Meet Marnie...Central Sensitisation Case Study
I had often read the theory of central sensitisation, told to look for signs of "central sensitisation" during my subjective and physical assessment. However, I had rarely seen a true "central sensitisation" patient...until I treated Marnie. This blog outlines her story, her clinical presentation, her descriptors of the condition, failed management and the management journey I undertook with her.
Marnie...
Marnie was walking down a street, tripped over some uneven paving and landed on hands and knees, twisting her right knee during the fall. Her initial pain was located in bilateral wrists from the impact and a sharp pain with constant achiness in the right medial knee. Three days later, this vague aching with intermittent sharp pain on loaded knee flexion (squatting, stairs, walking etc) became an intermittent burning. Marnie saw a general practitioner (GP) who referred for a knee MRI, which confirmed a medial meniscus tear. Treatment then consisted of unloading, some isolated quadriceps strengthening, range of motion exercises and education.
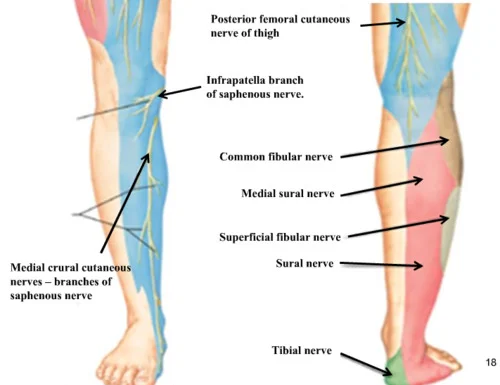
Marnie presented to our clinic after three months of physiotherapy treatment, with no change in symptoms. She was still experiencing the medial knee sharp pain, but was more concerned about the constant burning in the pes anserinus region, present on weightbearing and lingering at rest. It was slightly sensitive to clothing, especially the seams of pants, and worsened with hot showers or heat packs. The initial assessment determined Marnie had a neural irritation to the infrapatella branch of the saphenous nerve.
Infrapatella Branch of Saphenous Nerve, location of Marnie's neural irritation (image courtesy of google.com)
She was then referred to a pain specialist, to deal with the neural symptoms. The pain specialist believed there was inflammation surrounding the nerve and proposed a cortisone injection to the surrounding tissue to relieve her symptoms. Marnie had four hours of complete symptom relief, nil burning or sharp pain. However, the burning, prickling pain then returned at P8/10 and spread from her medial knee region to her medial shin and medial half of the foot. Her aggravating factors included any movement of the right leg, any weightbearing, any objects touching her skin and the thought of someone touching her leg.
She was placed on Lyrica, Endep, Temazepam, Panadeine Forte and various other medications, with varying dosages to assist with pain relief. Marnie attempted hydrotherapy but the pressure and temperature of the water exacerbated the burning and did not settle for 48 hours. She was also attending "stress management" sessions with a psychologist, as her work schedule and busy lifestyle also exacerbated her pain. Marnie believed this slightly eased the pain.
It is here that I first met Marnie...
Theory Into Practice
I first saw Marnie when my colleague was away on holidays, her presentation was interesting and I believed I had certain strategies which could assist her.
Day 1...Objectively...
- Her left (unaffected) straight leg raise (SLR) was 10 degrees plantarflexion, 0 degrees hip flexion, P1 left medial knee P9/10. I did not assess her right SLR, due to this finding.
- Thessaly meniscus test (right) was positive at 20 degrees knee flexion, reproducing the sharp P8/10 medial knee pain but not affecting the constant burning.
- Her left L1-5 region was allodynic to light touch, reproducing P8/10 locally and in the right knee.
- Her Recognise Foot App score was L 60%, R 69%, L 2.9s, R 3.1s, 14/20, a normal response is about 1 second, with 18+/20 considered normal.
- Upper chest breathing pattern
- Nil isometric gluteal activation in stand or prone
Initial Treatment...
My initial treatment consisted of teaching diaphragmatic breathing in prone, with Marnie's shirt off. This reduced the tactile stimulation to the allodynic left lumbar region. We retrained gluteal activation, by using posterior pelvic tilting to gain gluteal firing. Again, this small movement in a 'safe' position, to an area distant to the affected knee regions, slightly reduced the pain at the right knee. Marnie was to download the Recognise app and complete five 'games' at home daily, in addition to practicing her diaphragmatic breathing and 'butt squeezes'.
Burning Pain
Day 2...
Marnie returned with no change in her symptoms, still experiencing a constant burning, shooting 8/10 pain in the right leg. She had not downloaded the Recognise yet, so had not completed any repetitions. Marnie also mentioned she had started dropping things (such as pens, fork) from her right hand, and felt less strong and clumsy using her right hand. This led me to assess her two-point discrimination in her hand, which found...
- Left hand 2-point discrimination was 2mm, her right hand was 43mm.
My day two treatment consisted of five repetitions of the Recognise foot app, however this exacerbated her right knee pain. I then tried mirror box therapy placing the right hand behind the mirror, only moving the left hand...after 30 seconds of left hand movements, Marnie experienced burning pain from her right cervical spine to right hand, although no right hand movement occurred. I also instructed Marnie to perform hand tactile activities, such as squeezing a stress ball and playing with hand putty.
At this point, I felt overwhelmed and referred Marnie to Peter Selveratnam (FACP), and attended the session with her for a specialist opinion!
With Peter Selveratnam...
Peter Selveratnam, Specialist Musculoskeletal Physiotherapist.
The session with Peter consisted of a very thorough subjective examination, with Peter using various highlighters to colour code Marnie's various pain patterns. The physical assessment was quite interesting, some aspects were similar, however the differences are noted below:
- Light touch with tissue on bilateral big toes, medial shin, medial knee, anterior thigh, abdomen, deltoid, sternocleidomastoid, earlobe and forehead. All areas reproduced right medial knee pain and burning to the right 1st toe.
- Ice spray to the right medial knee reproduced an excruciating 10/10 from knee to foot.
- Peter also performed some cranial nerve tests and vestibular testing, which were NAD.
Peter believed Marnie had severe central sensitisation, with associated Complex Regional Pain Syndrome. He offered various management strategies including: hydrotherapy, dots on a mirror and following them with her unaffected hand, performing the Recognise hand app (which would be less provocative than foot, more distant to the affected area), continuing with her medications, continuing stress management classes and altering her work hours.
Peter also reinforced the notion of "no quick fix", there were central changes and a very alert, active neural/pain system which would take time to reverse.
Back in the Clinic...
Our next session, Marnie described her experience driving the previous weekend. She stated she was acutely aware of anything that happened on her right, for example a car overtaking her on her right side, while she was slow to notice anything happening on her left side. In opposition, while very perceptive to her right side, she had a delayed reaction on her right. So if a car suddenly appeared on her right side, she would immediately notice it but would have a few seconds delay in placing her foot on the brake. This created the perfect analogy for what was happening in her brain, she was hypervigilant on her right side, with slight left sided 'neglect', but had delayed motor activity and impaired processing on her right side.
Treatment consisted of sitting Marnie in front of a mirror, with her legs out of vision, and placing dots on the mirror corresponding with her eye, forehead, ear and chin. She then used her left hand to point to eye-chin-ear-forehead, eye-ear-forehead-chin etc. It took Marnie approximately 8 seconds to complete one circle, this slowly improved to 6 seconds after five repetitions. Marnie commented, "It sounds weird, but I feel like my brain is underwater and I know what I'm meant to do but I'm really slow in doing it, like a dream where you're trying to yell out but you can't." Marnie was to complete this exercise at home, at least five times a day.
Finally...
Marnie entered her last appointment, stating "I'm moving to Germany for work." She was very excited to be returning to her family and felt this could relieve some anxiety. She felt reassured that the pain could eventually get better, and felt she had management strategies to assist in all aspects of her condition. We also discussed continuing with a pain specialist in Germany, continuing her stress management, Recognise hand app and the mirror dot therapy. She was encouraged to attempt hydrotherapy in lukewarm water once she felt comfortable with water, and no longer threatened.
Life Lessons...
These patients are not simple, there are many complex genetic, chemical, neurological and psychological factors at work. So what did I learn??
- Listen to the patient...being an ear of empathy was why Marnie trusted me.
- Try one technique at a time...often the response is latent, if a technique increases their pain, the perceived threat, therefore perceived pain, increases.
- These are complex patients, don't be afraid to refer on or ask for a specialist consultation.
- Use technology...Recognise apps, youtube videos of Lorimer Moseley explaining pain, the NOI Group website, youtube videos of Peter O'Sullivan treating patients etc...use what you have available to explain to your patient what is happening.
Hopefully, this case study provides an insight into a complex pain patient, and highlights there are no quick fixes. If you wish to learn more about this subject, there is a Pain course (Assessment and Management of Pain in Clinical Practice) being run by MPA (VIC Branch) in Melbourne on the 6th and 7th of December. The presenters include Alastair Flett, Peter Roberts and Lester Jones, providing an absolute wealth of knowledge in the field of pain. I am really looking forward to attending this course.
Alicia