Surgery for Sciatica - a clinical commentary with Dr Lynn Bardin
In a previous blog on lumbar disc herniation with radiculopathy, I presented a case of conservative management of a patient with low back pain with radicular leg pain. This blog aims to explore how the science of clinical anatomy combined with our clinical assessment and decision-making process can be used in diagnosis and management, including referral for a spinal surgery consultation.
For this Dr Lynn Bardin, who lectures and tutors clinical anatomy at Melbourne University and works as a consultant spine physiotherapist at SUPERSPINE and at Austin Health, Melbourne, was invited to contribute a clinical commentary. She has chosen to link this to a case report from the 2015 Austin Health LifeSciences Research week (Bardin & Davis, 2015) that focused on physiotherapy and neurosurgery collaboration leading to optimal outcomes for a patient with severe, persistent and disabling radiculopathy. There are key elements that enhance our clinical understanding and guide us in the management of patients with ‘persistent sciatica’.
The poster summary of this case (Bardin & Davis, 2015) depicts a 32 year old man with severe, persistent radiculopathy and in the second column you will find clinical features of his presentation. These features are key aspects of the clinical presentation that would inform clinical decision-making regarding a possible referral for spine surgery. By posing 4 questions arising from this case and answering them, we hope, together, to facilitate important ‘take home messages’ which will be summarised at the end.
- Why should the term ‘lumbosacral radicular syndrome’ and not ‘sciatica’ be used in clinical diagnosis?
- What is 'enhanced specificity of surgical referral' ?
- What were the indications for surgical referral in this case report?
- What was exceptional about this patient’s recovery?
Q1: Why should the term ‘lumbosacral radicular syndrome’ and not ‘sciatica’ be used in clinical diagnosis?
‘Sciatica’ is a MeSH (Medical Index Subject Heading) term. It is defined as: “Condition characterised by pain radiating from the back into the buttock and posterior/lateral aspects of the leg. Sciatica may be a manifestation of sciatic neuropathy; radiculopathy (involving the spinal nerve roots; L4, L5, S1 or S2, often associated with intervertebral disk displacement); or lesions of the cauda equina”. It appears extensively in the literature and is generally understood by both clinicians and patients as being lumbar spine related ‘referred pain’ to the leg. However, not all referred pain is radicular pain (which is far more disabling) and the definition is wide and not specific to nerve root involvement. Reports in the literature of the prevalence of ‘sciatica’ ranging between 1.6% and 43% (Konstantinou, 2008) have led to comments by researchers emphasising the discrepancies in how sciatica is defined and diagnosed. Because of this the term ‘true sciatica’ is sometimes used to refer to radicular pain.
Lumbosacral radicular syndrome is a more explicit term. As our understanding of this condition sharpens to be more accurate in terms of both the clinical features and related patho-anatomy, it is helpful if we move away from the term ‘sciatica’ and embrace ‘lumbosacral radicular syndrome’.
Each of the 3 components of lumbosacral radicular syndrome adds understanding to this term. We shall summarise this briefly.
- Lumbosacral: Sciatica does not, by definition, include L1, L2, or L3 nerve root associated pain to the groin, anterior thigh or knee. By contrast, ‘lumbosacral’ incorporates any of the potential nerve roots (from the entire lumbosacral plexus, thus L2-S3) involved in dermatomal pain location (referred pain to the leg).
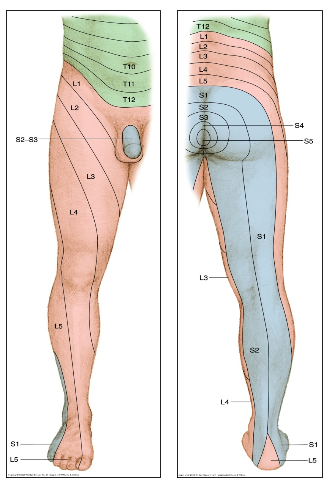
- Radicular: This is the term used to describe neurogenic/nerve root pain with its associated dermatomal pain location (Figure 1). (The relevance of this as a key item in the history and its importance in specificity of surgical referral is discussed later under question 3).
- Syndrome: This term denotes the clinical presentation of patients who have lumbosacral radicular syndrome. Debilitating radicular leg pain is the most frequent symptom, but is often associated with muscle weakness, sensory deficits and functional impairment (Luijsterburg et al 2007). ‘Syndrome’ perhaps captures the variance of clinical presentation e.g. can vary from a patient with severe radicular pain (but no motor deficit) to a patient with a painless footdrop.
It is important to recognise that the term sciatica is still widely used by practitioners and is easily understood by patients. Sciatica is a term that has been around a long time. Changes in nomenclature are slow to gain traction. Who of you reading this, for example, knows the new name for Ankylosing spondylitis? The use of sciatica is likely to persist, however as clinicians there is some advantage for us to use the term lumbosacral radicular syndrome. It will help us to educate patients about their symptoms and neurological examination findings, in a more scientifically accurate way, and explain treatment directed at pain relief, movement dysfunction and motor deficits.
Q2: WHAT IS ‘ENHANCED SPECIFICITY OF SURGICAL REFERRAL’?
Often referrals to spinal surgery lack specificity (Huang et al 2008; Coyle et al 2008). There are five factors that are commonly used in surgical decision-making and referrals that summarise this information have ‘enhanced specificity’. In a Canadian study it was found that less than 1% of referral letters contained information on all 5 of these factors and almost 25% of all referral letters did not mention any of them (Coyle et al 2008). We present the 5 factors with brief notes for each one as pertains to this case presentation.
Figure 1: Distribution of dermatomes (Hancock, 2011)
1. Dominant location of pain
Radicular pain is the most common key clinical feature of patients with lumbosacral radicular syndrome. In spite of this being a ‘symptom’ (subjective), not a ‘sign’ (objective), it has been shown that dermatomal pain location is the most informative individual item from the history and neurological examination to clinically determine the level of a possible disc herniation (Hancock 2011). The implication for clinicians is that interpreting dermatomal pain location is very important information when taking a patient’s history (to make an accurate clinical diagnosis). The clinical diagnosis, for example S1 radiculopathy (due to suspected L5/S1 disc extrusion) and structural/radiological diagnosis, for example MRI indicating a right postero-lateral L5/S1 disc extrusion, right S1 nerve root compression, congenital spinal stenosis and hypertrophy of the ligamentum flavum, may ‘match’, but this is not always the case.
2. Severity of symptoms.
Radicular pain is typically severe and debilitating. In this case it was rated as 9/10. Leg pain far more intense than back pain is typical of radicular pain and is associated with good outcomes following microdiscectomy. Part of the severe nature of radicular pain is the tendency for latent pain (flares up badly but as a delayed response to provocation). This reminds us to be careful when examining patients with a clinical presentation that is potentially ‘irritable’
3. Neurological findings.
- Plantar flexion weakness (due to S1 nerve root deficit - part of the innervation of the tibial nerve)
- Absent ankle reflex (S1, S2)
- Straight leg raise limited to 40 degrees
- These signs from the neurological examination suggest a clinical diagnosis of S1 nerve root pathology. A structural diagnosis, for which an MRI/CT scan is needed, assists our understanding regarding the patho-anatomy/probable cause i.e. lumbar disc extrusion/sequestration with associated foraminal/central canal stenosis.
4. Duration of symptoms.
- This patient suffered from persistent pain for 12 weeks duration, which is significantly beyond the normal recovery time for lumbosacral radicular syndrome.
5. Previous treatment.
- The patient had not improved with pain medication, resting and a few physiotherapy sessions (elsewhere before presenting to the SUPERSPINE clinic). The patient also reported that his function had deteriorated over time and his ability to manage his pain had reduced. He was recumbent most of every day.
Q3: WHAT WERE THE INDICATIONS FOR SURGICAL REFERRAL IN THIS CASE report?
In this case the patient presentation was clearly supported by signs and symptoms enabling a diagnosis of lumbosacral radicular syndrome. Because the clinical diagnosis and the radiological diagnosis matched well, and there were specific clinical features to support a referral for neurosurgery, this was relatively easy to motivate.
Key reasons to seek a neurosurgical opinion for this case were:
- Severe, persistent radicular pain lasting already present for 12 weeks
- Matching clinical diagnosis of S1 radiculopathy and structural/radiological diagnosis (MRI findings of L5/S1 disc extrusion)
- Persistent, severely antalgic posture
- Patient was young and not able to work at all
Clinical pathways are continuing to be developed in the hope that we can improve our triage process and identification of the best candidates for a surgical review. Dissapointingly, one of the common reasons that patients are referred to a neurosurgeon or spinal surgeon is because they have failed to improve with conservative treatment, however, this doesn't necessarily mean that they are a suitable candidate to receive surgical treatment (Wilgenbusch, et al., 2014). When determining if a referral is required or not, one must consider a) what are the indications for a referral, and b) what is the aim/expectation for outcomes of this referral? Otherwise the sheer number of referrals overloads the system and results in extended waiting times.
Canadian advances in surgical referral: the Saskatchewan Spine Pathway (SSP).
In 2010, the Saskatchewan Spine Pathway (SSP) was introduced in Canada, a multidisciplinary triage process which aims to more accurately identify surgical candidates than conventional processes. There have been several studies investigating the utility of this approach (Fourney, et al., 2011; Kindrachuk, et al., 2014; Wilgenbush, et al., 2014). What these studies found was that the SSP is more like to identify patients with leg-dominant pain, more like to accurately identify people who will benefit from a surgical consultation, and more likely to reduce the utilisation of MRI (Kindrachuk, et al., 2014; Wilgenbusch, et al., 2014). It seems that many countries are currently exploring ways to make our assessment processes more accurate in the hope of reducing wait list times, improving the referral process, reducing costly medical imaging procedure, and better directing patients towards their optimal treatment pathway.
The Saskatchenwan Spine Pathway offers a different assessment algorithm to ones that we commonly use in Australia. The SSP aims to categorise patients into one of four categories (inter-rater reliability of 76%)(Fourney, et al., 2011, p. S166):
- Pattern 1: Back dominant pain aggravated by flexion (this pattern is divided into two groups):
- a - Fast responders: Increased pain on flexion and relief with unloaded passive lumbar extension
- b - Slow responders: Increased pain on flexion and extension.
- Pattern 2: Back dominant pain aggravated by extension but not increased with flexion
- Patterns 3: Leg dominant pain that is constant, associated with positive neurological findings and aggravated by back movement.
- Pattern 4: Leg dominant pain that is intermittent, aggravated by activity in extension and relieved by rest in flexion.
What this study found is that patients presenting with pattern 1 or 2 are best suited for a referral for conservative treatment and referral for a surgical consultation if symptoms persist after 6 weeks of mechanical treatment. Pattern 3 indicated an urgent referral and pattern 4 a less-urgent referral. What you may realise after reading this is that while it helps to prioritise patients for surgical referral, it doesn't outline what the assessment process is, which is a limitation of this pathway in my mind.
The clinical reasoning process I, Sian, have been educated to determine if a referral is required is based on the presence of the following features (Ford, Hahne, Chan, & Surkitt, 2012; Jacobs et al., 2011; Koes, Van Tulder, & Peul, 2007; Luijsterburg, et al., 2007; Van der Windt, et al., 2010):
Clinical examination:
- Distribution of symptoms
- Unilateral leg pain greater than low back pain.
- Pain radiating in a dermatomal pattern, below the knee and into the foot or toes.
- Numbness & paraesthesia in the same distribution as pain.
- Positive signs on neurodynamic and neurological examination i.e. neurological deficits including muscle weakness, sensory loss/changes, and/or changes in reflexes.
- Reproduction/increase in pain with straight leg raising, slump test, or prone knee bend (neurodynamic tests).
- Positive findings on MRI and CT imaging indicating nerve root compression.
Q4: WHAT WAS EXCEPTIONAL ABOUT THIS PATIENT’S RECOVERY?
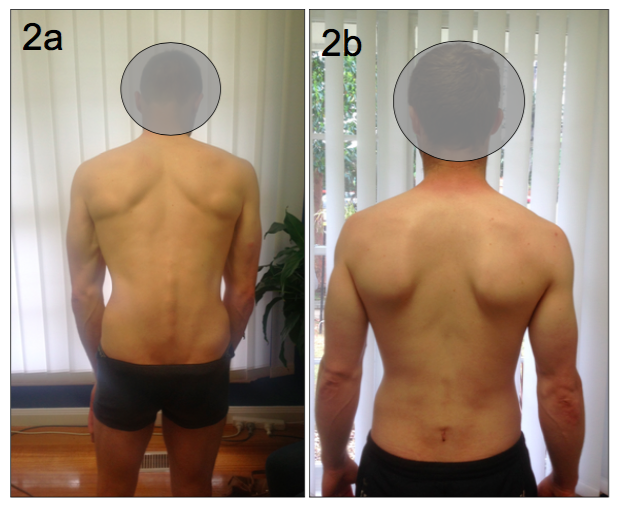
This image demonstrates the antalgic posture of the patient before and after surgery. How would you interpret this posture? Commonly, when you think of antalgic postures for low back pain, you might think about lists or shunts. From this image you can see something completely different. There is a complete loss of lumbar lordosis. There is also flexion at the hips and knees, sometimes referred to as a ‘Simian stance’. From a clinical anatomy perspective this can have three distinct effects on the lumbar spine.
- The spinal canal dimensions are altered by adopting a flexed position that increases both the central canal space and intra-foraminal cross-sectional area (Penning,1992).
- There is an associated posterior pelvic tilt related to the lumbar flexion, which affects gluteal muscle activation patterns and impacts lumbo-pelvic stability.
- Loss of lumbar lordosis causes the posterior muscles of the spine (extrinsic lumbar muscles such as lumbar erector spinae & intrinsic lumbar muscles such as rotatores and multifidus) to be placed in a lengthened position, which compromises their dynamic support of the spine.
What is exceptional about this patient's recovery is how well the patient could stand in a normal posture immediately post surgery. The disc extrusion, which was the cause of the radiculopathy, can be viewed as a space occupying lesion. Once removed, the adaptive antalgic posture spontaneously normalised. This is a great example of when the correct patient is selected for surgical management of persistent, disabling radiculopathy. The patient was working full time by 12 weeks post surgery and at the 6 month follow-up reported no pain, full function on the Roland Morris Disability Questionnaire, and had returned to work without restriction. Just a remarkable recovery.
Another aspect of this patient's management which is remarkable, is how quickly the patient was selected for surgery following the physiotherapy-led assessment. Patients can often face a long treatment pathway with poorly co-ordinated treatments, conflicting advice and a variety of treatment options (Wilgenbusch, et al., 2014). However, in this case a clinical-reasoning decision making process was used to enhance the specificity of the referral, which allowed the patient to receive the best treatment in a shorter timeframe than most. Many of the clinical pathways that currently exist aim to improve communication and collaboration, reduce wait-list times and help direct the patient towards the best resources and treatment pathways. While the validity of such clinical pathways remains an ongoing process, this case study reinforces the positive outcomes that can occur when such processes are refined and well executed within the primary care setting.
CONCLUSION
Collaborating to write about this topic has been a valuable learning experience for both of us and we hope we have provided a good clinical context for the following take home messages:
- Lumbosacral radicular syndrome is a clinical diagnosis that can be made based on a cluster of signs & symptoms. A detailed history and clinical examination with attention to accuracy of the neurological examination are essential in the diagnostic process. A matching structural/radiological diagnosis will strengthen the case for a surgical referral.
- Referrals for a spine surgery consultation should contain the 5 factors that will enhance specificity. These are dominant location of pain, severity of symptoms, neurological findings, duration of symptoms, and previous treatment (Simon et al 2009).
- In an attempt to foster positive collaboration between physiotherapists and neurosurgeons, the physiotherapy profession should strive for high quality referral letters to spine surgeons/GPs.
- Surgical intervention in carefully selected cases of lumbosacral radicular syndrome can lead to rapid recovery and optimal patient outcomes.
Sian & Lynn
References:
Bardin, L.D., Davis, G.A. (2015). Physiotherapy and neurosurgery collaboration: case report illustrating efficiencies with optimal patient outcomes. Austin LifeSciences Research Week.
Clare, H., Adams, R., & Maher, C. (2003). Reliability of detection of lumbar lateral shift. Journal of manipulative and physiological therapeutics, 26(8), 476-480.
Cohen, S. P., & Raja, S. N. (2007). Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. The Journal of the American Society of Anesthesiologists, 106(3), 591-614.
Ford, J. J., Hahne, A. J., Chan, A., & Surkitt, L. D. (2012). A classification and treatment protocol for low back disorders Part 3‐Functional restoration for intervertebral disc related disorders. Physical Therapy Reviews, 17(1), 55-75.
Fourney, D. R., Dettori, J. R., Hall, H., Härtl, R., McGirt, M. J., & Daubs, M. D. (2011). A systematic review of clinical pathways for lower back pain and introduction of the Saskatchewan Spine Pathway. Spine, 36, S164-S171.
Hahne, A., Ford, J., Surkitt, L., Richards, M., Chan, A., Thompson, S., et al. (2011). Specific treatment of problems of the spine (STOPS): design of a randomised controlled trial comparing specific physiotherapy versus advice for people with subacute low back disorders. BMC musculoskeletal disorders, 12(1), 104.
Hancock, M. J., Koes, B., Ostelo, R., & Peul, W. (2011). Diagnostic accuracy of the clinical examination in identifying the level of herniation in patients with sciatica. Spine, 36(11), E712-E719.
Jacobs, W. C., van Tulder, M., Arts, M., Rubinstein, S. M., van Middelkoop, M., Ostelo, R., et al. (2011). Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. European Spine Journal, 20(4), 513-522.
Koes, B. W., Van Tulder, M. W., & Peul, W. C. (2007). Diagnosis and treatment of sciatica. BMJ: British Medical Journal, 334(7607), 1313.
Konstantinou, K., & Dunn, K. M. (2008). Sciatica: review of epidemiological studies and prevalence estimates. Spine, 33(22), 2464-2472.
Luijsterburg, P. A., Verhagen, A. P., Ostelo, R. W., van Os, T. A., Peul, W. C., & Koes, B. W. (2007). Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. European Spine Journal, 16(7), 881-899.
Macedo, L. G., Smeets, R. J., Maher, C. G., Latimer, J., & McAuley, J. H. (2010). Graded activity and graded exposure for persistent nonspecific low back pain: a systematic review. Physical Therapy.
Maitland, G. D., Hengeveld, E., Banks, K., & English, K. (2005). Maitland's vertebral manipulation: Elsevier Butterworth-Heinemann Edinburg.
Penning, L. (1992). Functional pathology of lumbar spinal stenosis. Clin Biomech, 7(1), 3-17.
Peul, W. C., Brand, R., Thomeer, R. T., & Koes, B. W. (2008). Improving prediction of “inevitable” surgery during non-surgical treatment of sciatica. Pain, 138(3), 571-576.
Simon, D., Coyle, M., Dagenais, S., O’Neil, J., & Wai, E. K. (2009). Potential triaging of referrals for lumbar spinal surgery consultation: a comparison of referral accuracy from pain specialists, findings from advanced imaging and a 3-item questionnaire. Canadian Journal of Surgery, 52(6), 473.
Van der Windt, D. A., Simons, E., Riphagen, I. I., Ammendolia, C., Verhagen, A. P., Laslett, M., et al. (2010). Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain (Review). Cochrane Database Syst Rev, 2(2).