Cervical Motor Control Part 3 - Does Posture Matter?
Welcome to part three of the cervical motor control series as we breakdown the topic of posture. If you missed the previous two, there has been a blog on clinical anatomy of the cervical spine and an outline of cervical motor control assessment. The topic of 'ideal posture' continues to be challenging to define.
“Any information gained from the assessment of sitting and standing posture has to be linked to the problem” (Jull, 2008, p. 159). We can’t simply assume that posture is correlated to pain until we prove that changing it changes the pain.
The first reason for this challenge in the discussion of posture is that every functional task, occupation or daily position can be performed in a range of postures and there really is no way of saying one posture is perfect compared to others. A second reason revolves around the definition of ideal posture. When using the word posture in treatment or in research it is often difficult to know if we are referring to lumbo-pelvic sitting posture, scapula posture, head on neck posture, or all three. In fact, in regards to neck pain, posture actually involves all three of these aspects.
We are living in a technology driven world and many would say that office-related work tasks are the cause of the increasing prevalence of neck pain. Personally, I think this is a big leap and possibly placing a bit too much blame on the computer. Yes, we can't deny that there is more use of computers and smart phones but there is also increased usage of standing desks, raised screens, larger screens, wireless keyboards and mouses, better chairs, better prescription of glasses and less writing time. So, before we look at the final blog on phases of rehabilitation I first want to address the point of posture and the literature I read surrounding it the context of neck pain. I'll begin by saying that the evidence remains inclusive about the strong link between posture and pain. Nonetheless it doesn't deter me from discussing the topic as it is a common questions asked of me by my patients.
The goal for this blog is to take a brief moment to look at desk set up and the variability that can exist in sitting postures despite amazing workplace modifications. What I hope you'll notice is that it is not always the computers fault, but how long we use it for and how we use it. A previous blog by Alicia discussed the power of the words we use to discuss back pain, and the main message from that blog "what does that word mean to you?" is a principle that can be applied to all aspects of patient education. In this case it relates to "when I discuss the role of posture - what do you interpret that to mean?".
FORWARD HEAD POSTURE
One of the aspects of sitting that often comes under scrutiny is head position in relation to computer usage. In 2002, Szeto, Straker and Raine investigated the role of a forward head posture in neck pain. Forward head posture (FHP) is a combination of lower cervical flexion, upper cervical extension and rounded shoulders. What they found is that office works do have a tendency to hold their necks in increased lower cervical flexion while looking at a screen.
While it seems logical that this position would place increased loads on cervical structures, proving a cause-effect relationship between posture and pain is incredibly difficult (Szeto, Straker & Raine., 2002, p. 75). I believe this is because many people can have ‘poor posture’ and never develop pain and others can sit ‘ideally’ and still experience problems.
When it comes to postures the take home message is always if you can change the posture and it changes the pain, then postural re-education is worthwhile involving in treatment. If you assess your patients naturally sitting tendencies and there is a degree of forward head posture, be sure to check if changing this leads to a change in symptoms before placing the blame here.
Scapula positioning
Positioning and functioning of the scapula are concepts that are spoken about throughout the literature in relation to neck pain. With neck pain specifically, "comparing the patient’s painful neck symptoms, painful cervical movements, and palpable tenderness in axioscapular muscles, immediately before and after repositioning of the scapula, are helpful assessment strategies” (O’Leary, Falla, Elliott & Jull., 2009, p. 328).
It is important to assess the scapula in the most functional position for each patient. This may be either a prolonged static position or dynamic movement. If you are not sure how to bring out these motor control deficits, you may wish to consider loading the functional aggravating position. “Any alterations in scapula orientation and any lack of active scapular stability may become more obvious when the scapulae are loaded. This can be achieved by either the patient performing small arm movements (<30-40 degrees of motions) in ranges at which orientation of the scapula should remain relatively stable, or by having the patient perform isometric contractions of the shoulder against mild resistance” (Jull., 2008, p. 160-161). What we are trying to understand from our assessment is the possible connection between scapula position, cervical load and neck pain.
Scapula assessment is not covered in depth in this blog as the main focus around the neck itself. What you will see in the next blog is how scapula position varies between an office worker, painter and rugby player and how treatment is directed specifically at each patient type. Therefore it is beyond the scope of this blog to discuss all the variable scapula positions that may present with neck pain. If you are looking for more information about scapula dyskinesis, a previous blog discusses exercises that promote different aspects of scapula control.
Coming back to the neck however, please remember to assess the resting position of the scapula and how patients set and move their scapula during their functional movements. Below are two different scapula positions that can be adopted in the same chair and same laptop position and each of them need different corrections.
Does sitting posture influence neck muscle activity?
In 2010, Caneiro & colleagues studied three different postures in an asymptomatic population. The reason they investigated this idea is that prolonged non-neutral sitting positions have the potential for causing higher levels of cervical spine loading. “Evidence to link the influence of thoraco-lumbar spine posture to cervical posture and cervico-thoracic muscle activity is limited” (Caneiro et al., 2010, p. 52). Therefore, this was the first study to investigate the influence of these three different postures on head/neck posture and cervico-thoracic muscle activity.
Posture 1: slump sitting was a combination of sitting with thoraco-lumbar spine flexion and posterior pelvic rotation while still looking straight ahead.
Posture 2: lumbo-pelvic upright sitting consisted on anterior pelvic rotation which allowed the lumbar and thoracic spine to rest in a relaxed upright position with neural lumbar lordosis.
Posture 3: thoracic upright sitting consisted of anterior pelvic rotation, thoracic extension and shoulder blade retraction.
In each of these positions they investigate the surface EMG activity of the cervical erector spinae, thoracic erector spinae and upper trapezius. The results could be summarised as:
- Slump sitting had the highest amount of thoracic flexion and lumbar flexion of the three positions.
- Thoracic upright sitting had the lowest level of head/neck flexion and anterior head translation of the three postures.
- Slump sitting had the most head/neck flexion and anterior head translation of the three postures.
- When compare to lumbo-pelvic upright sitting, slump sitting has higher levels of thoracic flexion, more head/neck flexion and anterior head translation, increased activity of the cervical and thoracic erector spinae, and this is speculated to cause higher compressive loads on the cervical spine (Caneiro et al., 2010, p. 58).
- When compared to lumbo-pelvic upright sitting, thoracic upright sitting has more thoracic extension, reduced head/neck flexion and anterior head translation, higher amounts on thoracic erector spinae activity and less cervical erector spinae activity. These postural features can create cervical spinal loading through the multi-segmental attachment of the thoracic erector spinae coupled with reduced cervical erector spinae activity (Caneiro et al., 2010, p. 58).
In summary, lumbo-pelvic upright sitting is associated with the most neutral head/neck posture, the lowest amounts of superficial muscle activity across the cervicothoracic junction and is also associated with the highest levels of DNF activity. This makes lumbo-pelvic upright sitting the most ideal posture (Caneiro et al., 2010, p. 59). The outcomes of this study create a strong platform to continue research in understanding the correlation between these spinal postures and the existence of neck pain. Once a link between posture and pain is strongly established it would provide evidence for postural re-education in neck pain. Until then, clinically we can continue to evaluate the impact that changing head/neck posture and thoracic posture has on pain.
When I read this study was felt inspired to be more consistent in checking functional sitting posture in my patients with neck pain and educating them about how cervical loads change in each position. Then one morning I saw my husband working at the dining table (it is a pretty table but not awfully ergonomic) and I realised how slumped he was sitting. I briefly said "can you sit up a little straighter?" and when he did he moved so much further away from the laptop screen that his neck angle became more pronounced. Bugger I thought.... this research is going to be impacted by the environment more strongly than I anticipated.
What I decided to do next is take these three positions, which we assessed in static sitting, and put them in the context of computer work at a bench where there is no back rest (replicating the unsupported chair from the study). Interestingly, while the notes above say that the second picture is the most ideal posture, I'm not sure I would recommend any of these positions for patient working on a laptop. The first and third pictures don't look great but in the second, there is still too much looking down because of the bench height. So it begs the question of how much advice can we generically give about postural correction without taking into account the environment in which the person will be sitting?
Personally, I think these pictures are a great representation of when we can't just take on board all evidence because it was published in a research trial. It is a good reminder to ensure you use EBP in conjunction with your functional assessment and within the environmental context of the patient in front of you.
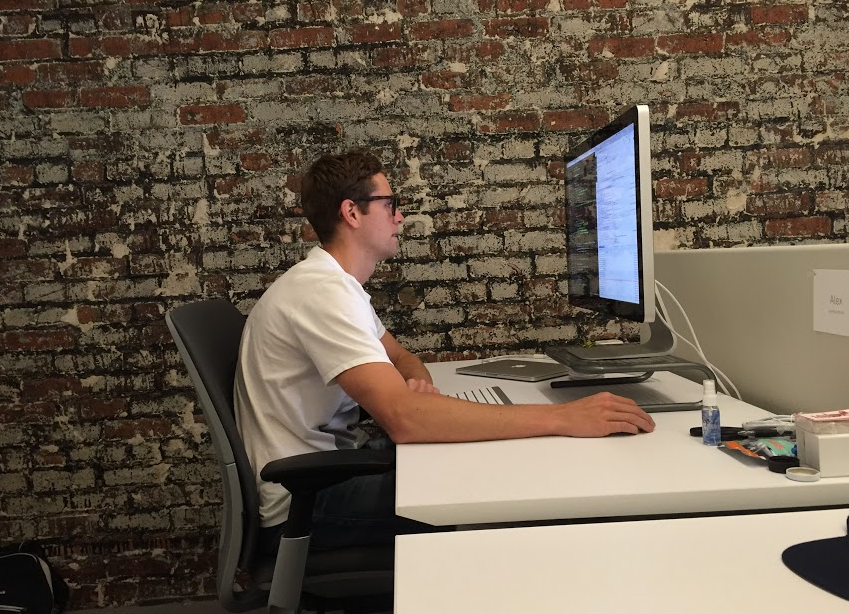
So what can we use to improve our patient's sitting posture? Fortunately we have new modifications available to us now, which include larger screens, desk chairs that are adjustable and standing desks. In the picture below my hubbie is showing me his 'comfy sitting position' for work. The screen is raised to raise his eye line, the wireless keyboard keeps his arms comfortably by his side and the adjustable arm rests allow the chair to roll in under the desk and allows him to rest back into the chair. This may not be the picture perfect sitting posture everyone strives for, but for him it is really comfortable and he works for long hours without any concerns. Reinforcing the idea that perfect posture isn't perfect for everyone. Or maybe there is no perfect posture to begin with?
Now, it is also important to recognise that you can have all the suggested workplace set up changes and still sit poorly. Here are a few different options that people commonly slip into. They may not be uncomfortable or bad for everyone and changing position during the day is really healthy, but, just remember that when you educate your patient on workplace setup, your advice might not translate into what you had in mind.
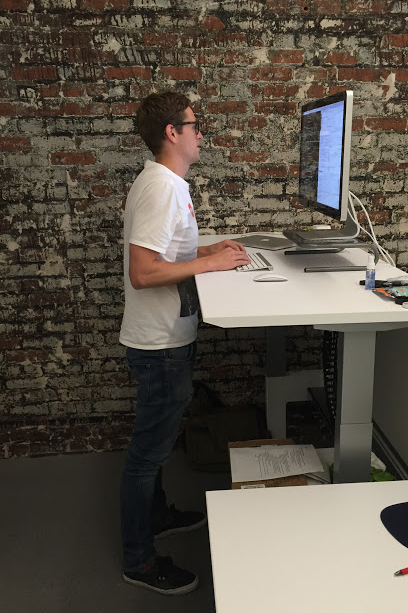
And finally, I think we should look at a few positions for the stand up desk.
I recognise that not everyone has access to this equipment but I hope that the pictures shown in this blog demonstrate the large variety of postures that can be used in different scenarios and emphasise that we need to educate patients about how to modify their posture for different environments. If you're not sure where to begin, first identify what posture your patient's sit in most often, change that posture, evaluate the effect on neck pain, and go from there.
Next week we look at the stages of rehabilitation in the context of three different patient subtypes, the office worker, the painter and the athlete. It begins with DCNF exercises, a place many of us know, and progresses through endurance, strength and functionally-targeted rehabilitation.
Sian :)
References:
Beer, A., Treleaven, J., & Jull, G. (2012). Can a functional postural exercise improve performance in the cranio-cervical flexion test? –A preliminary study. Manual therapy, 17(3), 219-224.
Caneiro, J. P., O'Sullivan, P., Burnett, A., Barach, A., O'Neil, D., Tveit, O., & Olafsdottir, K. (2010). The influence of different sitting postures on head/neck posture and muscle activity. Manual therapy, 15(1), 54-60.
Cleland, J. (2005). Orthopaedic clinical examination: an evidence-based approach for physical therapists. WB Saunders Co.
Edmondston, S., Björnsdóttir, G., Pálsson, T., Solgård, H., Ussing, K., & Allison, G. (2011). Endurance and fatigue characteristics of the neck flexor and extensor muscles during isometric tests in patients with postural neck pain. Manual Therapy, 16(4), 332-338.
Falla, D. (2004). Unravelling the complexity of muscle impairment in chronic neck pain. Manual therapy, 9(3), 125-133.
Falla, D., Bilenkij, G., & Jull, G. (2004). Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine, 29(13), 1436-1440.
Falla, D., Jull, G., O’leary, S., & Dall’Alba, P. (2006). Further evaluation of an EMG technique for assessment of the deep cervical flexor muscles. Journal of Electromyography and Kinesiology, 16(6), 621-628.
Jull, G. (2008). Whiplash, headache, and neck pain: research-based directions for physical therapies. Elsevier Health Sciences.
Jull, G. A., O'Leary, S. P., & Falla, D. L. (2008). Clinical assessment of the deep cervical flexor muscles: the craniocervical flexion test. Journal of manipulative and physiological therapeutics, 31(7), 525-533.
O'Leary, S., Falla, D., Elliott, J. M., & Jull, G. (2009). Muscle dysfunction in cervical spine pain: implications for assessment and management. journal of orthopaedic & sports physical therapy, 39(5), 324-333.
O’Leary, S., Falla, D., & Jull, G. (2011). The relationship between superficial muscle activity during the cranio-cervical flexion test and clinical features in patients with chronic neck pain. Manual therapy, 16(5), 452-455.
Schomacher, J., & Falla, D. (2013). Function and structure of the deep cervical extensor muscles in patients with neck pain. Manual therapy, 18(5), 360-366.
SELVARATNAM, Peter, et al. Headache, orofacial pain and bruxism. 2009.
Struyf, F., Nijs, J., Mottram, S., Roussel, N. A., Cools, A. M., & Meeusen, R. (2014). Clinical assessment of the scapula: a review of the literature. British journal of sports medicine, 48(11), 883-890.
Szeto, G. P., Straker, L., & Raine, S. (2002). A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Applied ergonomics, 33(1), 75-84.
VAN ETTEKOVEN, H.; LUCAS, C. Efficacy of physiotherapy including a craniocervical training programme for tension‐type headache; a randomized clinical trial. Cephalalgia, 2006, vol. 26, no 8, p. 983-991.
Watson, L. A., Pizzari, T., & Balster, S. (2010). Thoracic outlet syndrome part 2: conservative management of thoracic outlet. Manual therapy, 15(4), 305-314.