Frozen shoulder - to treat or not to treat? What Physiotherapy exercises are used to treat adhesive capsulitis of the shoulder?
Christine and David at graduation 2013
Christine Frith, Senior Musculoskeletal Physiotherapist at St Vincents Hospital, Melbourne, Australia, shares her ideas about the management of the frozen shoulder. For many years Christine has been a supervisor for both undergraduate and masters students, in fact she played a large role in my training during my masters degree. I've learnt so much from Christine. She has a special interest in shoulder management and heavily involved in the shoulder clinic at St V's. I asked Christine what she would share with Physiotherapists about shoulders if given the chance... and this is her message.
Introduction
Recently a newly graduated physio told me
“Frozen shoulders....well there is no evidence for physiotherapy management with frozen shoulders, so I give them an exercise program and don’t need to treat them. End of story...”
It made me wonder... is that true? My clinical experience tells me otherwise, so I thought I would review a little of the evidence and share it with you.
(Arthroscopic view of frozen shoulder on the right Pain> stiffness)
- Frozen shoulder or adhesive capsulitis is a problem of spontaneous onset of pain and progressive stiffness with marked loss of function.
- It is caused by inflammation of the joint capsule and synovium which is followed by fibrosis, scaring and contracture in the capsuloligamentous complex (Donatelli, et al., 2014).
- It results in global loss of passive and active range of movement at the glenohumeral joint (GHJ), most commonly painful and stiff ER is the most restricted movement.
- The incidence is between 2-5% of people and more common in the over 50s age group. Those with diabetes, prolonged shoulder immobilisation and systemic disease (hyperthyroidism, hypothyroidism, cardiovascular disease and Parkinson's disease) are at higher risk. In fact, some statistics suggest frozen shoulder occurs in 19% of the diabetic population.
- Initial phase: Pain > stiffness, with inflammation, substance P, neovascularisation.
- Later phase: Stiffness > pain, scarring and contracture formation (like Duputyren’s).
- Average duration is 12-42 months (but other papers stated ongoing dysfunction at 7 years in 50% of people diagnosed). How many of our patients are able to put their lives on hold for 1-3 years?
- Diagnosis is often based on the loss of ER active and passive range (at 30, 45 and 90 degrees abduction) and can occur in the absence of other diagnostic findings (usually x-ray).
- Patho-anatomically there is a reduction in GH intra-articular volume from 15-35cc to 5-6cc but no adhesions to the humerus.
- Clinically:
- There may be trigger point development and loss of extensibility in shoulder muscles and fascia, particularly subscapularis, pectorals, latissimus dorsi and posterior cuff muscles that will respond to soft tissue treatments (Page., 2010).
- There will be altered movement patterns (e.g. shrug sign) often related to glenohumeral capsular tightness and relative weakness in the lower trapezius muscles relative to upper trapezius, serratus anterior and infraspinatus (Page., 2010).
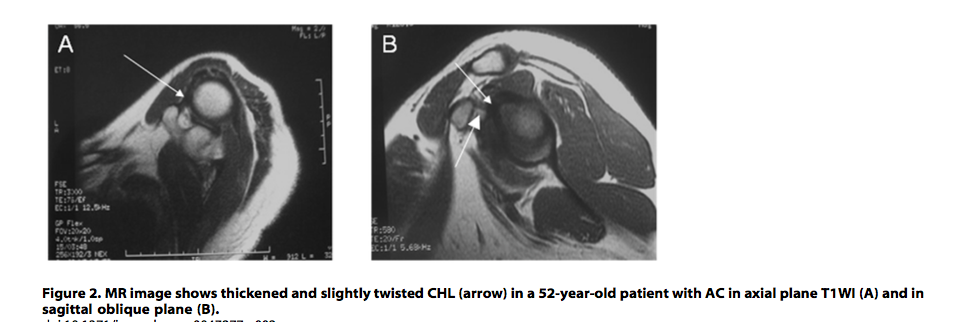
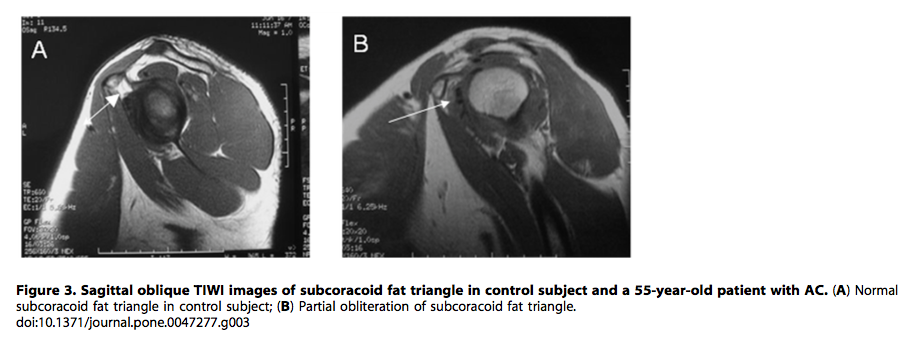
- Diagnostically, thickening of the coracohumeral ligament (CHL) and the capsule at the rotator cuff interval and complete obliteration of the fat triangle under the coracoid process have been shown to be the most characteristic MR findings seen with AC. (Even though most of the patients I see don’t have this test, it is interesting to know what can be visualised).
- Patients with frozen shoulder for 2-3 years need re-screening by a doctor/physician including blood tests to screen for poorly controlled diabetes or undiagnosed diabetes or inflammatory disease.
"Interventions for patients with adhesive capsulitis remains controversial and poorly understood" (Donatelli, et al., 2014, p.4)
- Heat reduces neovascularisation and there is some evidence for short wave diathermy – if you are lucky enough to have one.
- There is strong evidence that Corticosteroid injections ease painful inflammation in the short term and the effects are improved when combined with physio. The Hydro-dilatation with or without corticosteroid combined with physiotherapy rehabilitation has moderate evidence in the medium term (Lewis., 2014).
- There is some evidence for physiotherapy mobilisations into resistance over mobilisations into low resistance for improving function but not pain.
"A time-honored technique in shoulder therapy is the low-load prolonged stretch and static progressive stretch ... This technique requires placing the scarred or contracted tissue under stain at the end range of available motion with the intent to incrementally increase the mobility of the glenohumeral joint with the expectation of plastic remodelling of the periarticular connective tissues to ultimately improve active and passive range of motion of the shoulder" (Donatelli, et al., 2014, p.4).
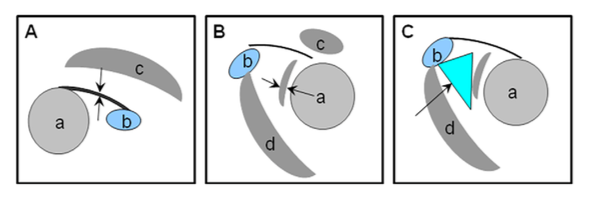
MRI can be used to study the characteristics of the thickness of the coracohumeral ligament (A) on a T1 image, the thickness of the capsule (B), and the thickness/presence of the subcoracoid fat triangle (C), which have shown to be characteristics of adhesive capsulitis on MRI (Zhao, et al., 2012, p.2).
- a = Humeral head
- b = Caracoid notch
- c = Supraspinatus
- d = Coracobrachialis
(Zhoa et al, 2012, p. 3)
Top image is an MRI of a shoulder with adhesive capsulitis in the axial and sagittal and oblique plane, indicating thickening of the coracohumberal ligament. Bottom image shows two MRIs, one of a healthy shoulder with the subcoracoid fat triangle, and the other of a shoulder with adhesive capsulitis with loss of the subcoracoid fat triangle.
(Zhoa, et al., 2012, p. 4)
Case study 1
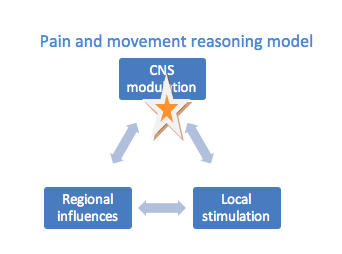
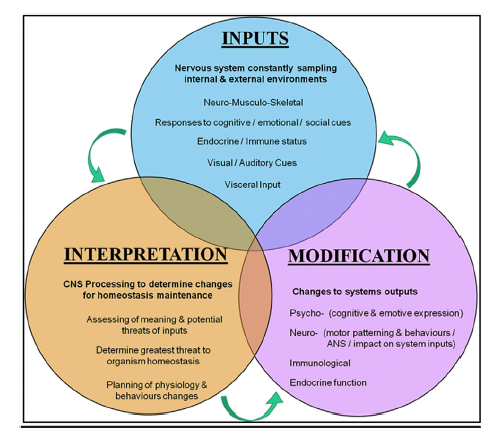
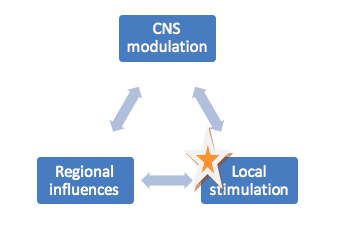
A 52 y.o. woman was recently referred to me with adhesive capsulitis for >2 years and a past social history of an abusive husband and reported emotional distress and vulnerability. The pain presentation included a dominance of a non-mechanical pain triggers associated with signs of (almost) ‘neglect’ of her right upper limb. I charted her pain sources on Day 1 (right) refer to the orange star.
CNS modulation was the dominant driver for this person’s pain on that day and therefore education, stress management, body awareness, graded motor imagery and graded exposure which all tackle descending inhibition of pain might be useful techniques with this person initially. She was already having counselling and multiple interventions from her medical team and re-screening for inflammatory disorders. (Of interest there were no signs of adhesive capsulitis on her shoulder MRI). This is not the ideal person to treat with physiotherapy as the primary driver was not local stimulation. If you'd like to read more about central processing and it's role in pain processing, I'd recommend reading The Pain and Movement Reasoning Model: Introduction to a simple tool for integrated pain assessment by Jones and O’Shaughnessy (2014). This is a representation of that model.
(Jones & O' Shaughnessy., 2014, p. 271)
Case study 2
In contrast, another person Mr U, 60 y.o. man, is a self-employed cafe owner with a 6 month history of adhesive capsulitis. He had a mechanical shoulder presentation and had tried a hydro-dilatation 2 months ago with no improvement in symptoms and no physio. Charting his pain and movement responses suggested that his pain is largely driven by local structures that are more ameniable to manual therapy and exercise based physiotherapy.
He was reluctant to have another hydro-dilatation as he thought the procedure made him worse. This was despite the fact there is moderate evidence that hydro-distension with physiotherapy helps in the short term and can be repeated one month later if resistant to change (Favejee., 2011).
He presented with shoulder stiffness more than pain and reported problems stacking the shelves in the cafe at shoulder height (6/10 and stiff) and pain (7/10) when rolling onto the right shoulder. His pain was mechanical (very capsular) with no change in range or pain with scapula re-positioning tests during flexion (80) or abduction (60). He had mild improvement in shoulder passive ER range (from 10 to 15 degrees) with AP glide on the GHJ during the movement (Johnson., 2007). There was mild scapula protraction on the right side with reduced endurance on right when assessed in prone but this was a minor factor in the presentation.
He was motivated to try a rehab program of exercise while waiting to see a shoulder specialist. He was not reporting any undue stress or concerns, other than being busy at work and not wanting to attend physio very often.
Exercises for improving GHJ range of movement
There are seven stages in restoring rotation range of movement (Donatelli, et al., 2014, p. 9).
- Passive external rotation of the GH joint in the adducted position or at 0 degrees of abduction in the plane of the scapula (POS) provides strain to the lower and middle fibers of the subscapularis.
- Passive external rotation of the GH joint at 30 degrees of abduction in the POS provides strain to the upper, middle, and lower fibers of the subscapularis.
- Passive external rotation of the GH joint at 45 degrees of abduction stretches the subscapularis and middle GH ligament.
- Passive external rotation of the GH joint at 90 degrees of abduction stretches the inferior ligament complex..
- Passive internal rotation of the GH joint at 30 degrees of abduction in the POS provides stretch to the superior portion of the posterior capsule.
- Passive internal rotation of the GH joint at 30 degrees of extension and internal rotation provides stretch to the inferior portion of the posterior capsule.
- Passive flexion and internal rotation of the GH joint at 90 degrees of abduction provides general stretch to the posterior capsule (This position can be adjusted depending on pain and joint restrictions to 60 or 40 degrees).
One key element for these stretches to be effective is selecting the appropriate amount of tensile load. "An insufficient amount of stress will have no therapeutic effect, where as an excessive dose will produce complications such as pain and inflammation. Three factors should be considered when calculating the prescribed amount of force delivered to soft tissues: intensity, duration and frequency" (Donatelli, et al., 2014, p. 4).
I began with a series of sustained stretches into rotation that I had read about recently using Shoulder ER in 3 positions to stretch the tightened bands in the capsule + coracohumeral ligament (and possibly the associated muscles) within the scapula plane (Donatelli, et al., 2014). The first is ER in the scapula plane, the second is in approximately 35 degrees elevation, and the third approximately 70 degrees. Holding each position for 2 minutes with a can of beans 250 gram, or in this case an orange. I explained that the prolonged stretch is the key; ideally repeated 3-4 times per day - progressing to 5 minutes stretches in each position over 3 weeks. I advised that "Mild discomfort during the stretches is essential but not moderate pain".
Within the session, during each stretch, I added in passive GH joint sustained glides, to reduce the discomfort of the stretch e.g. AP glide or Inferior glide of GH or combination of both. I usually hunt around to find the best angle during each stretch and explored the associated muscles for tightness and trigger points.
At home I suggested a heat pack over the anterior shoulder to see if that improved the pain prior to or even during the stretching and advised to use a tennis ball in a sock to massage the posterior cuff against a wall for 5 minutes per day. (This pictures uses a spiky ball)
Day 2 (two weeks later)
Mr U was 10 better into Flexion actively, I progressed the weight to .5 kg and the starting position of the stretch to approach the hand toward head position with elbow on a bolster. He was also doing some old exercises including the Door stretch for ER. (I didn't have a 0.5kg weight for the photo but this jam jar is a great alternative)
Day 3 (three weeks later)
Mr U was very happy with the improvements. He could now see a difference in the shoulder at work (Flexion 110), but stated that his shoulder was ‘not normal’. I progressed the starting positions of the old stretches to push further into range and added in 2 new stretches. Beginning with 2 minutes and progressing to 5 minutes as able over 3 weeks, following the same dosage as the other exercises. The first was hand near hear in prone with a bolster under the shoulder and the second was HBB in prone with a bolster under the shoulder.
I will wait to see how he presents next visit.
What you might notice from this treatment approach is that rotation was the primary focus rather than restoring elevation. Forcing the shoulder into elevation in the hope of gaining more elevation can actually lead to more pain, increased inflammation, which results in further formation of scar tissue (Donatelli, et al., 2014). Hopefully this blog provides alternative strategies for managing restricted range of movement in patients with adhesive capsulitis.
Another aspect that needs to be considered is dosage. Articles presenting treatment ideas for adhesive capsulitis often present different dosages. The ones that I follow are guided by the work of Donatelli and colleagues (2014). In their article they do review other possible dosages, and if you're looking to read about them further, I'd recommend starting with that paper.
My management of patients with adhesive capsulitis is somewhat limited by the lack of money patients have to spend on splints and hydro-dilatations and the lack of electrotherapy modalities that I can access at work in a public Hospital, however having said that, 90% of patients in my clinic have some improvements in their range and function within 2 months.
I am sure that everyone has success with the majority of frozen shoulder patients in the Stiffness > pain phase where local nociceptors are the main driver of the problem. It is not clear from the literature what particular stretches should be prescribed but if progress stalls; why not experiment with these stretches and feedback to the blog about your results?
Christine & Sian :)
References:
Buchbinder, R., Green, S., Youd, J. M., Johnston, R. V., & Cumpston, M. (2008). Arthrographic distension for adhesive capsulitis (frozen shoulder). The Cochrane Library.
Donatelli, R., Ruivo, R. M., Thurner, M., & Ibrahim, M. I. (2014). New concepts in restoring shoulder elevation in a stiff and painful shoulder patient. Physical Therapy in Sport, 15(1), 3-14.
Favejee, M. M., Huisstede, B. M. A., & Koes, B. W. (2011). Frozen shoulder: the effectiveness of conservative and surgical interventions—systematic review.British journal of sports medicine, 45(1), 49-56.
Johnson, A. J., Godges, J. J., Zimmerman, G. J., & Ounanian, L. L. (2007). The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. journal of orthopaedic & sports physical therapy, 37(3), 88-99.
Jones, L. E., & O'Shaughnessy, D. F. (2014). The Pain and Movement Reasoning Model: Introduction to a simple tool for integrated pain assessment.Manual therapy, 19(3), 270-276.
Lewis, J. (2015). Frozen shoulder contracture syndrome–Aetiology, diagnosis and management. Manual therapy, 20(1), 2-9.
Page, M. J., Green, S., Kramer, S., Johnston, R. V., McBain, B., Chau, M., & Buchbinder, R. (2014). Manual therapy and exercise for adhesive capsulitis (frozen shoulder). The Cochrane database of systematic reviews, 8.
Zhao, W., Zheng, X., Liu, Y., Yang, W., Amirbekian, V., Diaz, L. E., & Huang, X. (2012). An MRI study of symptomatic adhesive capsulitis.