Muscle Synergies of the Hip and Pelvis
Grimaldi and colleagues have published several articles which outline the muscle synergies around the hip and the changes in muscle function associated with hip joint pathology. A previous blog has outlined the changes associated with osteoarthritis. This blog goes into further detail about these muscle synergies.
When assessing the hip it may be helpful to view groups of muscles as synergies rather than individual units. Understanding the role of muscle synergies can allow us to select functional tasks to assess different aspects of muscle function.
Layers of control
Grimaldi (2009) breaks down muscles into layers of control as follows:
- Deep muscle system
- Primarily act to control the movement of the femoral head in the acetabulum.
- Iliacus, gluteus minimus, obturator externus, obturator internus, gamelli, and quadratus femoris.
- Intermediate muscle system
- Plays a role in torque production and control of the pelvis on the femur in weight bearing.
- Gluteus medius, piriformis, short adductors, and iliopsoas.
- Superficial muscle system
- Primary function in torque production, also controls pelvis/hip control, and controls high load functional tasks.
- Gluteus maximus, TFL, long adductors, Rectus femoris, Satorius, and the hamstrings.
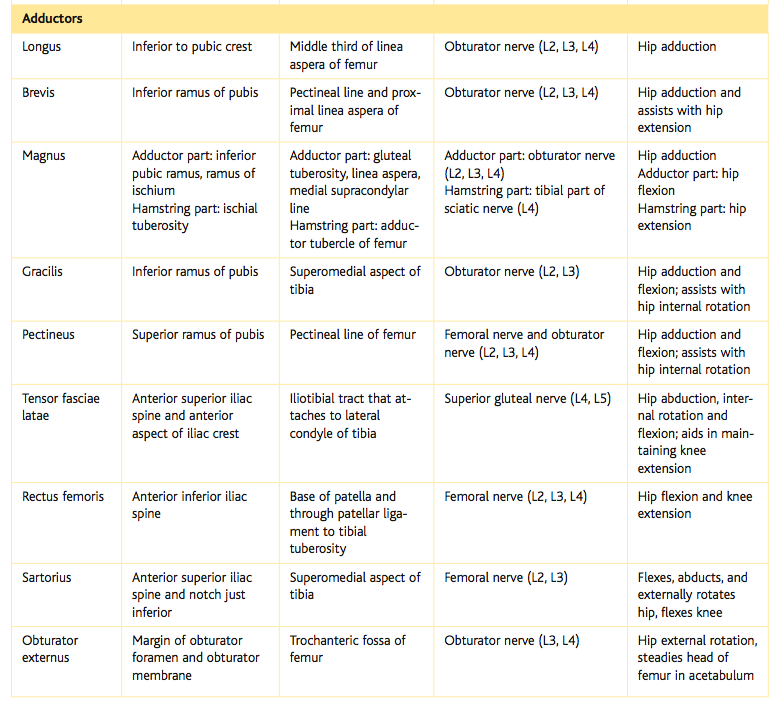
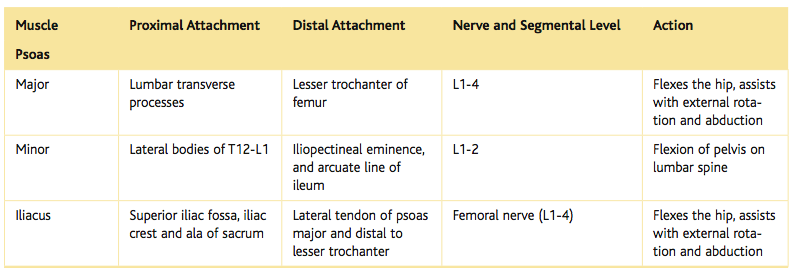
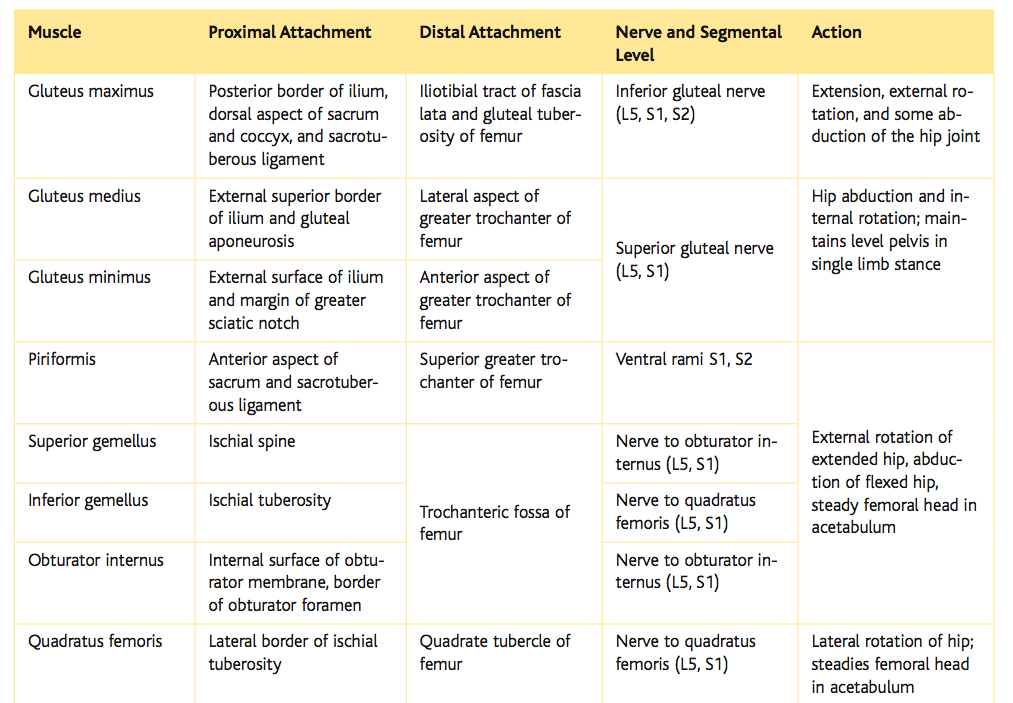
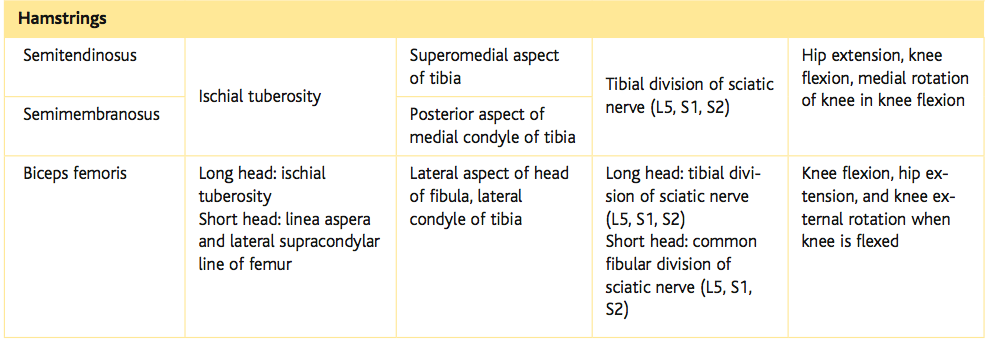
Thinking of muscles in terms of 'Layers of control' is how I was taught about muscles during university. We learn their individual origin, insertion, innervation, and action. There are tables below displaying this information. An alternative system for visualising how these muscles act together is that of muscle synergies. The descriptions below of each synergy has been summarised from the work by Grimaldi (2011).
The extensor synergy
Firstly lets talk about the action of gluteus maximus, the primary hip extensor muscle.
- Individual actions:
- The upper portions of gluteus maximus arise from above the axis of rotation and are primarily involved in abduction.
- The lower portions of gluteus maximus sit below the axis of rotation and are primarily involved in extension.
- Both UGM and LGM contribute to external rotation (Grimaldi, Richardson, Durbridge, et al., 2009, p.612).
- Both UGM and LGM are active during heel strike to help absorb ground reaction forces which causes lateral pelvic drop and flexion moments at the hip (Grimaldi, Richardson, Durbridge, et al., 2009, p.616).
Posterior muscles of the hip and thigh (Cleland, 2005, p. 249)
The abductor synergy
The hip abductor synergy comprises of UGM, tensor fascia latae (TFL) and vastus lateralis (VL) (superficial system), GMed and piriformis (intermediate system), and GMin (deep system).
- TFL and UGM with ITB create the deltoid of the hip.
- Vastus lateralis is thought to contract and act as a hydraulic amplifier.
GMed: The anterior and posterior portions sit deep to the middle or lateral superficial portion. These deep parts may be involved more in joint protections with the superficial parts being more involved in torque production. This is explained by the separate innervations to each portion of the GMed muscle (Grimaldi, 2011).
GMin: Has a strong attachment to the superior aspect of the capsule and acts to resist supero-lateral and anterior migration of the femoral head. It is active in all directions of hip movement except adduction.
- At 0 degrees hip flexion:
- Anterior GMed is an internal rotator, middle GMed is an abductor and posterior GMed and piriformis are external rotators and abductors.
- At 90 degrees hip flexion:
- All portions of GMed and piriformis act as internal rotators, and posterior GMed and piriformis act also as abductors.
The flexor synergy
The hip flexor synergy consists of sartorius, rectus femoris (RF), tensor fascia-latae (TFL), adductor longus (ADL) and pectineus (superficial), iliopsoas (intermediate), and iliacus and iliocapsularis (deep system).
- Iliacus
- Activates prior to hip flexion at the end of stance phase to stabilise the femoral head anteriorly.
- Covers the head of femur where the capsule is deficient and forms a sling at the front of the joint.
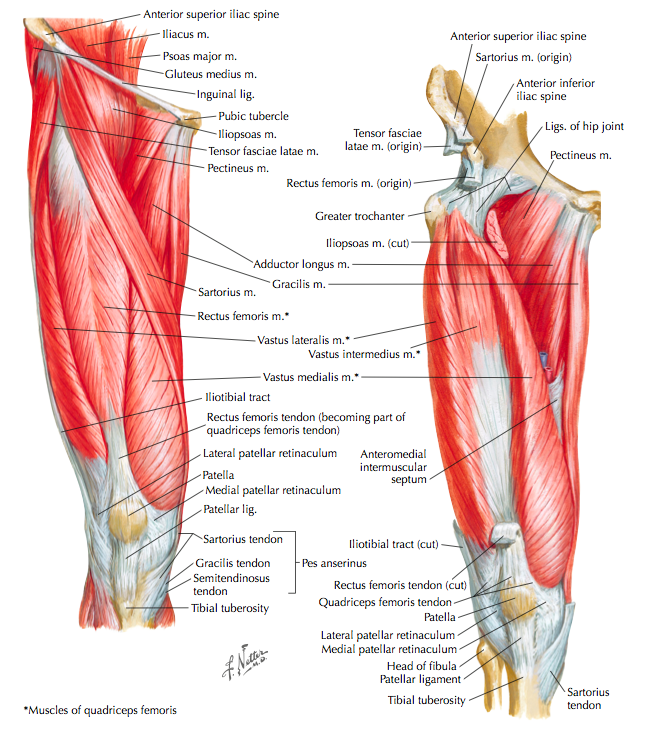
Anterior muscles of the hip and thigh (Cleland, 2005, p. 251)
The adductor synergy
The hip adductor synergy consists of adductor magnus, adductor longus and gracilis (superficial), adductor brevis and pectineus (intermediate), quadratus femoris, and obturator externus (deep).
- Adductor magnus is a powerful hip adductor, extensor and external rotator.
- Adductor longus is a powerful hip adductor and flexor.
- Adductor brevis acts as an adductor and flexor and assists with stabilisation of the pelvis on femur in stance phase of gait.
- Pectineus acts as a flexor, adductor and internal rotator and is thought is assist with control of anterior shear of the femoral head in an abducted position.
The external rotator synergy
The external rotator synergy consists of gluteus maximus, satorius, rectus femoris, adductor magnus, long head of biceps femoris (all superficial system), piriformis and posterior GMed (intermediate system), and quadratus femoris, obturator internus, obturator externus, and gamelli (deep system).
Some interesting functional facts (Grimaldi, Richardson, Durbridge, et al., 2009)
- Walking = primarily gluteus medius (GMed).
- Jogging = half GMed and UGM.
- Running = equal split between GMed, UGM and LGM (active hip extention during swing phase).
- Forward lunge (trunk forward position) = LGM
- Squats = both UGM and LGM
- Mid-late stance phase = Anterior portions of GMed
A clinical example
An brief example of how I have applied the information to clinical practice:
Recently I had a patient with right sided sacro-iliac joint pain caused by reduced force closure.
Subjectively she reported immediate pain with standing and a further increase in pain with walking, going up stairs, lifting her children, and lying on her right hand side.
On physical examination her pain was reproduced with lumbar flexion, single leg stance, and she had pain on all of Laslett's pain provocation tests, pain and reduced loading capacity with the stalk test and the active straight leg raise test, and tenderness on palpation of her long dorsal ligament. Lumbar palpation was painfree and hip joint clearing tests unremarkable.
So I decided to look at her gluteal function further to assess the impact on force closure around the SIJ. Specifically I was interested in the function of gluteus maximus.
On assessment there was wasting in both her upper and lower gluteus maximus. Functionally she had too much pain in standing to perform gluteal retraining. I was able to individually assess the contribution of UGM and LGM to force closure by activating UGM with isometric abduction in side lying and LGM with isometric hip extension in 4 point-kneeling.
The patient was able to individually activate different muscle portions in a painfree position and develop a better understanding of how to use them. Each muscle was activation isometrically for 5 second holds x 5 repetitions. On reassessment her standing pain was resolved and her single leg stance painfree. This was associated with increased tone throughout the affected gluteus maximus.
Conclusion
Having a better understanding of muscle function around the hip has helped me with my assessment of patients. Specifically it has changed:
- The way I assess muscle strength and control.
- The way I interpret movement patterns observed during functional tasks.
- It has also allowed me to adapt exercises and assessments to still specifically target synergies while tailoring my approach to suit the patient's level of function, level of severity and irritability.
Below is a review of the anatomy of the hip and thigh for further reference. You may also be interested in reading Alicia's previous blog on assessment of hip strength and my previous blog outlining the changes in muscle function which occur during hip osteoarthritis.
Sian
References
Cleland, J. (2005). Orthopaedic clinical examination: an evidence-based approach for physical therapists: WB Saunders Co.
Grimaldi, A., Richardson, C., Stanton, W., Durbridge, G., Donnelly, W., & Hides, J. (2009). The association between degenerative hip joint pathology and size of the gluteus medius, gluteus minimus and piriformis muscles. Manual therapy, 14(6), 605-610.
Grimaldi, A., Richardson, C., Durbridge, G., Donnelly, W., Darnell, R., & Hides, J. (2009). The association between degenerative hip joint pathology and size of the gluteus maximus and tensor fascia lata muscles. Manual therapy, 14(6), 611-617.
Grimaldi, A. (2011). Assessing lateral stability of the hip and pelvis. Manual Therapy, 16(1), 26-32.
Retchford, T. H., Crossley, K. M., Grimaldi, A., Kemp, J. L., & Cowan, S. M. (2013). Can local muscles augment stability in the hip? A narrative literature review. J Musculoskelet Neuronal Interact, 13(1), 1-12.
Courtesy of Cleland (2005, p. 250).
(Cleland, 2005, p. 250)
(Cleland, 2005, p. 248)
(Cleland, 2005, p. 248)