Pancoast Tumour & Red Flags for the Upper Limb
"Medicine is not and cannot be an exact science because of the complexity of the human element involved" (Henry Pancoast, 1932, p. 1391).
The topic of red flags intrigues me. Some practitioners would say that the diagnostic utility of red flags is not very strong, and they are not entirely wrong in making this claim based on our currently available evidence. Nonetheless, we need something to use to help guide our clinical decision making. From my experience using special questions to try identify red flags has been very useful, especially when I know what I am looking for. When you ask your special questions you really need to have an idea of what competing conditions have made their way onto your hypothesis list. Taking this approach is more effective than simply asking out of habit. Previously I have written broadly on the topic of red flags and this blog is going to zoom in onto one condition in particular, the Pancoast Tumour.
In a recent podcast by Untold Physio Stories, Jason Shane and Erson Religioso discuss a case where Erson identified several red flags and his patient ultimately was diagnosed with cancer. When I listened to the podcast it reminded me of a few unusual cases that I’ve experienced. You never forget them because the true fact is that when you gut starts to churn and you truly realise something isn’t quite right, then what remains to be determined is not always friendly. Nor is it easy to treat.
A case of a suspected Pancoast Tumour
The case I want to share is of a time when I was highly suspicious my patient had a pancoast tumour. Female, 59 years old, heavy smoker, stressful job, struggling with an lengthy work-cover (litigation) claim for her shoulder injury, poor general health, and I was treating her post a supraspinatus surgical repair and shoulder decompression. Her rehab was fairly consistent with the expected recovery until one day, when she came in with this sudden swelling over her left supraclavicular region. The swelling was accompanied with severe, non-remitting, non-mechanical pain shoulder pain and pain radiating in her arm all the way into the wrist and hand. There were no reflex or myotomal changes but her pain looked very much as though a nerve root was being entrapped (C6 nerve root dermatomal pattern). The swelling was so unusual and given her smoking history, her age and the nature of her presentation I immediately thought…"Oh dear, have I been treating her for a musculoskeletal shoulder injury and what if I've overlooked a Pancoast tumour?" This got me so worried…. Pancoast tumours are a fairly rare and very aggressive lung tumour that are associated with a poor prognosis and high mortality rates.
What is a Pancoast tumour?
The first case of this condition was reported in 1838 by Hare (Panagopoulos, et al., 2014). It wasn't until 90 years later that the tumour become a known entity. In 1924 Henry Pancoast, American Radiology, went to the American Medical Association and presented his first paper on a new case of intra-thoracic tumours (Pancoast, 1932). At this time the tumour was termed "superior pulmonary sulcus tumour" which implied the location of the tumour but not the origin. Around the same time, Tobias discovered that the tumour was brachio-pulmonary in origin (Arcasoy & Jett, 1997). Pancoast presented two papers in 1924 and 1932 and the tumour became known as Pancoast Tumour.
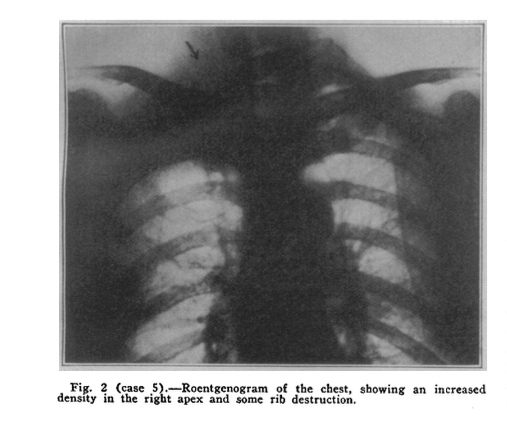
In his papers, Pancoast describes the clinical presentation of three cases. In each the tumour was associated with shoulder and arm pain, Horner's syndrome, and atrophy of the muscles of the hand. On radiographic imaging there was evidence of a shadow in the apex of the thoracic inlet, local destruction of the first three ribs and on occasion, infiltration of the vertebral bodies (Pancoast, 1932). In addition to these clinical features, patients were often found to have a small, hard and tender nodule at the base of their neck, distended veins in the neck, left upper chest, shoulder, and upper third of the arm (Pancoast, 1932).
Pancoast tumours come under the subset of non-small cell carcinoma of the lung (NSCLC). As mentioned previously, it is a tumour within the pulmonary sulcus and accounts for 5% of all cancers (Manenti, et al., 2013; Panagopoulis, et al., 2014).
Clinical presentation
The main clinical features originally noted by Pancoast are described above, and some authors referred to these as Pancoast-Tobias Syndrome (Panagopoulos, et al., 2014). Differential diagnosis involves cervical radiculopathy, rotator cuff disease and thoracic outlet syndrome. None of these conditions however would result in distended vein's on the neck, chest and arm, Horner's syndrome, and an opaque mass on chest XRAY.
Horner's Syndrome. Image courtesy of Google Images
One of the hallmark features of Pancoast tumours is the development of Horner's syndrome. Horner's syndrome occurs on the ipsilateral side to the symptoms and is caused by the invasion of the tumour into the cervical stellate ganglion resulting in:
- Miosis (constricted pupil),
- Ptosis (droopy eyelid),
- Enophthalmos (inset eyeball),
- Anhidrosis (decreased sweating) (Arcasoy & jett, 1997; Manenti, et al., 2013).
(Arcasoy & Jett, 1997, p. 1370)
Horner's syndrome doesn't occur in all presentations. When it does occur, shoulder pain is the primary symptom for months prior to it's development. This would explain why this conditions is often mistaken for musculoskeletal conditions of the shoulder or cervical spine.
Image courtesy of Google Images
To a large extent, the symptoms depend on the surrounding structures that the tumour encroaches on or invades. Interestingly, Panagopoulos, et al (2014, p. S111) discuss how the location of the tumour alters the clinical symptoms:
- If the tumour is between the sternum and anterior scalene then the pain is predicted to radiate into the anterior chest wall and also cause venous thrombosis.
- If the tumour is between the anterior and middle scalene it causes pain and paraesthesis in the shoulder, anterior upper limb, and arterial thrombosis and diaphragm paralysis.
- If the tumour is behind the middle scalene it results in pain in the axillary region, medial upper arm and Horner's syndrome.
None of the articles discuss the nature or behaviour of the pain around the shoulder. Luckily for us, 90 years later and we have developed a lot more knowledge about pain presentations of common musculoskeletal conditions and can use this knowledge in our assessment to determine in the pain is mechanical, neurogenic, centrally driven etc.
Medical imaging
In many cases, the first line of referral is for a plain chest Xray. On Xray a difference in apical caps of >5mm is considered to be clinically significant (Arcasoy & Jett, 1997, p. 1371).
(Pancoast, 1932, p. 1393)
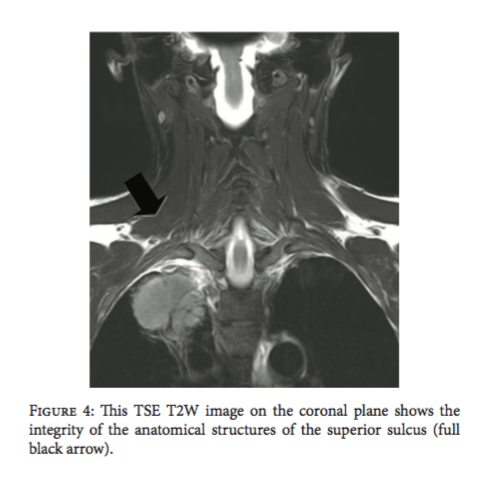
MRI and CT scans play an important role in diagnostic imaging. If radio-opacity is seen on XRAY then PET-CT can be used to confirm diagnosis, while MRI helps to provide a high resolution image of all the surrounding tissues (Manenti, et al., 2013).
"MR imaging has a pivotal role for staging and therapeutic management in patients with Pancoast tumour. MR neurography, Diffusion Weighted (DW) imaging, and MR angiography are actually mandatory imaging techniques in all patients with superior pulmonary sulcus tumours" (Manenti, et al., 2013, p. 5).
(Manenti, et al., 2013, p.3)
(Manenti, et al., 2013, p.3)
Treatment & prognosis
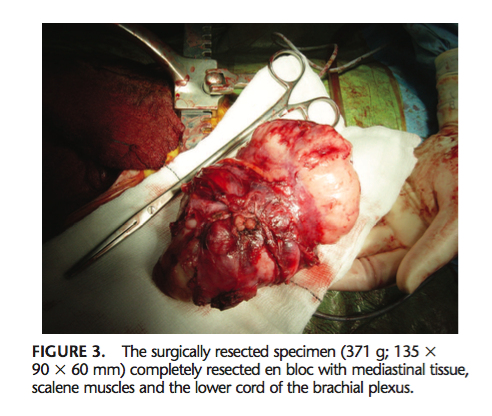
Many of the case studies I've read around this topic, including Dartnell et al (2009) describe the pancoast tumour as rare and highly aggressive. At the time that Pancoast published his papers (over 90 years ago) the tumour was treated primarily with radiation therapy, not surgical resection, and known to be rapidly fatal, with most patients dyeing within 3-4 months of diagnosis. Since then, treatment has changed.
(Dartnell, et al., 2009, p. 137)
The 1960's saw the first attempts of surgical resection combined with radiotherapy and this approach remained the mainstay for the next 30 years. It wasn't until the 1990's when combined chemotherapy, radiotherapy and surgical resection was introduced and suddenly mortality rates began to change (Panagopoulos, et al., 2014).
"Prognosis depends mainly on T stage of tumour, response to preoperative chemo-radiotherapy and completeness of resection" (Formulas, et al., 2013, p. S342).
- Surgery for Pancoast tumours is associated with 5% mortality rate and the complication rate varies from 7-38% (Formulas, et al., 2013, p. S342).
- The overall five-year survival rate after combined preoperative radiotherapy and extended surgical resection is generally around 20 to 35 percent, with a median survival of 7 to 31 months (Arcasoy & Jett, 1997, p. 1374).
- The overall 2-year survival rate after induction chemo-radiotherapy and resection varies from 55% to 70%, while the 5-year survival for resections is quite good (54-77%) (Formulas, et al., 2013, p. S342).
- The main pattern of recurrence is that of distant metastases, especially in the brain (Formulas, et al., 2013, p. S342).
What did my treatment and assessment involve?
Coming back to the case above... I assessed her neck, thoracic spine, and shoulder thoroughly and then wrote a letter to the doctor stating my physical findings, clinical presentations and concerns about the sudden changes in her clinical presentation. This patient didn't have signs of Horner's syndrome but as the research suggests, this doesn't occur until later in the disease progression.
After referral to the doctor, the patient was quickly referred for an XRAY and cervical MRI as the doctor shared the same concerns as I had. Luckily there was no tumour but the MRI revealed a large nerve entrapment. Given the severity of her pain, she was referred for a cortisone injection as a first line of treatment and thankfully her symptoms resolved quickly.
Closing thoughts
So all in all, it was nasty and painful but not sinister. It didn’t look like a usual C6 radiculopathy and there were several red flags in her presentation. I’m glad I made the decision to refer her out immediately and she landed up quickly on the best course of treatment.
What I have found clinically is that if you perform a thorough physiotherapy assessment, ask the relevant special questions and then refer your client to their doctor with a letter supporting your suspicions, they will be much better cared for than simply telling someone to go ask their doctor for a second opinion.
Pancoast tumours are a rare condition and rapidly progressing. Often there are delays in diagnosis when aspects of clinical presentation are similar to common complaints such as cervical radiculopathy. Make the pieces fit and when in doubt, refer out for a second opinion.
Sian :)
References:
Arcasoy, S. M., & Jett, J. R. (1997). Superior pulmonary sulcus tumors and Pancoast's syndrome. New England Journal of Medicine, 337(19), 1370-1376.
Dartnell, J., Pilling, J., Ferner, R., Cane, P., & Lang-Lazdunski, L. (2009). Malignant triton tumor of the brachial plexus invading the left thoracic inlet: a rare differential diagnosis of pancoast tumor. Journal of Thoracic Oncology,4(1), 135-137.
Foroulis, C. N., Zarogoulidis, P., Darwiche, K., Katsikogiannis, N., Machairiotis, N., Karapantzos, I., ... & Zarogoulidis, K. (2013). Superior sulcus (Pancoast) tumors: current evidence on diagnosis and radical treatment. Journal of thoracic disease, 5(Suppl 4), S342.
Manenti, G., Raguso, M., D'Onofrio, S., Altobelli, S., Scarano, A. L., Vasili, E., & Simonetti, G. (2013). Pancoast tumor: the role of magnetic resonance imaging. Case reports in radiology, 2013.
Pancoast, H. K. (1932). Superior Pulmonary Sulcus Tumor: Tumor characterized by pain, Horner's Syndrome, destruction of bone and atrophy of hand muscles Chairman's Address. Journal of the American Medical Association,99(17), 1391-1396.
Panagopoulos, N., Leivaditis, V., Koletsis, E., Prokakis, C., Alexopoulos, P., Baltayiannis, N., ... & Katsikogiannis, N. (2014). Pancoast tumors: characteristics and preoperative assessment. Journal of thoracic disease,6(1), S108-S115.
Weber, D. J., Okereke, I. C., Birdas, T. J., Ceppa, D. P., Rieger, K. M., & Kesler, K. A. (2014). The “cut-in patch-out” technique for Pancoast tumor resections results in postoperative pain reduction: a case control study.Journal of cardiothoracic surgery, 9(1), 163.