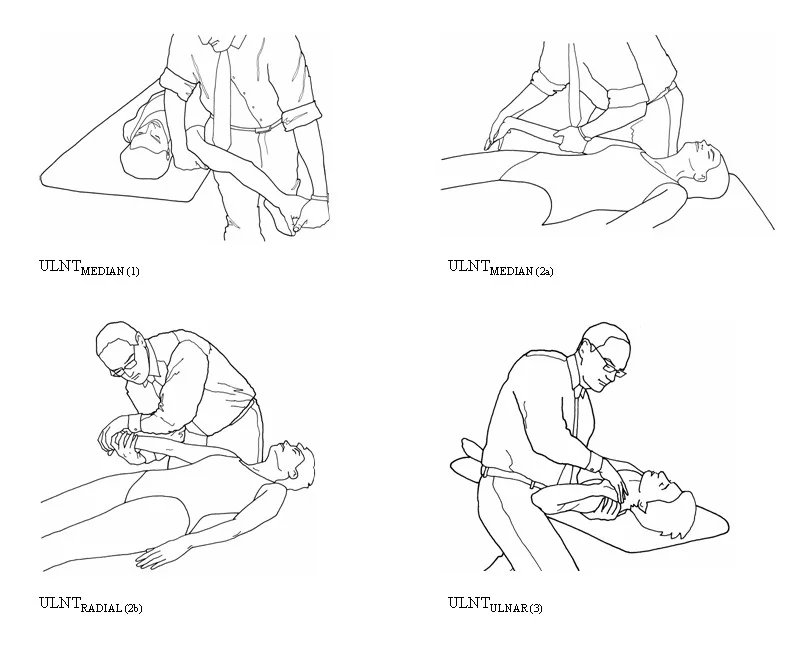
Neurodynamic Testing – what is positive?
Cleland and Koppenhaver (2011) define a positive neurodynamic response as having any one of the following: symptom reproduction, change in symptoms with distant segmental movement or a difference between limbs of >10°, however research dictates at least two of three be present to be considered positive. Normal sensory responses include aching, burning, stretching, or tingling in the medial elbow, the forearm, or hand. Structural differentiation, movement of distant segments which alter symptoms, is the most clinically relevant response and considered characteristic of neural mechanosensitivity (Butler, 1989; Elvey, 1979; Lohkamp & Small, 2011). Traditionally in the upper limb, ipsilateral or contralateral cervical side-flexion is most common, although you should employ a movement distant to the pain site, i.e. wrist flexion/extension for patient presenting with neck pain. The literature describes a between-sides difference ranging from 10° to 37° on neurodynamic testing, however with varying methodology. A recent study by Stalioraitis and colleagues (2014) shows a between-sides difference of >15° is required for the median nerve and >11° for the radial nerve to be clinically significant and not a normal variation, the ulnar nerve was not tested. The process and analysis employed in this article is the best I have read, and I’m comfortable using these values until further research discounts this.
Butler DS, The Sensitive Nervous System, Unley, DC, Australia: NOIgroup Publications, 2000
Ulnar Entrapment Neuropathies
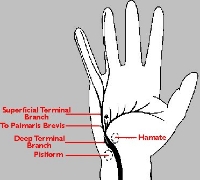
The ulnar nerve passes the arcade of Struthers then enters the cubital tunnel (fibrous canal) at the medial epicondyle. The tunnel roof is formed by a band of fascia between the olecranon and the medial epicondyle and is the tunnel between the two heads of flexor carpi ulnaris. The nerve passes beneath the arcuate ligament then travels through the anterior compartment of forearm. It enters the wrist at Guyon’s canal, which is a fibrous tunnel between the hook of hamate and pisiform.
Cubital Tunnel (courtesy of www.google.com)
Guyon's Canal (courtesy of www.google.com)
Cubital Tunnel Syndrome
Cubital tunnel syndrome is the entrapment of the ulnar nerve in this structure. Bayramoglu (2004) claimed, during elbow flexion, the tunnel flattens as the ligament stretches, causing pressure on the ulnar nerve. Sustained elbow flexion (malposition during work or sleep), abnormal bands of fascia, subluxation or dislocation of nerve over medial epicondyle could result in entrapment. This is a critical point to note in subjective questioning, especially in regards to their aggravating factors.
Symptoms include:
- initially hand clumsiness, weakness, cramping in small hand muscles
- tingling in ulnar distribution (medial 4th & all of 5th finger and ulnar palm)
- weakness – pinch grip, eventually reduced power grip, advanced cases get clawhand due to atrophy of interosseous & hypothenar muscles
- enlarged nerve on palpation in cubital fossa
Cleland and Koppenhaver (2010) describe three tests which have a high sensitivity & specificity for cubital tunnel syndrome, all are considered positive if the patient reports reproduction of their symptoms. Although these are suggested, a thorough neurodynamic test with structural differentiation and nerve palpation should provide a conclusive diagnosis.
- Ulnar Bias Neurodynamic Test that reproduces pain, numbness, or tingling symptoms is considered a positive sign (sen 0.75, sp 0.99), however can be made more sensitive with structural differentiation.
- Pressure Provocation Test – elbow in 20° flexion & full supination, apply pressure to ulnar nerve just above the cubital tunnel for 60 seconds (sen 0.89, sp 0.98).
- Combined Pressure & Flexion Provocation Test – maximal elbow extension & supination, pressure applied just proximal to the cubital tunnel for 60 secs (sen 0.98, sp 0.95)
Differential Diagnosis:
- C8/T1 – dermatomal pattern of 4th/5th fingers, weakness of hand intrinsics, often neck involvement (pain, reduced ROM)
- Thoracic Outlet Syndrome – pain, paraesthesia, weakness in arm, shoulder & neck, possible arterial or venous symptoms (arm feels cold, 'poor circulation' feeling)
- Ulnar Collateral Lig Insufficiency – underlying laxity causing ulnar irritation, laxity on collateral testing
- Pancoast Tumour - Abnormal growth of tissue on apex of lung causing compression of lower trunk of brachial plexus, similar signs to C8/T but also red flags (night sweats, loss of weight, malaise, constant pain, history of malignancy)
Guyon's Canal entrapment (courtesy of www.google.com)
Guyon’s Canal Entrapment
Zone 1 (zone 2 in picture above) holds the motor branch of the nerve after it has bifurcated into dorsal cutaneous branch (about 7cm proximal to the canal) so no loss of sensation dorsally. Entrapment here causes pure loss of motor function to all of the ulnar-innervated muscles in the hand. A ganglion or fractured hook of hamate are the most common causes of entrapment. Palpation in the area is the best way to diagnose.
Zone 2 - sensory branch of the bifurcated nerve, causes sensory loss to the hypothenar eminence, the small finger, and part of the ring finger, but it does not cause motor deficits. Common causes are synovial inflammation and muscle hypertrophy/compression. Again, palpation is the most useful diagnostic tool.
Cyclist’s Palsy/Handlebar Palsy – cyclists who ride long distances in wrist extension with the hook of hamate pressed against the handlebars, compressing the ulnar nerve, causes sensory loss to 5th and half 4th digit and weakness of hand intrinsics.
Radial Nerve Entrapment Neuropathies
Radial Tunnel (courtesy of www.google.com)
The radial nerve divides inside the radial tunnel, into a superficial and deep branch. The superficial branch is sensory only. The deep branch is the posterior interosseous nerve which winds around the lateral radius and through the supinator muscle. The radial tunnel spreads from the lateral epicondyle to the supinator muscle. The arcade of Frohse is a fibrous ring located at the proximal edge of the supinator muscle, the literature all describe this arcade as the most common place of radial entrapment.
Posterior Interosseous Nerve Entrapment
The patient may describe vague forearm pain (Spinner, 2003) while Corwin (2006) states pain may be felt over the lateral elbow but is not the most noticeable symptom. Symptoms include gradual or sudden weakness of thumb & finger extension (Corwin, 2006). Patients are able to extend their wrist but only in radial deviation, as extensor carpi radialis longus (ECRL) is innervated before the radial nerve bifurcates. They will be unable to extend in neutral or ulnar deviation. They may hold their wrist in radial deviation due to this muscle activation. No sensory loss as the nerve is motor only and no Tinel’s sign will be present.
Differential Diagnosis:
- Lateral Epicondylalgia – no noticeable weakness of wrist + finger extensors, negative neurodynamic testing
- C8 Radiculopathy – loss of thumb extension & finger flexion (long finger flexors) not extension, probable sensory signs (paraesthesia, numbness)
- Extensor Tendon Rupture – loss of tenodesis, also history of trauma
Entrapment neuropathies can occur at any point along the course of the nerve, with the above conditions being the most commonly seen clinically. A thorough and specific neurodynamic assessment carefully isolating each joint movement, along with nerve palpation, can assist in diagnosis of these conditions.
Alicia
References:
Bayramoglu, M. (2004). Entrapment neuropathies of the upper extremity. Neuroanatomy, 3(1), 18-24.
Butler, D.S. (2002) The Sensitive nervous system. Unley, Australia: Noigroup Publications.
Campbell, W. W. (1997). Diagnosis and management of common compression and entrapment neuropathies. Neurologic clinics, 15(3), 549‐567.
Cleland, J., Koppenhaver, S., & Netter, F. H. (2011). Netter's orthopaedic clinical examination : an evidence-based approach (2nd ed.). Philadelphia, Saunders/Elsevier.
Corwin, H. M. (2006). Compression neuropathies of the upper extremity. Clinics in occupational and environmental medicine, 5(2), 333-352, viii.
Lohkamp, M., & Small, K. (2011). Normal response to Upper Limb Neurodynamic Test 1 and 2A. Manual Therapy, 16(2), 125-130.
Shacklock, M. (2005). Clinical Neurodynamics: A new system of musculoskeletal treatment. Edinburgh: Elsevier.
Stalioraitis, V., Robinson, K., & Hall, T. (2014). Side-to-side range of movement variability in variants of the median and radial neurodynamic test sequences in asymptomatic people. Manual therapy, 19(4), 338-342.