Modic changes & Spinal degeneration
Dr. Mark Percy, Specialist Radiologist with MIA Victoria, who previously guided me on the topic of VBI and pre-manipulative screening also spoke with me about Modic changes. Previously I didn't completely understand the clinical significance of this term and why as Physiotherapists we need to consider the implications of this word being written on the radiology report. Dr. Percy explains what we need to know about them.
What are Modic Changes?
Image courtesy of Google Images
Modic changes are a term which is used to describe the changes of the vertebral endplate which are related to spinal degeneration. They are called 'Modic changes' after the author Dr. Modic, who was the first Doctor to identify and classify degenerative endplate changes and marrow changes surrounding the intervertebral disc.
On MRI demonstrates signal intensity changes during the degeneration process, whether it be fat, oedema or sclerosis. Modic changes are thought to be a dynamic process which can change and progress, but no cases have been reported where Modic changes have gone away (Mann, et al., 2014).
On MRI, Modic changes will look like signal alteration in the end-plates parallel to the disc. They are most common in the lumbar spine, and whilst they can occur at any level, they are most commonly observed at L4/5 and L5/S1. Where the changes occur is variable too. Commonly they occur anteriorly, but there are also cases where there is near-complete vertebral involvement (Dr. Percy, 2015).
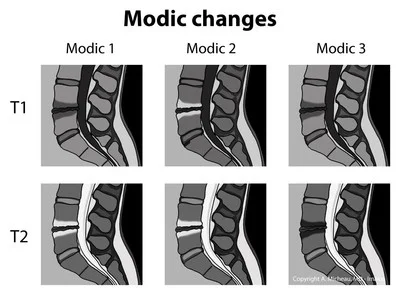
There are three types of Modic changes (Järvinen, et al., 2015; Mann, et al., 2014)
- Type 1 - Represents fibrovascular changes in the subchondral bone marrow such as oedema and inflammation. Type I refers to acute degenerative changes which are often associated with pain. These images will show high signal intensity on T2 and low signal intensity on T1 images.
- Type 2 - Represents replacement of bone with fatty yellow marrow. It can be distinguished with increased signal intensity in both T1 and T2 images.
- Type 3 - Represents the replacement of bone with bony sclerosis where there is little residual marrow. Sclerotic changes will also be visible on XRAY. There is low signal intensity on both T1 and T2 images.
Image courtesy of Google Images
What is the difference between T1 & T2 images on MRI?
MRI has no colour, only shades of grey from bright to dark. When comparing T1 and T2 images try to remember that on T1 fluid is dark, and on T2 fluid is bright. Spinal cord matter and cortical bone are a darker grey on both. Subcutaneous fat is brighter grey on both. The main difference for MRI is the brightness of grey which fluid will reflect. Many pathologies have fluid in them, making them easier to see as you compare each image.
T1 - Cerebrospinal fluid is dark.
T2 - Cerebrospinal fluid is bright.
We use MRI to view changes in the endplate because CT is insensitive to early changes of oedema and fatty replacement. On XRAY, only Type III sclerotic changes can been seen. But with MRI, and especially with the comparison of T1 and T2 images, a lot of information can be gathered about the suspected changes occurring in the spine (Dr. Percy, 2015).
What is the differential diagnosis that radiologists need to consider?
- Disc space infection
- Osteomyelitis
- Malignancy
IS DISC DEGENERATION PAINFUL?
Type I Modic changes are present in 4% of patients undergoing MRI for disc disease. Type II is present in 16% of patients, and Type III is the least common and present in around 1%. The cause of these endplate changes is largely unknown (Luoma, et al., 2009). Modic created a diagnostic system, however, research continues to evaluate what causes these Modic changes to occur, as well as the prevalence and association of these changes with pain.
The relationship of Type I end-plate changes to low back ( discogenic ) pain is controversial. The reported prevalence of Modic Changes with lumbar spine pain is considerably variable between studies (Jensen, et al., 2008). Jensen and collegues (2008) conducted a systematic review on the prevalence and association of Modic changes with back pain and they concluded that although there is an association between MRI changes and back pain, there are also asymptomatic people who display these features on MRI.
Some studies suggest that with increasing age that Type II changes become more prevalent in both the cervical and lumbar spine, describing Modic changes as a dynamic phenomenon (Mann, et al., 2014). It has also been documented that Type I changes can progress to Type II over time.
There are studies that suggest a high presence of Modic Changes with lower back and neck pain but there is uncertainty about it's correlation to high levels of pain (Sheng-yun, et al., 2014) Some studies suggest that type I and II change have a high specificity ( >90% ) but low sensitivity ( 20-30% ) for painful lumbar disc. What this means is that despite the high prevalence of Modic changes, there is a small percentage of people with severe disc degeneration who have persistent and high levels of pain (Takatalo ESJ et al, 2011). There is on the other hand, and large percentage of people (35%) who have disc degenerative changes and no pain. Disc degeneration is an aged related process and not a disease process and therefore does not have to be a painful problem. It can be accelerated in some cases and viewed as a pathology, but generally speaking, many people experience changes which are associated with age alone.
A study by Modic (2005) looked at the prevalence of disc herniation in back pain and radiculopathy, noting two things; that the presence of disc herniation in lower back pain is around 57% and lumbar radiculopathy 65%, but that this prevalence has poor correlation with prognosis. In fact, patients knowing the outcome of the medical imaging was associated with a poorer outcome and lower sense of wellbeing. How many patients have you met that say their problem is a 'bulged' or 'slipped disc'? People carry these labels with them for long periods and often have negative views about what these terms mean about their prognosis and future.
A study by McCullough et al (2012) explored the prevalence of MRI findings in people without back pain. 237 reports were taken and 30% of these reports were accompanied with the statement about normal morphological changes seen on scans. The results found that when patients/clinicians were provided with epidemiological data on the normal spinal changes seen on MRI, they were less likely to receive narcotic prescription.
Disc degeneration was seen in 91% of people, disc height loss in 56%, disc bulges in 64%, disc protrusion in 32%, and annular tears in 38% of people. The findings of these studies reinforce to clinicians that MRI results for the spine must be viewed with caution and related back to the clinical presentation.
So what does all this information mean for physiotherapists? Don't be anti-scanning…. we often find useful and valuable information from scan. It is not the scan or the radiologist that leads to poorer outcomes or the nocebo effect, it is the way we educate patients and give them information about the results. Take time to carefully educate them about these MRI features and ensure they understand correctly.
Sian
References:
Luoma, K., Vehmas, T., Grönblad, M., Kerttula, L., & Kääpä, E. (2009). Relationship of Modic type 1 change with disc degeneration: a prospective MRI study. Skeletal radiology, 38(3), 237-244.
Järvinen, J., Karppinen, J., Niinimäki, J., Haapea, M., Grönblad, M., Luoma, K., & Rinne, E. (2015). Association between changes in lumbar Modic changes and low back symptoms over a two-year period. BMC musculoskeletal disorders,16(1), 98.
Jensen, T. S., Karppinen, J., Sorensen, J. S., Niinimäki, J., & Leboeuf-Yde, C. (2008). Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain.European Spine Journal, 17(11), 1407-1422.
Mann, E., Peterson, C. K., Hodler, J., & Pfirrmann, C. W. (2014). The evolution of degenerative marrow (Modic) changes in the cervical spine in neck pain patients. European Spine Journal, 23(3), 584-589.
McCullough, B. J., Johnson, G. R., Martin, B. I., & Jarvik, J. G. (2012). Lumbar MR imaging and reporting epidemiology: do epidemiologic data in reports affect clinical management?. Radiology, 262(3), 941-946.
Modic, M. T., Steinberg, P. M., Ross, J. S., Masaryk, T. J., & Carter, J. R. (1988). Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology, 166(1), 193-199.
Modic, M. T., Obuchowski, N. A., Ross, J. S., Brant-Zawadzki, M. N., Grooff, P. N., Mazanec, D. J., & Benzel, E. C. (2005). Acute Low Back Pain and Radiculopathy: MR Imaging Findings and Their Prognostic Role and Effect on Outcome 1. Radiology, 237(2), 597-604.
Sheng-yun, L., Letu, S., Jian, C., Mamuti, M., Jun-hui, L., Zhi, S., ... & Zhao, F. (2014). Comparison of Modic Changes in the Lumbar and Cervical Spine, in 3167 Patients with and without Spinal Pain. PloS one, 9(12), e114993.