Adhesive Capsulitis - Pathology & Assessment
“difficult to define, difficult to treat and difficult to explain from the point of view of pathology" (D'Orsi, 2012)
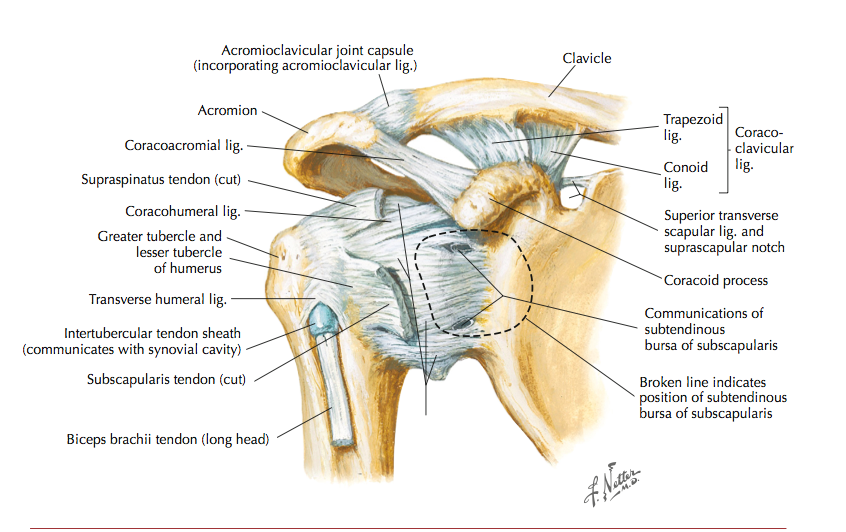
Adhesive capsulitis is a shoulder condition resulting in loss of active and passive ROM. It's a combination of synovial inflammation and capsular fibrosis. It can present as a poorly localised deep ache which may radiate to biceps or posterior humerus (if localised then could be joint capsule). There is progressive pain and stiffness into flexion, abduction and hand behind back. It can be primary or secondary due to an underlying condition (diabetes mellitus, rotator cuff tear/tendinopathy, subacromial bursitis, recent surgery etc). Neurological symptoms in forearm/hand are suggestive of a cervical radiculopathy not adhesive capsulitis.
Differential diagnosis, as always, is crucial in effective management.
The following table, from Ewald (2011, pg 418) shows these alternatives.
In particular, the following structures should be tested and cleared/excluded.
- AC joint - horizontal adduction with compression.
- Rotator cuff - Empty/Full can, RC strength testing, Neer's.
- Biceps LH tendon - Speed's, Yergason tests.
- Cervical spine - ROM, cervical quadrant, and PAIVM's.
- Neuro testing - cervical myelopathy, nerve root.
(Cleland, 2005, p.382)
Risk Factors include:
- Diabetes - independent predictor (1.2% of adhesive capsulitis in diabetes group vs 0.95% in non-diabetes group, study of 300,00+ subjects by Huang et al (2013), Tighe (2008) studied 88 patients with newly diagnosed adhesive capsulitis & no diabetic history, 39% had undiagnosed diabetes, 33% had undiagnosed prediabetes, 72% of total had diabetic relationship).
- Low BMI - independent predictor (for each kilogram underweight = 3% increase in risk (Wang, 2013)).
- Being born in British isles or parents/grandparents born there (1/4 of adhesive capsulitis vs 1/8 control from Britain (Wang, 2013)).
- First degree relative had adhesive capsulitis (30% of adhesive capsulitis vs 7% of controls (Wang, 2013)).
So how do we diagnose...it's primarily a clinical diagnosis, however imaging is useful to exclude other pathology.
- X-ray - no change evident.
- MRI - useful for thickening of coracohumeral ligament, joint capsule.
- Ultrasound - can detect coracohumeral ligament thickness, the presence of hypoechoic areas with vascularity correlates with inflamed tissue, can provide early/accurate diagnosis.
- Arthrography - assesses volume in joint, adhesive capsulitis = axillary fold is contracted reducing joint volume, however normal joint volume doesn't exclude adhesive capsulitis, may be false negative.
Adhesive capsulitis follows a clear clinical pattern but all other pathologies must be ruled out (tendons, AC joint, cervical spine) before this diagnosis is given. There is a definite link with diabetes, so the healing process can be delayed. In a patient with no diabetic history, it may be beneficial to refer them back to their GP for diabetic testing and appropriate management, given 70% of new adhesive capsulitis presentations have undiagnosed diabetes.
Further information regarding medial, surgical and physiotherapy interventions is to follow.
Alicia
References
Cleland, J. (2005). Orthopaedic clinical examination: an evidence-based approach for physical therapists. WB Saunders Co.
D'Orsi, G. M., Via, A. G., Frizziero, A., & Oliva, F. (2012). Treatment of adhesive capsulitis: a review. Muscles, ligaments and tendons journal, 2(2), 70-78.
Ewald, A. (2011). Adhesive capsulitis: a review. American family physician, 83(4), 417-422.
Huang, Y.-P., Fann, C.-Y., Chiu, Y.-H., Yen, M.-F., Chen, L.-S., Chen, H.-H., & Pan, S.-L. (2013). Association of diabetes mellitus with the risk of developing adhesive capsulitis of the shoulder: a longitudinal population-based followup study. Arthritis care & research, 65(7), 1197-1202.
Tighe, C. B., & Oakley, W. S., Jr. (2008). The prevalence of a diabetic condition and adhesive capsulitis of the shoulder. Southern medical journal, 101(6), 591-595.
Wang, K., Ho, V., Hunter-Smith, D. J., Beh, P. S., Smith, K. M., & Weber, A. B. (2013). Risk factors in idiopathic adhesive capsulitis: a case control study. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons ... [et al.], 22(7), e24-29.