Pregnancy Related Pelvic Girdle Pain
Pelvic girdle pain experienced following pregnancy is very common, but what is the source of the pain, and what factors need to be addressed? Although there are anatomical and physiological factors to address, if the ‘yellow flags’ aren’t considered, full recovery will be challenging. This post provides an overview of these changes and the current research regarding the pain source in pelvic girdle pain postpartum.
Anatomical Factors
Pregnancy-related pelvic girdle pain (PGP) is difficult to define as the aetiology and pathoanatomical source of the pain are challenging to localise, with various clinical presentations causing similar pain patterns.
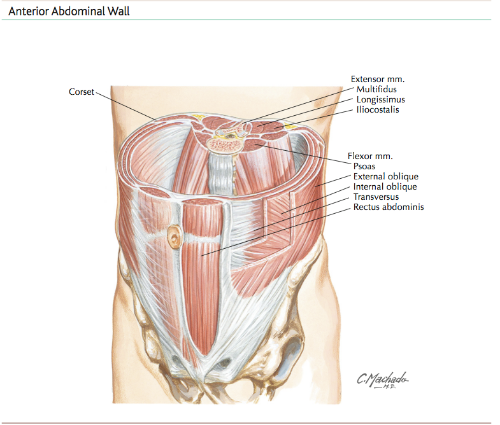
The sacroiliac articulation is inherently unstable, with a wedge shaped structure sitting adjacent to the ilium, relying heavily on passive stabilising structures and both local and global muscle activity to increase stability and allow normal function (Vleeming et al, 2012). The literature describes the co-asctivation of TrA, multifidus and pelvic floor with the global musculature of lat dorsi, thoracolumbar erector spinae, internal obliques and glute max to provide a force coupling, compressing and ultimately stabilising the SIJ (Vleeming et al, 2012).
Lumbopelvic stability is sustained by modulating the motor recruitment and activation patterns of the local and global lumbar muscles, through the central nervous system. They describe a pre-activation of the segmental trunk musculature, with the diaphragm and contralateral transversus abdominis and internal obliques activating before limb motion, to allow controlled fluid movement (Hungerford et al, 2003). Adding multifidus activation increases pelvic control in single leg weightbearing, through attachments to thoracolumbar fascia. Pubic symphysis stability is increased with adductor activation while glute max, lumbar ESpinae and lat dorsi activation increases SIJ compression (Hungerford et al., 2003).
An alteration to the bony or ligamentous structures would place greater mechanical load on the contractile tissue. A study by Bjorklund (1999, 2000) found a moderate correlation between women suffering from pregnancy-related PGP and increased pubic symphysis diameter, however no measurements were taken postpartum. The pain levels were unable to be used as a predictor for the width of the pubic symphysis, indicating a relationship is present but other pathophysiological processes are also occurring (Bjorklund et al., 2000). Damen et al (2001)found a strong correlation between unilateral sacroiliac joint laxity and PGP during and following pregnancy, although this was not bilateral. It appears the laxity is a result of unilateral motor dyskinesis rather than global ligamentous change following pregnancy. Hungerford et al (2003) found a delay in muscle activation of multifidus, internal obliquus and gluteus maximus on the stance leg when performing the Stork test, in individuals with sacroiliac joint pain, again proposing an altered stabilisation strategy on pelvic loading.
Additionally, the sacroiliac ligamentous structures have been reported as local pain-producing structures (Wu et al., 2004). Hungerford et al (2003) indicate these tissues prevent excessive pelvic motion, control the direction of movement and provide joint stabilisation and compression. Creep occurs in these ligamentous tissues when sustained loading is endured, so control must include both passive stability from ligaments and active stability from activation of lumbopelvic muscles to prevent creep (Hungerford et al., 2003).
Physiological Factors
Many physiological changes occur during pregnancy, with increased production of relaxin commonly mentioned. Earlier studies suggest these sex hormones have a role in altering collagen production affecting the ligamentous structures stabilising the pelvic girdle, however recent strong evidence indicates relaxin is not the cause of PGP (Aldabe et al, 2012; Kristiansson et al, 1999). Instead, O’Sullivan and Beales (2007a) propose the existence of other hormones in influencing pain modulation and the inflammatory process, possibly inducing heightened pain reception and prolonging the inflammatory response (Aloisi & Bonifazi, 2006).
Mens and colleagues (2009) found pelvic girdle motion to be 32% to 68% greater in those with PGP, in the first three weeks post partum, compared to the control group. This coincides with Damen’s (2002) findings of asymmetrical sacroiliac joint laxity in those with pelvic pain. Damen (2002) further states the degree of pain is not associated with the degree of laxity but the amount of difference between sides, with asymmetrically lax individuals being three times more likely to have their pain persist into the postpartum period. Also, Wu et al (2004) revealed pregnant patients with PGP had increased mobility in their thoracolumbar spine and pelvis on gait analysis. These findings enhance the suggestion that while relaxin and sex hormones are not the source of the pain, the resultant increased motion with secondary alteration in motor control is a cause of PGP and validates treatment to retrain pelvic movement patterns (Mens et al., 2009).
Psychological Factors
Any chronic injury is associated with psychological and cortical changes. O’Sullivan and Beales (2007a) specifically identify the presence of hyper-vigilance, fear avoidance behaviour, altered coping strategies, anxiety, pacing, depression and helplessness in pelvic girdle pain, among others. Hansen (2005) found individuals with pelvic girdle pain displayed poor coping strategies, compared to the control groups. Women exhibiting these behaviours may be at higher risk of developing chronic pelvic pain, ultimately becoming centrally sensitised (Zusman, 2013). Many therapists have identified fear avoidance as a contributor in pelvic girdle pain, affecting the transfer of load through the pelvis. Although not a primary mechanism for the pain, it can cause secondary alterations in muscle activation and motor control, perpetuating the asymmetrical pelvic stability associated with pelvic girdle pain (Beales, O'Sullivan, & Briffa, 2010).
These psychosocial issues have an ability to drastically alter the patient’s outcome, while these factors are not the primary mechanism of pain, they have the capacity to sensitise or amplify pain receptors and disability (O'Sullivan & Beales, 2007a). A patient with poor coping strategies, in the presence of pelvic girdle pain, may experience increased anxiety levels, damaging beliefs, fear avoidance and catastrophising causing a heightened pain response through central sensitisation, further perpetuating the pain cycle (O'Sullivan & Beales, 2007a).
A patient displaying these traits requires a biopsychosocial management plan, addressing the cognitive factors associated with a chronic pain disorder, endorsing accurate beliefs, activity modulation and active coping strategies (O'Sullivan & Beales, 2007a). If the negative cognitive features of pelvic girdle pain are unable to be resolved, psychological and medical intervention may be appropriate (O'Sullivan & Beales, 2007a). Until the psychosocial aspects of the condition are addressed, a therapist will have difficulty resolving the motor impairments, and altered movement patterning, associated with this disorder (Hansen et al., 2005).
The following blog post will address current evidence-based practice in treating pregnancy-related pelvic girdle pain.
Alicia
References
Bjorklund, K., Bergstrom, S., Nordstrom, M. L., & Ulmsten, U. (2000). Symphyseal distention in relation to serum relaxin levels and pelvic pain in pregnancy. Acta obstetricia et gynecologica Scandinavica, 79(4), 269-275.
Damen, L., Buyruk, H. M., Guler-Uysal, F., Lotgering, F. K., Snijders, C. J., & Stam, H. J. (2001). Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta obstetricia et gynecologica Scandinavica, 80(11), 1019-1024.
Damen, L., Buyruk, H. M., Guler-Uysal, F., Lotgering, F. K., Snijders, C. J., & Stam, H. J. (2002). The prognostic value of asymmetric laxity of the sacroiliac joints in pregnancy-related pelvic pain. Spine, 27(24), 2820-2824.
Hansen, A., Jensen, D. V., Larsen, E. C., Wilken-Jensen, C., Kaae, B. E., Frolich, S., . . . Hansen, T. M. (2005). Postpartum pelvic pain--the "pelvic joint syndrome": a follow-up study with special reference to diagnostic methods. Acta obstetricia et gynecologica Scandinavica, 84(2), 170-176.
Hungerford, B., Gilleard, W., & Hodges, P. (2003). Evidence of altered lumbopelvic muscle recruitment in the presence of sacroiliac joint pain. Spine, 28(14), 1593-1600.
Hungerford, B., Gilleard, W., & Lee, D. (2004). Altered patterns of pelvic bone motion determined in subjects with posterior pelvic pain using skin markers. Clinical biomechanics (Bristol, Avon), 19(5), 456-464.
Mens, J. M. A., Pool-Goudzwaard, A., & Stam, H. J. (2009). Mobility of the pelvic joints in pregnancy-related lumbopelvic pain: a systematic review. Obstetrical & gynecological survey, 64(3), 200-208.
Mens, J. M. A., Snijders, C. J., & Stam, H. J. (2000). Diagonal trunk muscle exercises in peripartum pelvic pain: a randomized clinical trial. Physical therapy, 80(12), 1164-1173.
O'Sullivan, P., & Beales, D. (2007a). Diagnosis and classification of pelvic girdle pain disorders--Part 1: a mechanism based approach within a biopsychosocial framework. Manual therapy, 12(2), 86-97.
O'Sullivan, P., & Beales, D. (2007b). Diagnosis and classification of pelvic girdle pain disorders, Part 2: illustration of the utility of a classification system via case studies. Manual therapy, 12(2), e1-12.
Vleeming, A., Albert, H. B., Ostgaard, H. C., Sturesson, B., & Stuge, B. (2008). European guidelines for the diagnosis and treatment of pelvic girdle pain. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society, 17(6), 794-819.
Vleeming, A., Schuenke, M. D., Masi, A. T., Carreiro, J. E., Danneels, L., & Willard, F. H. (2012). The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. Journal of anatomy, 221(6), 537-567.
Vleeming, A., Stoeckart, R., Volkers, A. C., & Snijders, C. J. (1990). Relation between form and function in the sacroiliac joint. Part I: Clinical anatomical aspects. Spine, 15(2), 130-132.