Concussion & Dr Jessica Schwartz
Recently I listened to a two-part podcast hosted by Therapy Insiders Podcast on the discussion of concussion with guest speaker Dr. Jessica Schwartz. It was a brilliant discussion about the current updates on this topic and I thoroughly enjoyed hearing about Dr. Schwartz's personal journey with concussion, profession experience and current role in managing concussion injuries and promoting concussion awareness world wide.
Dr. Jessica Schwartz, PT, DPT, CSCS is program director for the Evidence In Motion Concussion Certification, an orthopedic residency trained doctor of physical therapy, a national spokeswoman for the American Physical Therapy Association, and a post-concussion syndrome survivor, advocate and concussion educator.
You can access Part 1 Podcast & Part 2 Podcast here and the purpose of this blog is to briefly discuss some of the key points that were most interesting to me. Dr. Schwartz discusses a very complex condition is such an easy-to-understand manner and expresses her commitment to sharing information. Sharing of information, education of health professionals and connection with our community are all values that drive our blog, so to listen to such an experienced clinician share the same values was encouraging and inspiring.
I became most interested in concussion injuries when I first became involved with the Olympic Winter Institute of Australia as a travelling Physio for the Para-Alpine team. In the arena of winters sports concussion is a injury that athletes risk obtaining as much as any other injury. The speed they race and the environment they race in increases this risk of sustaining a head injury with crashes significantly. So the first comment that Dr. Schwartz made which caught my attention is that there is no distinct or uniform mechanism of injury that results in a concussion.
A concussion is a transient mild traumatic brain injury that is only deemed to be transient once neurological symptoms resolve. Often a concussion can result in a functional brain injury rather than an observable structural one. A concussion can be caused by linear or rotational forces, from direct blows to the head and sub concussive blows to the body. The degree of force does not correlate with the severity of symptoms. To sustain a concussion you do not need to be hit in the head and most importantly, loss of consciousness does not need to happen for a concussion to occur. There is no stereotypical pattern of clinical presentation when it comes to this disorder, no strict mechanism of injury, and definitely no distinct recovery pathway or prognosis. Each person must be assessed individually.
Concussion is truely a clinical diagnosis. "There is no single test to diagnose this condition and no series of tests that outperform an experienced clinician" (Dr. Schwartz). For us to completely understand the impairments that affect each individual, we need to consider that there are six clinical trajectories occurring from a concussive incident that may result in vestibular, oculomotor, migrainous, cervical, cognitive and affective impairments. In the case of a severe traumatic brain injury a patient would most likely be managed in an inpatient setting with access to a diverse team involving a physician, neuropsychologist, speech pathologist, occupational therapist, nurse, team coordinator, family members and us (the physical therapist). But concussions are often managed in a community setting. Even though their impairments can cross multiple clinical domains, they often don't receive the same multidisciplinary and coordinated care. It is even more important therefore for Physical Therapists to understand the complexity of concussions in order to identify where other professionals may need to be involved in rehabilitation.
For many injuries in the body, Physiotherapists are urged to view patients from a biopsychosocial approach. To address each individual in the context of their lives and to do our best to treat the impairments we are able to help them with. For concussion, this approach is paramount in achieving successful outcomes.
Dr. Schwarz emphasises that 'we can't pull people apart and take away the biopsychosocial aspects of the condition'. Instead we really need to focus on understanding the pre-morbid history of the person and the post-injury issues they are dealing with. Concussion doesn't result in a distinct set of symptoms and effects many interacting systems, as mentioned above. These symptoms are often difficult for people to describe to begin with and therapists need to listen, with a non-judgmental ear, to truely hear and understand what it is their patients are suffering from. Having the skills to take a "exquisite history" and truely understand the premorbid lifestyle and health of each person will enable us to better identify what conditions/issues can decompensate following injury.
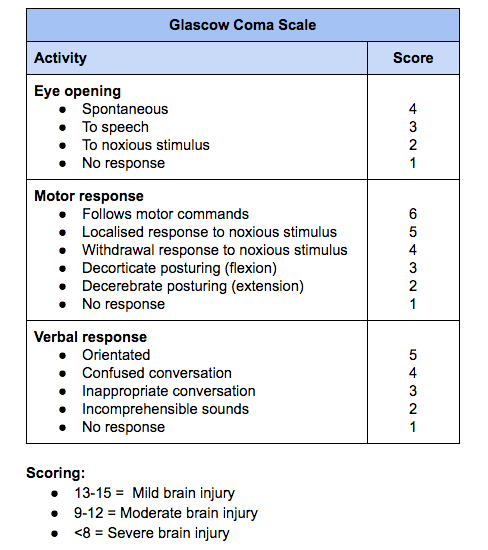
Initial severity of injury is often determined by using the Glascow Coma Scale, however for mild brain injury the injuries can be missed if the person is responsive, alert and orientated. Therefore we need to use other assessments beyond the GCS to determine presence and severity of impairments. Outside a thorough musculoskeletal and neurological examination there is also the need for each therapist to understand the details of a vestibular and oculomotor examination. Some outcome measures can assist with our diagnosis and gathering of objective data that Dr. Schwartz recommended the BESS, SCATT 3 and King Devick test.
I really enjoyed these two podcasts and the sharing of knowledge from both the hosts and guest speaker and I encourage you to take the time to listen in and understand more about the complexities of concussion as a condition but also the challenges that clinicians face when treating people suffering from post-concussion syndrome.
Some of the resources that Dr. Schwartz recommended are below:
Previously I've written on the topic of concussion specifically in the context of the winter sport environment, which aims to look more deeply at the initial assessment and patient interview involved.
Concussion injuries can result in long term deficits and often appear to be benign injuries at onset, so I urge you to be aware of the primary symptoms in the hope that we can all become better at recognising and more appropriately managing these injuries.
Sian