Cricket Case Study
Working in cricket the past 2 years, I have seen many athletes who experience pain after bowling. Tim is a very typical case, with multiple areas to address. Meet Tim...
Presenting Problem
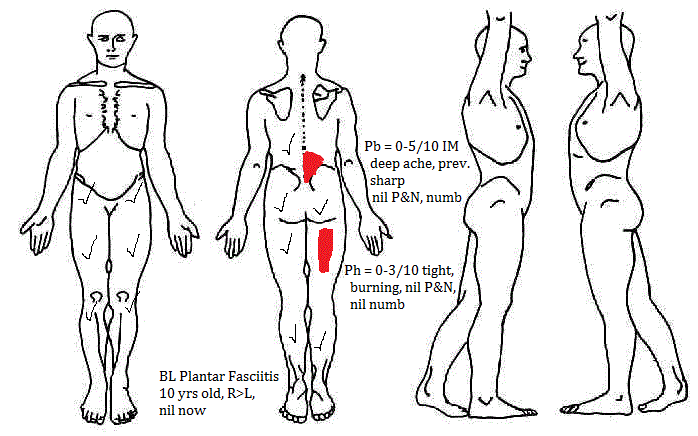
30 year old male, amateur spin bowler
Aggravating Factors
- Sitting 2 hours onset of Pb3/10, walking/stretching into Lx extension for 3 mins eases pain to zero
- Driving 60 mins Pb3/10, Ph1/10, eases with lumbar extension stretching for 3 mins
- Deadlifts 50kg max, Pb5/10 >55kg, nil Ph, awareness for 2 days
- Bowling - 1 hour post-bowling brings on Pb4/10, Ph 1/10 awareness, eases with 24 hours of rest/”cobra” (lumbar extension) stretching
Tim avoids impact or weighted bending (lifting weights, lifting boxes) to prevent flare-ups
24 Hour Behaviour
AM – stiff Pb2/10, 30 mins to ease PM – when Pb >3/10, wakes in night when changing position
History
Current History:
- Pb increased one month ago, previously Pb 2/10 max, now 5/10 max, coincided with increase in cricket load
- Tues/Thurs 15-20 overs (90-120 balls), Sat 10-20 overs (60-120 balls), total ~50 overs/week (300 balls/week)
- 7 weeks ago – 3 hour flight, Pb3/10 by end of flight, next day Pb6/10 on bending/sitting, eased after 5 days with rest & avoiding aggs
Past History:
- 4 yrs ago post-cricket onset of Pb, sharp 8/10, had started working in pub at same time, lifting 65kg kegs of beer 5-10x a day, saw physio, diagnosed “bulging disc”, resolved with lumbar extension, stretching & off-season of cricket so not aggravating back
Social History:
- Works in sales, sit/stand/walking during day, minimal gym/strength work, often driving between clients,
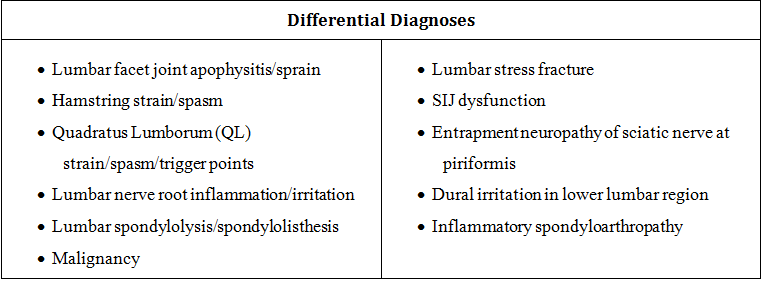
Differential Diagnoses
Following subjective questioning, I already have a list of possible diagnoses in my head. Based on the patient's aggravating and easing factors, location of pain, age, occupation and previous injury history, this was the prioritised list of diagnoses I had to confirm or refute, during my physical examination.
My goals for the initial physical examination were:
- Determine source of Pb, confirm primary hypothesis of discal pathology with neural irritation, isolate lumbar pain to specific level/s.
- Determine contribution of neurodynamic dysfunction to Ph.
- Determine contribution of secondary hypotheses to primary presentation (e.g. QL muscle spasm, facet joint stiffness) or clear secondary hypotheses.
- Determine contribution of bowling technique and biomechanical factors (gluteal, calf strength, lumbosacral control) to pain.
If I achieved all of these goals in my day 1 assessment, I would have a solid understanding of the patient's presentation and a clear plan for the following few sessions.
Physical Examination
Symptom Sources/Mechanisms
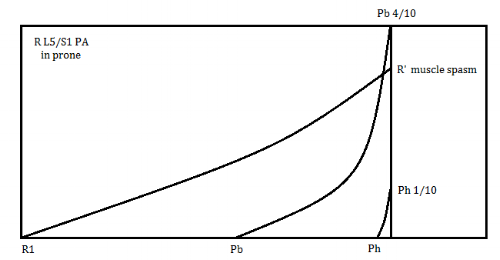
- PA R L5/S1 hypo Pb4/10, Ph1/10
- Central PA L5 hypo + Pb3/10, nil Ph
- R SLR 80° Ph1/10, with ankle DF Ph2/10, slight Pb awareness
- Muscle spasm R QL (reproduce Pb1/10), gluteus medius
Physical Impairments
- Lx flexion = fingers to ankles, Pb1/10 EROM (end-range)
- Flexion/L sideflexion/rotation (opening Quadrant) = symmetrical range, Pb3/10, Ph awareness
- Lx/hip Quadrant clear
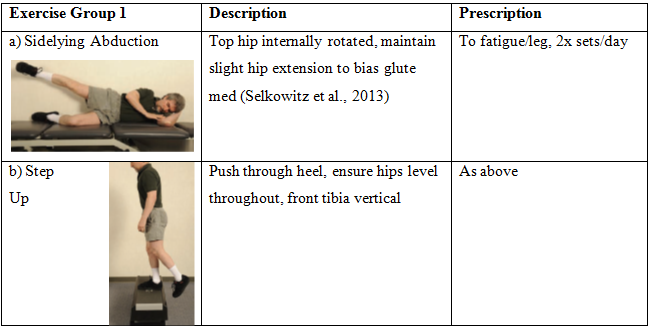
- Glut med endurance (sidelying hip abduction) L 12 repetitions fatigue, RPE 6/10, R 15 reps, RPE 3/10
- Glut max strength L 160mmHg, RPE 8/10, 190mmHg, RPE 7/10
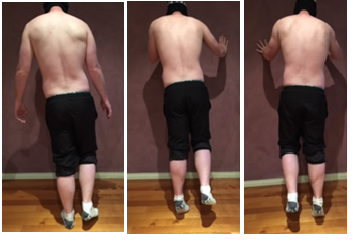
- SLCR L = supinates midfoot, left trunk lean, ¾ plantarflexion range, when corrected L fatigues 5 reps, R 8 reps
Pic 1&2: Left leg single leg calf raise Picture 3: R SLCR
- SLSquat BL = Moderate dynamic knee valgus, Trendelenberg with anterior pelvic tilt, trunk lean forward (Crossley et al., 2011)
Pic 1 & 2: Left single leg squat Pic 3: Right single leg squat
- Reduced muscle tone/bulk bilateral lower glute max, medial gastrocnemius
- Hop – bilateral excessive arm/trunk/hip strategy to initiate movement, dynamic knee valgus & Trendelenberg on land, reduced hop height
Sporting / Functional Limitations
- No cricket limitation
- Deadlifts 50kg max, Pb5/10 >55kg
- Sitting >2hours, Pb3/10
Contributing / Predisposing Factors
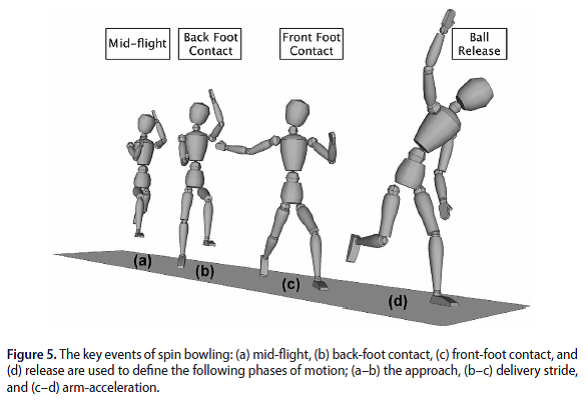
Bowling Technique
- Back foot planted ~50° to wicket (75 - 90° recommended to reduce injury risk (Beach et al., 2016))
- 50° lumbar sideflexion on ball release (recommended 20 - 40° (Elliott & Khangure, 2002))
- Minimal rear thigh drive (Ferdinands, Kersting, & Marshall, 2009)
Bowling Load
- Currently 240 – 360 balls/week, Tuesday/Thursday/Saturday
- Bowling >188 balls/week correlated with increased injury risk (Dennis, Farhart, Goumas, Orchard, & Farhart, 2003)
- <2 days rest between sessions gives 2.4x injury risk, with 1.4x with 2-3 days rest (Dennis et al., 2003)
- Bowling 200% of monthly average (chronic load) gives 3.3x greater risk of injury (Hulin et al., 2014)
- Patient bowling >188 balls/week, having <2 days rest between sessions, and had large acute load spike, giving high injury risk
Psychosocial Impairments, Attitudes, Beliefs
Displays poor pacing, avoidance behaviour with ADL’s, maladaptive coping (Fersum, O'Sullivan, Skouen, Smith, & Kvale, 2013)
Treatment
1. R PA L5/S1 III 3x30sec
- Reproduced both Pb and Ph symptoms, no worsening of symptoms following PAIVM’s assessment
- Provocative segment consistent with body chart, AROM restrictions and functional deficits
- Movement diagram shows muscle spasm, pain is limiting factor not resistance, consistent with chemically sensitised disc and somatic referral to hamstring
- Technique addressing pain, rather than resistance, so mobilisation applied at mid-range (G3 not ++)
- Larger amplitude technique chosen to reduce risk of latency to sensitised structures
- Dosage conservative, care taken with sensitised disc/neural structures
// Lx flex = full, no pain // Opening Quadrant = full, no pain // QL – nil spasm, nil Pb // R SLR 90° stretch, nil Ph, with ankle DF Ph1/10, nil Pb
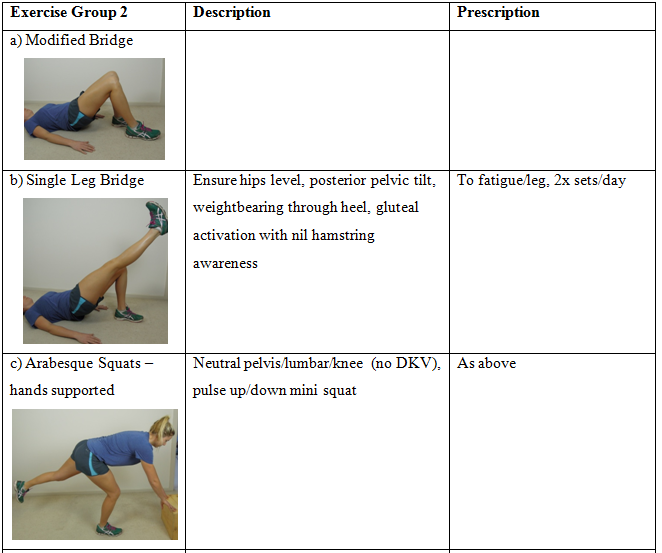
2. Modified Bridge
- Push through heel closest to hips, ensure hips level (addressing rotational deficit in single leg squat), encourage posterior pelvic tilt (biasing inferior glut max), neutral thoracolumbar junction
- Fatigued 15 reps L, 19 reps R, complete 3x sets to fatigue daily, targeting activation and endurance with high repetitions and repeated daily (no rest days between)
- Co-contraction of gluteus medius, biasing glute max but addressing activation/endurance deficits in both glute max and med (Selkowitz, Beneck, & Powers, 2013)
// Opening Quadrant = full, no pain // R SLR 90° stretch, nil Ph, with ankle DF nil Ph/Pb // Prone hip extension L RPE 5/10 (previously 8/10), R 4/10 (previously 7/10) // Sidelying hip abduction L RPE 3/10 (previously 6/10), R 2/10 (previously 3/10) // L SLSquat = mildly improved dynamic knee valgus, reduced trunk lean to left
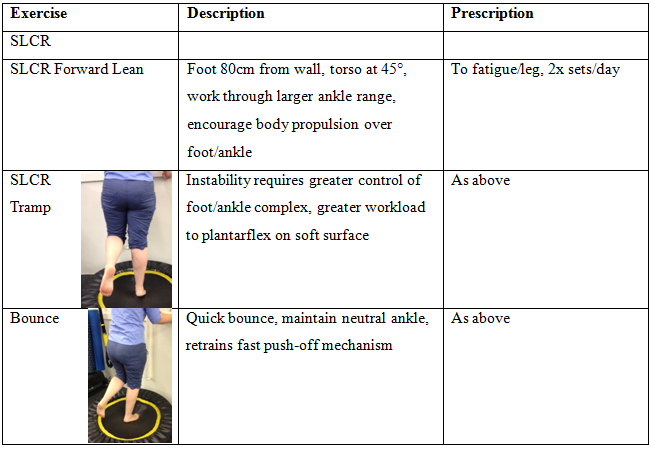
3. Single Leg Calf Raise
- Weight on big toe to encourage neutral midfoot and medial gastrocnemius/evertor co-contraction
- Perform in front of mirror to increase external feedback on technique
- Fatigued 5 reps L, 8 reps R, 3 sets to fatigue completed in treatment, home exercise – complete 6x sets to fatigue daily, targeting activation and endurance with high repetitions and multiple sets (achieve neural adaptation) (Joyce, 2014)
- Improved foot biomechanics to allow improved “push-off” (Oatis, 2009; Silbernagel et al., 2001)
// Flexion/L sideflexion/rotation = full, no pain // SLCR L = 10 rep fatigue, R 13 rep fatigue // SLSq L R = improved trunk control, dynamic knee valgus ISQ // Hop L R = ~30% reduced arm/trunk/hip strategy, slightly increased hop height
Exercise Progressions
The exercises from Day 1 would be progressed over the next 6 weeks, as described in the tables below.
Single Leg Calf Raise Exercise Progressions - targeting medial gastrocnemius & soleus, progress once patient achieves 25 reps/leg, maintaining good technique.
Sidelying Abduction Exercise Progressions - targeting gluteus medius, progress once patient achieves 25 reps/leg, maintaining good technique.
Lunge - targeting gluteus maximus, progress once patient achieves 25 reps/leg, maintaining good technique.
Return To Sport Plan
The patient presents with three common bowling technical faults, planting his foot too front-on, poor pelvic drive and increased lumbar counter-rotation. Assessing and modifying technique errors, consistent with back pain (such as poor foot position and excessive counter-rotation), decreases incidence and progression of lumbar disc degeneration (Elliott & Khangure, 2002).
Poor bowling load management is a consistent factor in cricketer’s low back pain (Hulin et al., 2014; Orchard et al., 2015; Orchard, James, Portus, Kountouris, & Dennis, 2009). By effectively managing bowling load, while addressing strength, motor control and technique, Tim's pain should resolve.
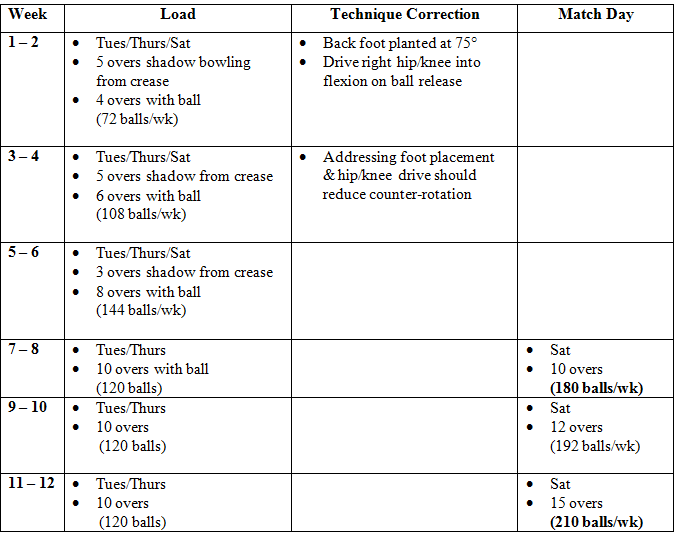
Bowling Plan
Planned return to bowling plan, return to full load by week 12. If pain occurs, regress by 1 week.
Prognosis
Favourable
Both Pb and Ph were resolved during the initial treatment session, indicating a mechanical loading dysfunction, rather than loss of structural integrity and tissue damage. There is gross lower limb kinetic chain weakness and poor control, with great potential for improvement. Addressing the causes of dysfunction, by providing greater lower limb strength/endurance and lumbopelvic control, should protect sensitised structures and prevent recurrence. Currently, there is poor bowling load management; monitoring and managing this more closely can greatly reduce risk of recurrence. (Dennis, Farhart, Clements, & Ledwidge, 2004; Hulin et al., 2014; Orchard et al., 2009)
Unfavourable
Most acute lumbar incidents resolve within a month, however recurrence rates within 12 months are up to 78% (Van Dillen et al., 2016), with poor recovery. This is attributed to cognitive factors (Vlaeyen & Linton, 2012), physical factors (Peter O'Sullivan et al., 2006) and lifestyle conditions (Fersum et al., 2013). There is also poor diagnosis, with 90% of low back pain considered non-specific, due to absence of strong radiological findings (P. O'Sullivan, 2005). The patient shows signs of maladaptive coping strategies and poor pacing, global deconditioning, altered body schema, muscle guarding and altered movement patterns, increasing the likelihood of recurrence.
Summary
Tim has now returned to full bowling load, and is currently bowling pain-free at amateur level cricket, bowling ~250 balls/week. The combination of manual therapy, strength/rehabilitation and monitoring and controlling bowling load successfully achieved full return to pain-free sport. I believe previous treatment had only addressed one or two aspects, without addressing all pathology and contributing factors. Hopefully, this case study can be applied to any musculoskeletal condition, so the next time you treat a cyclist, carpenter, office worker or lecturer, you address their physical impairments, contributing factors and ensure a graded return to loading plan.
Alicia
References:
Beach, A. J., Ferdinands, R. D., & Sinclair, P. J. (2016). The kinematic differences between off-spin and leg-spin bowling in cricket. Sports Biomechanics, 15(3), 295-313.
Bogduk, N. (2009). On the definitions and physiology of back pain, referred pain, and radicular pain. Pain, 147(1-3), 17-19.
Brukner, P., & Khan, K. (2012). Brukner & Khan's clinical sports medicine (4th ed.). Sydney ; New York: McGraw-Hill.
Burnett, A. F., Elliott, B. C., & Marshall, R. N. (1995). The effect of a 12-over spell on fast bowling technique in cricket. Journal of sports sciences, 13(4), 329-341.
Coppieters, M., Stappaerts, K., Janssens, K., & Jull, G. (2002). Reliability of detecting 'onset of pain' and 'submaximal pain' during neural provocation testing of the upper quadrant. Physiotherapy research international : the journal for researchers and clinicians in physical therapy, 7(3), 146-156.
Crossley, K. M., Zhang, W.-J., Schache, A. G., Bryant, A., & Cowan, S. M. (2011). Performance on the single-leg squat task indicates hip abductor muscle function. The American journal of sports medicine, 39(4), 866-873.
Dennis, R., Farhart, P., Clements, M., & Ledwidge, H. (2004). The relationship between fast bowling workload and injury in first-class cricketers: a pilot study. Journal of science and medicine in sport / Sports Medicine Australia, 7(2), 232-236.
Dennis, R., Farhart, P., Goumas, C., Orchard, J., & Farhart, R. (2003). Bowling workload and the risk of injury in elite cricket fast bowlers. Journal of science and medicine in sport / Sports Medicine Australia, 6(3), 359-367.
Donelson, R., Aprill, C., Medcalf, R., & Grant, W. (1997). A prospective study of centralization of lumbar and referred pain - A predictor of symptomatic discs and anular competence. Spine, 22(10), 1115-1122.
Elliott, B., & Khangure, M. (2002). Disk degeneration and fast bowling in cricket: an intervention study. Medicine and science in sports and exercise, 34(11), 1714-1718.
Ferdinands, R. E. D., Kersting, U., & Marshall, R. N. (2009). Three-dimensional lumbar segment kinetics of fast bowling in cricket. Journal of biomechanics, 42(11), 1616-1621.
Fersum, K. V., O'Sullivan, P., Skouen, J. S., Smith, A., & Kvale, A. (2013). Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: A randomized controlled trial. European Journal of Pain, 17(6), 916-928.
Horn, K. K., Jennings, S., Richardson, G., van Vliet, D., Hefford, C., & Abbott, J. H. (2012). The Patient-Specific Functional Scale: Psychometrics, Clinimetrics, and Application as a Clinical Outcome Measure. Journal of Orthopaedic & Sports Physical Therapy, 42(1), 30-42.
Hulin, B. T., Gabbett, T. J., Blanch, P., Chapman, P., Bailey, D., & Orchard, J. W. (2014). Spikes in acute workload are associated with increased injury risk in elite cricket fast bowlers. British journal of sports medicine, 48(8), 708-712.
Hungerford, B., Gilleard, W., & Hodges, P. (2003). Evidence of altered lumbopelvic muscle recruitment in the presence of sacroiliac joint pain. Spine, 28(14), 1593-1600.
Jensen, M. C., Kelly, A. P., & Brantzawadzki, M. N. (1994). MRI OF DEGENERATIVE DISEASE OF THE LUMBAR SPINE. Magnetic Resonance Quarterly, 10(3), 173-190.
Joyce, D. (2014). High-performance training for sports.
Kahraman, B. O., Sengul, Y. S., Kahraman, T., & Kalemci, O. (2016). Developing a Reliable Core Stability Assessment Battery for Patients With Nonspecific Low Back Pain. Spine, 41(14), E844-E850.
Laplante, B. L., Ketchum, J. M., Saullo, T. R., & DePalma, M. J. (2012). Multivariable Analysis of the Relationship Between Pain Referral Patterns and the Source of Chronic Low Back Pain. Pain Physician, 15(2), 171-178.
Laslett, M. (2006). Pain provocation tests for diagnosis of sacroiliac joint pain. The Australian journal of physiotherapy, 52(3), 229.
Maitland, G. D., & Edwards, B. C. (1986). Vertebral manipulation (5th ed.). London ; Boston: Butterworths.
Middleton, K., Foster, D., & Alderson, J. (2016). Pelvic and trunk mechanics and injury in cricket: A spin bowling case study. International Journal of Sports Science & Coaching, 11(2), 250-254.
Moore, K. L., Dalley, A. F., & Agur, A. M. R. (2014). Clinically oriented anatomy (7th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health.
O'Sullivan, P. (2005). Diagnosis and classification of chronic low back pain disorders: Maladaptive movement and motor control impairments as underlying mechanism. Manual therapy, 10(4), 242-255.
O'Sullivan, P., Dankaerts, W., Burnett, A., Chen, D., Booth, R., Carlsen, C., & Schultz, A. (2006). Evaluation of the flexion relaxation phenomenon of the trunk muscles in sitting. Spine, 31(17), 2009-2016.
Oatis, C. A. (2009). Kinesiology : the mechanics and pathomechanics of human movement. Baltimore: Lippincott Williams & Wilkins,.
Orchard, J. W., Blanch, P., Paoloni, J., Kountouris, A., Sims, K., Orchard, J. J., & Brukner, P. (2015). Cricket fast bowling workload patterns as risk factors for tendon, muscle, bone and joint injuries. British journal of sports medicine, 49(16), 1064-1068.
Orchard, J. W., James, T., Portus, M., Kountouris, A., & Dennis, R. (2009). Fast bowlers in cricket demonstrate up to 3- to 4-week delay between high workloads and increased risk of injury. The American journal of sports medicine, 37(6), 1186-1192.
Orchard, J. W., James, T., & Portus, M. R. (2006). Injuries to elite male cricketers in Australia over a 10-year period. Journal of science and medicine in sport / Sports Medicine Australia, 9(6), 459-467.
Perry, J., Weiss, W. B., Burnfield, J. M., & Gronley, J. K. (2004). The supine hip extensor manual muscle test: a reliability and validity study. Archives of physical medicine and rehabilitation, 85(8), 1345-1350.
Ranawat, V. S., Dowell, J. K., & Heywood-Waddington, M. B. (2003). Stress fractures of the lumbar pars interarticularis in athletes: a review based on long-term results of 18 professional cricketers. Injury, 34(12), 915-919.
Selkowitz, D. M., Beneck, G. J., & Powers, C. M. (2013). Which exercises target the gluteal muscles while minimizing activation of the tensor fascia lata? Electromyographic assessment using fine-wire electrodes. The Journal of orthopaedic and sports physical therapy, 43(2), 54-64.
Silbernagel, K. G., Thomee, R., Thomee, P., & Karlsson, J. (2001). Eccentric overload training for patients with chronic Achilles tendon pain--a randomised controlled study with reliability testing of the evaluation methods. Scandinavian journal of medicine & science in sports, 11(4), 197-206.
Stuge, B., Hilde, G., & Vollestad, N. (2003). Physical therapy for pregnancy-related low back and pelvic pain: a systematic review. Acta obstetricia et gynecologica Scandinavica, 82(11), 983-990.
Van Dillen, L. R., Norton, B. J., Sahrmann, S. A., Evanoff, B. A., Harris-Hayes, M., Holtzman, G. W., . . . Strube, M. J. (2016). Efficacy of classification-specific treatment and adherence on outcomes in people with chronic low back pain. A one-year follow-up, prospective, randomized, controlled clinical trial. Manual therapy, 24, 52-64.
Vlaeyen, J. W. S., & Linton, S. J. (2012). Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain, 153(6), 1144-1147.
Vleeming, A., Schuenke, M. D., Masi, A. T., Carreiro, J. E., Danneels, L., & Willard, F. H. (2012). The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. Journal of anatomy, 221(6), 537-567.
Widler, K. S., Glatthorn, J. F., Bizzini, M., Impellizzeri, F. M., Munzinger, U., Leunig, M., & Maffiuletti, N. A. (2009). Assessment of hip abductor muscle strength. A validity and reliability study. The Journal of bone and joint surgery. American volume, 91(11), 2666-2672.
Xergia, S. A., Pappas, E., Zampeli, F., Georgiou, S., & Georgoulis, A. D. (2013). Asymmetries in Functional Hop Tests, Lower Extremity Kinematics, and Isokinetic Strength Persist 6 to 9 Months Following Anterior Cruciate Ligament Reconstruction. Journal of Orthopaedic & Sports Physical Therapy, 43(3), 154-162.