The Tetris effect
This case presentation is a follow-up to the previous blog series about lateral epicondylalgia (LE) assessment and treatment. LE is a common condition which is easy to recognize and often difficult to treat but after researching for the previous blogs, I was excited to translate my new learning to a patient with acute and severe lateral elbow pain.
Why this patient was so interesting to me is that the treatment advice and technique which made the most impact wasn't the most research element of this condition. There is one key area of physiotherapy treatment that is unique among us all, and when it is given to a patient in a way that is meaningful and impactful for them, it's power in recovery is unmeasurable. This component is the part we most commonly overlook or leave until the end of our sessions when time is scarce, but is the most important part to include - patient education.
Before I give away the ending, let's find out more about this person's problem...
Introducing Mrs. P
Mrs. P was a 49 year old female who presented with a 3 week history of constant right lateral elbow pain which was worsening in nature. This was the 3 major episode within a year of the same elbow pain and the worst so far. She had not previously sought out treatment and the pain usually resolved within a few days. When I met Mrs. P two things stuck me immediately; her kind compassionate persona and her inability to extend her arm to shake my hand. She tried to support her elbow with her left arm and I knew as her hand was limply placed in mine that a firm handshake was completely out of the question.
Her pain was located over the lateral epicondyle and radiated from the elbow down the back of the forearm into the wrist. It began in the elbow but was so severe in the wrist she had started to sleep and work with a wrist splint on to prevent any active movements. The main aggravating movements were reaching for objects, opening doors, holding onto the steering wheel, picking up her drink bottle and using the mouse at work.
Her pain was a constant 6-8/10 in severity at the region of the elbow and when she performed the movements above, there was pain and tingling from her elbow into her wrist. Ibuprofen had a minimal effect and she didn't know what to do.
On physical examination:
- Her grip was 20% of the left side and limited by pain in the wrist and elbow.
- Resisted wrist extension and 3rd finger extension were pain inhibited.
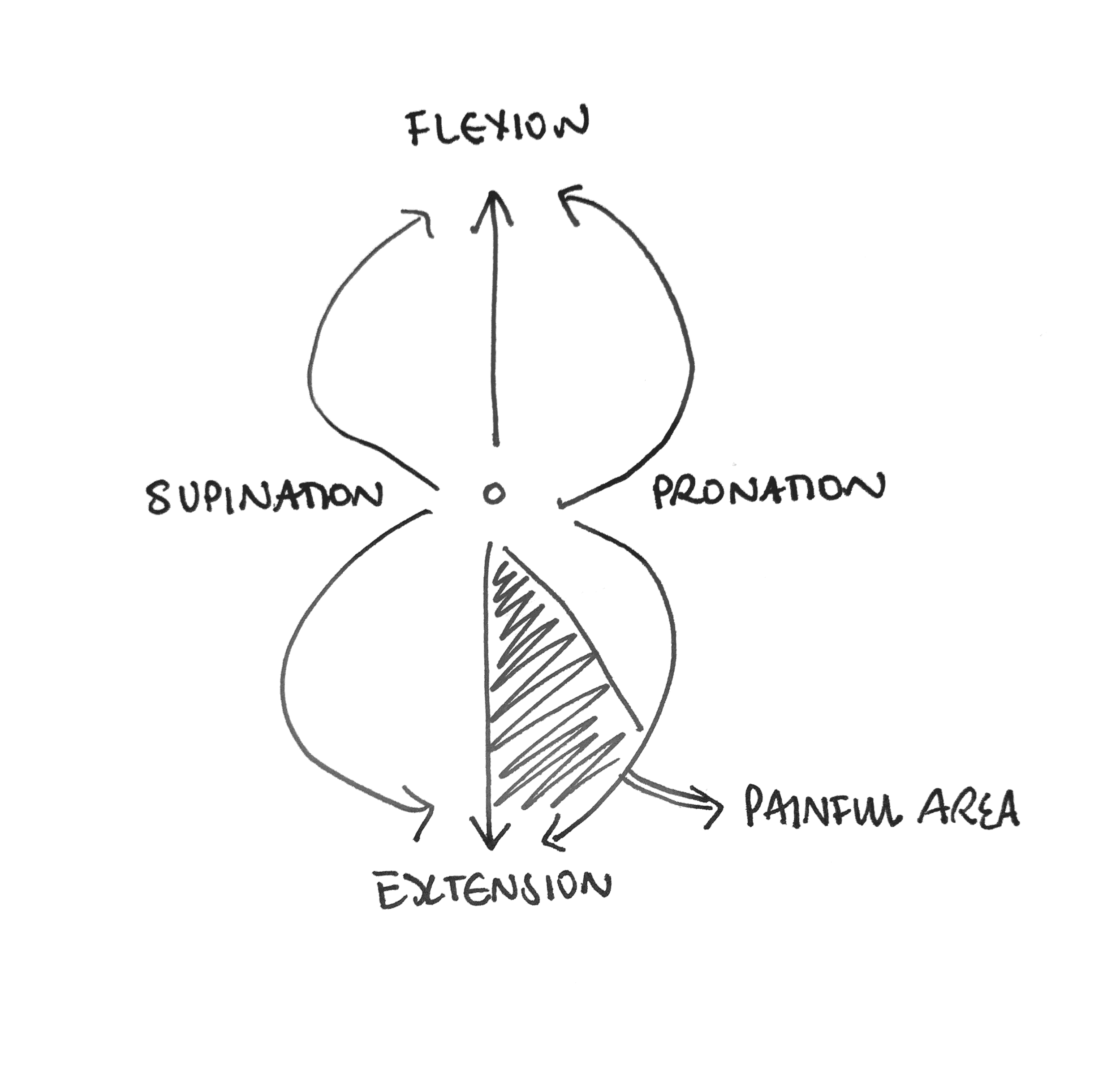
- Elbow PROM was limited in the last 20 degrees of extension and worse with forearm pronation than supination.
- There was tenderness on palpation over the lateral epicondyle, forearm extensors but not over the wrist.
- Overt (positive) radial nerve neurodynamic test which was initially limited by elbow PROM and not able to be clearly tested until day 3.
- Reduced glenohumeral horizontal abduction and abduction/external rotation but tightness through the front of the shoulder/chest.
- Cervical AROM was not limited from L to R but the patient did have a past history of recurrent episodes of neck pain and stiffness.
- Wrist PROM was pain free if tested in elbow flexion and there was no tenderness on palpation.
Sound like LE with some cervical and neurodynamic and postural components thrown in there? I thought it seems pretty text book in presentation and was excited to used my treatment strategies which I had previously learnt.
Day 1 treatment involved a manual lateral ulna glide (without seatbelt) with the patient performing a mobilization with movement (MWM) of tennis ball squeezes in full elbow extension and supination. There was a marked reduction in pain during the treatment and her grip was 2/10 pain severity after treatment. The patient was surprised to see how movement and grip training (both of which had been so painful) had been used in a modified way to improve her resting pain. She was curious and asked me:
Can I move it?
Should I move it even though it hurts so much?
Motion is lotion
At this point in the first session my response to such questions would normally be yes, movement is essential for recovery but take care with your painful direction which is extension/pronation.
For some reason however, maybe because she asked me while I was still holding onto her arm, I decided to show her. This video is captured on an asymptomatic elbow but shows how I move through combined elbow range in my passive movement assessment. What you can see is that even though the elbow joint proper is mostly viewed as a hinge joint, when combined with forearm pronation and supination it has a much larger and circular range available. What I was able to show Mrs. P is that she has full elbow flexion with both pronation and supination, full elbow extension in supination and only a small part of her overall elbow movement was impacted at this stage (combined extension/pronation). Instead of the patient then focussing on the movement that increased her pain, she realized how much unrestricted movement was non-provocative.
I realize that this image is not a normal depiction of a movement diagram of the elbow but it helped both myself and my patient understand where the the region of restriction was and show Mrs. P how much available active movement was still available for her to use in her recovery to maintain and progress her exercises. This image was a guide to show Mrs. P how to maintain her current flexibility and monitor change in her range of movement.
Each session the area in 3D space attributed to painful or limited movement reduced and instead of focussing on the fact that end range extension with pronation and overpressure was painful, each day she saw her progress and was encouraged to keep moving.
This was difficult to document yet powerful to use.
It helped Mrs. P see small changes towards the larger goal of painfree movement and allowed her to monitor progress rather than avoiding the painful part of the quadrant. At the end of her treatment her movement looked like this video. I call these seaweed movements because they are creative and flowing like seaweed moving continuously in water. Essentially these are combined active movements through the wrist, elbow and shoulder with some neurodynamics blended in too.
The tetris effect
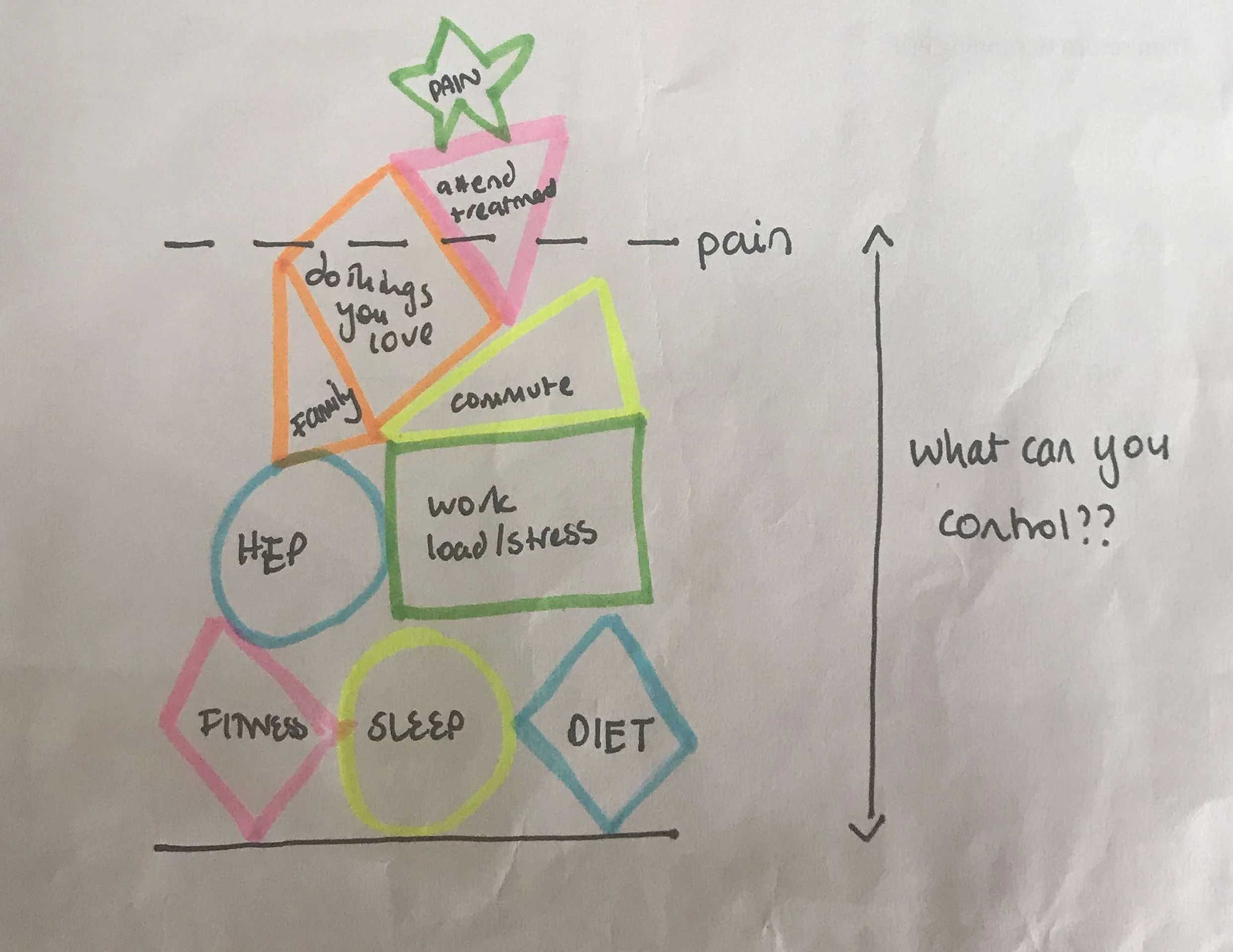
Butler & Moseley describe the tissue tolerance line and pain line in their book Explain Pain. I often discuss this concept with patients who have both acute and chronic pain. This concept is used to explain that often there is a buffer zone between the point at which we feel pain and the point where actual tissue damage occurs, with the tissue tolerance line being higher. What I pay particular focus on is explaining the space between these two points to emphasize that pain does not always mean we are causing further tissue damage. From this point I then go on to discuss how we can understand where the pain line is and what triggers it, which leads me onto a concept I describe as the tetris effect. This is something I have developed over time to discuss all of the contributing factors that are involved in each person's pain experience.
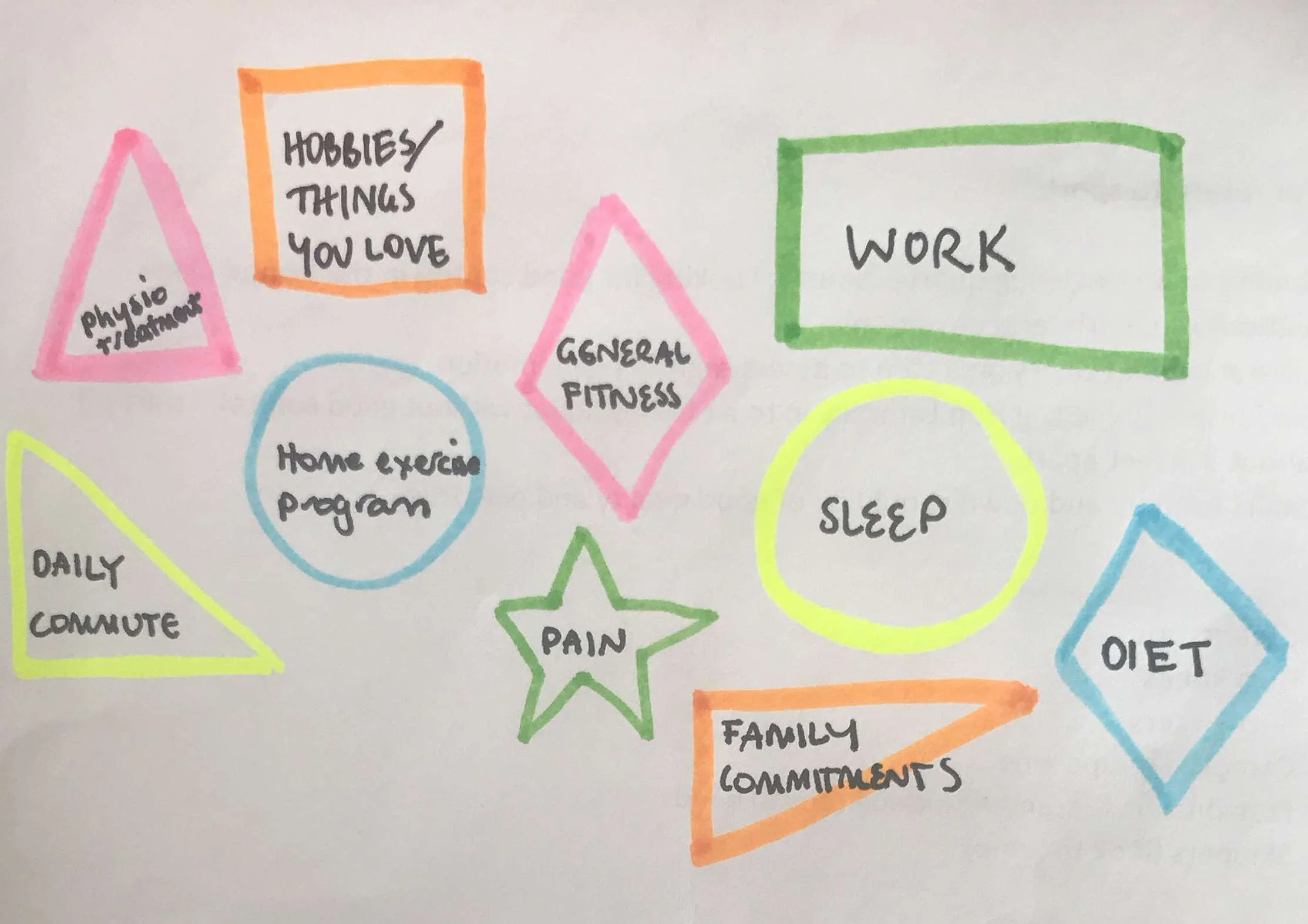
You can call these life's pillars or life's pebbles, what ever analogy you use, we all have to fit it in to make it work. These same shapes occur in pain production, control and management. If you can find the balance, you will stay below the flare up line. From here I explain my tetris theory like this...
First you need to identify your shapes.
Then identify which ones I can help you with and which ones you need to manage yourself.
As the clinician, it is our job to set goals with each patient and part of that process is to identify strategies to get them below the flare up line. So why not hit the biggest blocks first? Sleep, doing a home exercise program, eating well, continuing to exercise and keeping fit, doing things that you love, and most of all controlling what you can control in life.
For many people, and for Mrs. P in particular, if you can knock out the bigger shapes and I help with the physical/therapy related shapes, together we work out how to stay under the line and return to normal function in a graded way. Hopefully this explains my theory a little (again this is hard to write down) and I want to emphasize this is merely my visual analogy for helping others realize how much control they have over their own problem. What I use it to explain is:
- How much they have to be actively involved in their own recovery,
- How they have to help set realistic and measurable goals,
- How pain is multifaceted,
- That addressing other areas of health and wellbeing is so important in recovery,
- And, that pain is manageable.
For Mrs. P this visualisation clicked on the first session and she went away with a home exercise program designed to initially help reduce her pain and then redevelop strength. Our treatments till involved more traditional manual therapy, soft tissue treatments and a progressive home exercise program but Mrs. P spent time focussing on her sleep, diet and recognizing and reducing other stresses in her life. She was curious about her pain and creative about her movements. No longer held back by the fear of not knowing what to do about her pain, she actively did something everyday to help herself recover. These two tips, understanding the complex contributions to pain and recognizing how movement is helpful to recovery simply set her on the path to drive her own recovery. She even created the exercise below as a progression of her forearm strengthening exercises to improve reaching forward and overhead (two of her aggs) and she called them tick-tocks.
Summary
This patient received 8 sessions in total over the course of 6 weeks and was pain free for the two weeks leading up to her final review. For me this was one of the quickest recoveries I had seen, to go from continuous pain to return of full function in around four weeks. Especially as my expectations for LE is that it can be a tricky condition to get settled. We were both very happy with the outcome but the biggest thing I learnt is not to underestimate the power of knowledge and it's influence on healing and recovery. I am continually reminded that the human body is a complex and beautiful organism, that it is both unique and indivisible. We can't remove the mind from the physical body and we should not approach recovery by viewing the elbow as a removable part of the entire picture.
"What goes on in our body effects what goes on in our minds and what goes on in our minds effects what goes on in our bodies" (Robert Sapolsky).
The words we choose can convey a powerful message to our patients. Use them to empower those around you.
SS :)