Screening for VBI & CAD in patients with cervical spine pain
Introduction
In 2018, the Australian Physiotherapy Association published revised clinical guidelines for safe practice of manual therapy on the cervical spine. This topic of “safety” and in particular, identifying patients presenting with signs of VBI and CAD (vertebrobasilar insufficiency and cervical arterial dissection) is a topic I’ve come back to many times throughout my career. Each time I read the literature updates, the same message is made very clearly.
Although both VBI and CAD are fairly rare conditions, their primary symptoms are common reasons that people seek treatment from physical therapists, namely neck pain, headaches and dizziness.
The impact of these conditions is serious and potentially life threatening.
We rely heavily on our subjective examination to guide us to make relevant adjustments to our physical examination and management.
VBI and CAD are contraindications to manual therapy, specifically end range mobilization and manipulation.
This is a very serious topic in our profession, yet I have been fortunate enough not to experience firsthand. Just as we revise our CPR training every few years, frequently revisiting this topic is important to stay current in knowledge and sharp in our clinical reasoning skills. This blog is just that, a revision of the current recommendations for the identification of CAD and VBI.
Recent publications
Firstly, I want to highlight 2 very helpful guidelines published by the APA (Thomas, Shirley & Rivett., 2017). The first was a review of the vascular considerations in patients with neck pain and the second was best practice recommendations for the use of high velocity thrust techniques.
https://australian.physio/sites/default/files/tools/NAT023_APA_VBI_FACTSHEET.pdf
https://australian.physio/sites/default/files/tools/APA_VBI_A4_factsheet_A_v10.pdf
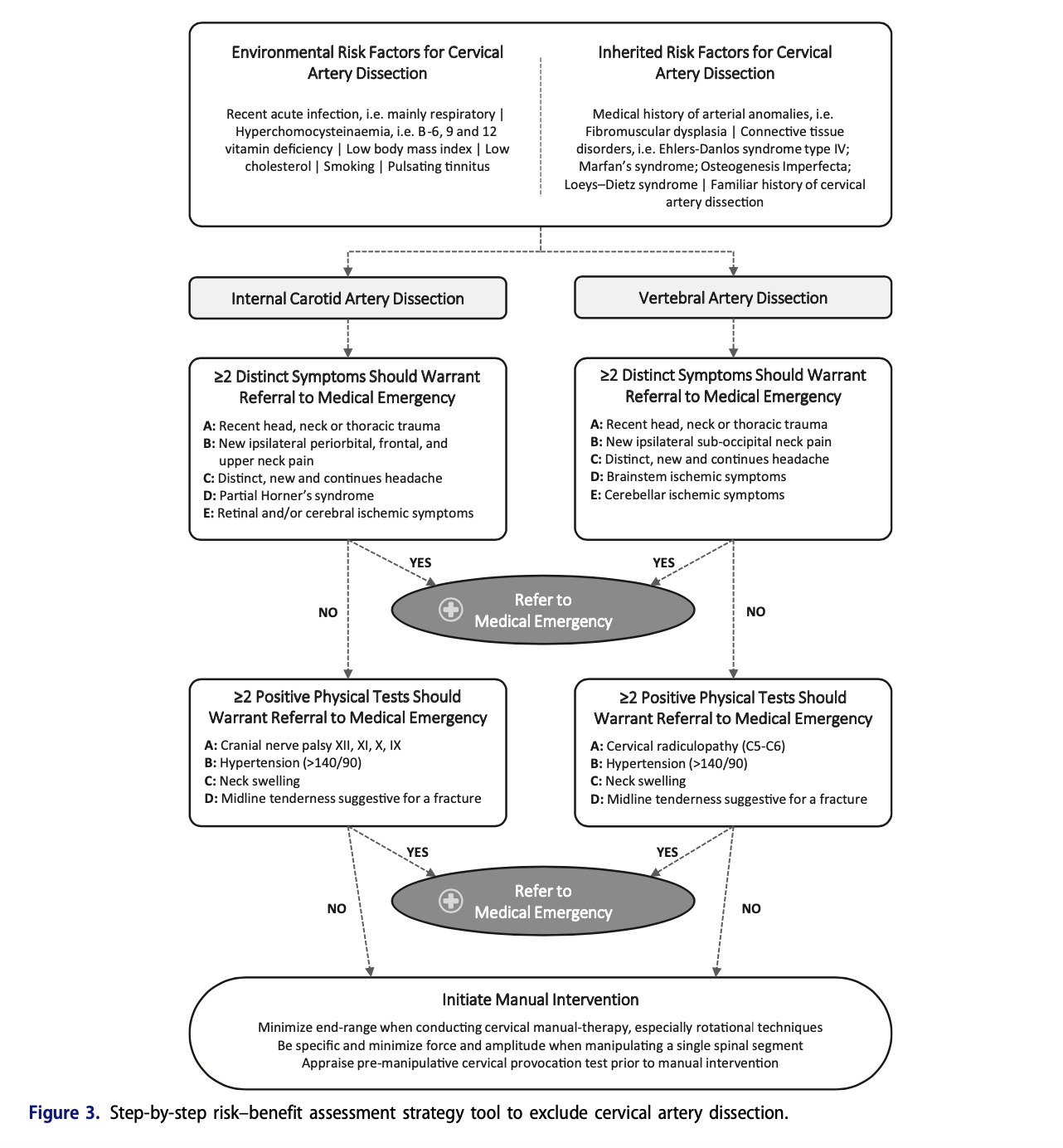
Secondly, I want to reflect on a current paper from 2019, published by Chaibi & Russell. These authors provide a risk-benefit assessment tool to assist in the clinical reasoning for patients with cervical pain and headaches. I found this paper complimented the APA guidelines and expanded on the debate around causality between manipulation and adverse events.
It cannot be emphasized enough just how important the subjective assessment is in guiding our clinical reasoning to identify red flags and suspect serious pathology.
Patients with VBI will commonly complain about dizziness.
Patients with CAD will present with sudden unfamiliar headache and upper cervical neck pain.
Neither of these conditions follow common patterns of musculoskeletal conditions. (How will you know? From asking the right questions about severity, intensity and nature).
There is no conclusive evidence around causality between manipulation and the progression of VBI/CAD, only case studies with poor methodology.
Positional testing for VBI can be provocative and should be selected carefully.
Signs & symptoms of CAD
Environmental risk factors to consider are acute respiratory infection, low BMI, low cholesterol, smoking, tinnitus.
Medical history of arterial anomalies and connective tissue disorders.
Less than 55 years of age
Acute, sudden and unfamiliar pain/headache in the ipsilateral, frontal, periorbital upper neck region.
Minor trauma
5D’s and 3N’s
Diplopia – and other visual disturbances such as blurred vision or transient hemianopia
Dizziness or vertigo
Drop attacks
Dysarthria
Dysphagia
Nausea and vomiting
Nystagmus
Other neurological signs
This list may be familiar to you but that last statement I actually have often overlooked and assumed the authors meant neurological signs of and central vascular issue. After reading the recommendations again and in combination with Chaibi & Russells paper, I now realize that this statement is referring to neurological signs related to the cranial nerve assessment (listed below)
Signs & symptoms of VBI
Previously I have written about VBI in this blog in much greater detail. But as a recap of the signs and symptoms, the following list of symptoms or signs is taken from the APA clinical guidelines for the assessment of VBI in the management of cervical spine disorders (Rivett, Shirley, Magarey, & Refshauge., 2006). I have referred to this document many times to remind myself of the contraindication/precautions to manipulation of the cervical and lumbar spine.
Dizziness and ipsilateral and sub-occipital neck pain
Family history of VBI or arterial anomalies
Medical history of connective tissue disorder
Age generally >65 years old
Risk factors of high blood pressure, high cholesterol
Previous diagnosis of VBI or previous possible VBI episode provoked by cervical manipulation
5D’s and 3N’s
Other symptoms: Lightheadedness, fainting, disorientation and anxiety
Tinnitus or hearing disturbances
Fascial or intra-oral anaesthesia or paraesthesia
Pallor, tremors, sweating
Any of these symptoms provoked by neck positions (sustained end range rotation of at least 10 seconds for VBI specifically)
As you can see from the two lists, it is much more than a check list of questions. It is a meaningful inquiry about symptoms which represent altered cerebral bloodflow. Both Chaibi & Russell (2019) and the Australian Physiotherapy Association guidelines (2018) suggest to include the following in your physical examination (in addition to your routine examination).
Blood pressure
Lower cranial nerve assessment (IX, X, XI, XII)
IX Glossopharyngeal nerve – dysphagia, dysarthria, taste sensation on the posterior 1/3 of the tongue.
X Vagus nerve – gag reflex and voice changes (hoarseness)
XI Accessory nerve – bilateral shrug (upper trapezius) and bilateral neck rotation (sternocleidomastoid)
XII Hypoglossal nerve – tongue weakness in protrusion, lateralization, retraction and elevation.
Neck swelling
Midline tenderness (suggestive of fracture)
Upper limb neurological examination (cervical radiculopathy)
Horner’s syndrome
Aka oculosympathetic paresis
Ipsilateral symptoms
Miosis – constricted pupil
Ptosis – droopy eyelid
Anhydrosis – reduced sweating
(Chaibi & Russel., 2019, p.123)
Conclusion
This list may be familiar to you, but often I have overlooked the 3rd N – other neurological symptoms that may represent a central vascular issue. After reading the recommendations again in combination with the article from Chaibi & Russell, I now realize that screening is more than the 5D’s and 3N’s. It also should include blood pressure, lower cranial nerve assessment and assessing for Horner’s syndrome.
Being thorough and intentional with the questions we ask during our patient history, is a part of clinical reasoning that I am continually developing. Always asking myself why am I asking this question, what do the answers mean, can I clarify the information further to best direct my assessment and management. As we all know, directing a conversation and conducting an interview isn’t always as simple as asking the right list of questions. We often get side-tracked by the story our patient’s want to tell. So, from time to time, I find it a grounding experience to revise the purpose of the subjective examination and remind myself of the responsibilities each clinician holds in ensuring the patient is heard and that the right questions are asked. I hope you too find this blog a useful refresher of the current EBP for CAD and VBI assessment.
Sian
Other blogs that may interest you
Vertebrobasilar arterial insufficiency
Cervicogenic dizziness & sensorimotor dysfunction
Assessment of cervicogenic dizziness
Differential diagnosis of dizziness
References
https://australian.physio/sites/default/files/tools/NAT023_APA_VBI_FACTSHEET.pdf
https://australian.physio/sites/default/files/tools/APA_VBI_A4_factsheet_A_v10.pdf
Refshauge, K. M., Parry, S., Shirley, D., Larsen, D., Rivett, D. A., & Boland, R. (2002). Professional responsibility in relation to cervical spine manipulation. Australian journal of Physiotherapy, 48(3), 171-188.
Rivett, D., Shirley, D., Magarey, M., & Refshauge, K. (2006). Clinical guidelines for assessing vertebrobasilar insufficiency in the management of cervical spine disorders. Australian physiotherapy association.
Van Tulder, M., Becker, A., Bekkering, T., Breen, A., Gil del Real, M. T., Hutchinson, A., ... & Malmivaara, A. (2006). Chapter 3 European guidelines for the management of acute nonspecific low back pain in primary care. European Spine Journal, 15, s169-s191.