Dry Needling or Acupuncture? Part 1 An interview with Dr Peter Selvaratnam
Introducing Dr. Peter Selvaratnam
I first met Dr. Peter during my Masters degree and what an inspiring teacher he is. I remember Peter was lecturing on modern concepts of neurodynamics and he had the whole class in stitches with laughter and we creatively explored the movements of the upper-limb that create neural sliding exercises. First impressions always last and for me Peter has always been humorouss, approachable and incredibly knowledgeable. Best of all, he loves sharing his knowledge and for this blog Peter is going to share his thoughts and experience about Acupuncture and Dry Needling.
Dr Peter Selvaratnam first qualified as a Physiotherapist and then completed a postgraduate programme in Musculoskeletal Physiotherapy, a Diploma in Acupuncture, a PhD in Medicine and later a Specialist Musculoskeletal Physiotherapist with the Australian College of Physiotherapy. Dr. Peter Selvaratnam is a Specialist Musculoskeletal Physiotherapist and an Associate Clinical Professor at The University of Melbourne. Peter has a PhD in Medicine in the field of Anatomy and is a Principal of The Melbourne Spinal and Sports Physiotherapy Clinic and The Headache Centre of Victoria. Peter with two other medical colleagues recently published a book with Elsevier on Headache, Neck and Orofacial Pain with a multi-disciplinary approach to headache management and orofacial pain involving medical and physical therapy management.
It is so exciting to meet a Physiotherapist passionate about pain, the spine, the nervous system, and someone who holds qualifications in both acupuncture and dry needling. I studied my Dry Needling Level 1 certificate with Peter and was shocked to realise how little I knew about the distinctions between these two treatment modalities. In Australia, Physiotherapists are not allowed to practice dry needling without Australian Physiotherapy Association - approved (APA) post-graduate qualifications, which is usually a 2-4 day course. However, not all countries have the same policies regarding dry needling and in many countries, Physiotherapists aren’t allowed to practice this treatment. This blog is a 2 part series. The aim of the first blog is to share some of that information with you to expand your knowledge about these treatment modalities and the second component is to understand what conditions and patient populations will benefit from these approaches.
Q1: What is acupuncture?
Acupuncture is part of Traditional Chinese Medicine (TCM) that treats patients by inserting solid, extremely fine, stainless steel needles into acupuncture points in the skin. They do not resemble the thicker needles used by western medicine practitioners and do not inject any soluble material.
Acupuncture has been practised for over 2500 years by Chinese medical practitioners. There is evidence that acupuncture has been practised in ancient Egypt, Persia, India, Sri Lanka, Arabia, many parts of Europe and South America, and by the North American Indians. The Eskimos, for instance, are still using sharpened stones for treating illness. In Brazil there is a tribe whose method of treating illness is to shoot tiny arrows from a blowpipe onto specific areas of the skin. However, it was the Chinese who perfected acupuncture and is considered as an alternative medicine. Traditional Chinese Medicine (TCM) like Western Medicine assesses and treats a variety of medical conditions and is not limited to musculoskeletal or neurological conditions.
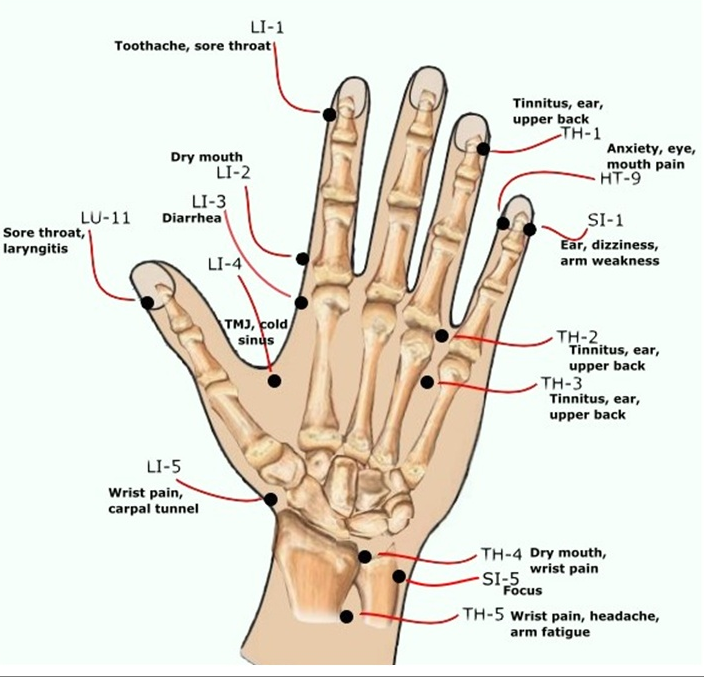
Image courtesy of Google Images
While Western medicine is based on biological and physiological paradigms,
- TCM originates in Taoism which is an Eastern religious philosophy.
- TCM is based on the yin and yang philosophy on which much of the foundation of Chinese medicine is based.
- Yin and yang are considered to be two fundamental forces of the cosmos that generate all transformation in the universe.
- The body is considered to be lined with invisible energy channels called meridians through which Qi energy is considered to flow.
- There are 12 major meridians and 8 special meridians in the human body along which Qi flows.
- Meridians do not conform to human physiology but are unseen conduits of Qi (Daniel Tong, 2003).
- Diseases are considered to result from Qi obstruction/deficiency resulting in yin/yang imbalance. Acupuncture along with moxibustion and herbal medicine are utilised as modalities to rebalance yin/yang and correct imbalances in the flow of Qi through meridians.
- There is no tangible Western medicine proof to the existence of meridians. Scientific research has not found any histological or physiological correlates for Qi, meridians and acupuncture points.
Image courtesy of Google Images
Acupuncture assessment includes:
- Assessment of Whole Person
- Tongue Diagnosis
- Pulse Diagnosis
- Meridians, Yin and Yang
- Acupoints, Ah-shi points
Current scientific research supports acupuncture’s efficacy in the relief of certain types of pain conditions and post-operative nausea. Other reviews have concluded that the positive results reported for acupuncture are too small to be of clinical relevance and may be the result of inadequate experimental blinding, or can be explained by placebo effects and publication bias. Other researchers have pointed out the difficulty in designing an adequate scientific control for any placebo effect acupuncture might have, due to its invasiveness.
There is general agreement that acupuncture is safe when administered by well-trained practitioners using sterile needles but does carry small risk of serious and adverse effects.
Image courtesy of Google images
The use of acupuncture for certain conditions has been tentatively endorsed by the United States National Institutes of Health, the National Health Service of the United Kingdom, the World Health Organization, and the National Centre for Complementary and Alternative Medicine though most of these endorsements have been criticised.
The concept of dry needling was “born” due to the Taoist spiritual basis of acupuncture.
The term ‘dry needling’ (DN) was initially described by Dr Chan Gunn of Canada in 1977. He is a Malaysian-Chinese medical practitioner who trained in Oxford University. He treated patients following the nerve model (referred to as the 'radiculopathy model'), suggesting that the patient’s musculoskeletal condition was due to nerve involvement. Treatment was followed using the concept of proximal spinal points, and distal points following the branches of the nerves. Deep dry needling of myofascial trigger points was first introduced by Czech physician Karel Lewit in 1979.
Image courtesy of Google Images on ear acupuncture (auriculotherapy).
DIFFERENCES BETWEEN TRADITIONAL CHINESE MEDICINE (TDM) & DRY NEEDlING (DN)
Acupuncture is based on Taoist spiritual paradigms while dry needling is based on Western medicine neurophysiological principles. The following table shows some of the comparisons between the two approaches.
2: What are the key features of dry needling?
The origin of DN was in 1977 by Dr Chan Gunn based on the nerve model to relieve pain and later by Dr Lewitt on treatment of muscle trigger points. Myofascial trigger points (MTPs) can be located within the muscle belly or at musculotendinous junctions. MTPs may consist of multiple contraction knots and were initially considered due to excessive release of acetylcholine (ACh) from selected motor end plates (Dommerholt et al, 2006). They are classified as active or latent, primary or associated. In certain countries, practitioners follow the radiculopathy model and in others, the MTP model. Some may even follow both models, while in Australia, practitioners have expanded from these two models.
Active MTPs are responsible for the pain generated in myofascial pain syndromes (Simons et al, 1999; Lucas, 2007). Latent MTPs are non-painful asymptomatic nodules that may contribute to restricted range of movement and muscle stiffness and have the potential to become active (Hong et al, 1998; Lucas, 2004; Lucas, 2007). They may however be painful on palpation. Primary MTPs occur within the muscle responsible for causing pain and may refer symptoms to specific regions associated with that muscle. Associated MTPs may occur in the region of the referred pain zone of a primary MTP. They could also occur due to increased functional demands of the associated musculature (Simons et al, 1999).
Subsequent studies by Shah et al (2005) found that the active myofascial trigger points have a biochemical milieu within the tissues. This biochemical milieu included norepinephrine, serotonin, bradykinin, interleukin-1, calcitonin-gene-related-peptide (CGRP), tumour necrosis factor, and substance P in its immediate milieu compared to normal muscle tissue. This investigation was the first to evaluate the biology of the MTPs compared to latent MTPs, normal muscle and the effect of dry needling an active MTP. Investigations into active MTPs and needling have found that the concentrations of this biochemical milieu in the immediate vicinity of the active MTPs reduces to normal levels after treatment.
However, the development of MTPs is currently considered due to input from the central nervous system (Bolton & Selvaratnam, 2009). Further investigations with event-related functional MRI suggests that patients with myofascial pain have an abnormal pain response to pain stimulus (Niddam et al, 2008). The activation patterns from the left upper trapezius in 16 fibromyalgic patients were compared to healthy controls when evoked from an ‘equivalent site’ stimulus intensity matched and pain intensity matched stimuli. The imaging was conducted in all subjects during needle and digital stimulation of the trapezius. Patients revealed significantly enhanced somatosensory (SI, SII, inferior parietal, mid-insula) and limbic (anterior insula) activity and suppressed right dorsal hippocampal activity, compared to asymptomatic people. The findings indicated that patients with hyperalgesia had abnormal brain activity in areas that processed stimulus intensity and negative affect. The authors speculated that suppressed hippocampal activity may reflect secondary stress-related changes in patients with chronic pain.
Importance of Local Twitch Responses (LTR)
- LTR is an objective sign that the clinician needs to identify in order to deactivate a MTP. It is an objective sign that there will be a chemical change at the MTP site (Karen Lucas, personal communication, 2008).
- Reproduction of the patient’s pain with the LTR is an important indicator that the MTP correlates to the patient’s symptoms.
- The more LTRs one elicits and the bigger the LTRs, the better the resolution of the MTP.
Melzack and Wall (1977) reported of a strong relationship between MTPs and acupoints and that 71% of MTPs coincide with ‘channel’ and ‘extra’ acupoints correlated with MTPs. The findings of Melzack and colleagues (1977) were refuted by Birch (2003). He reported that Melzack and colleagues' methodology was based on 'questionable assymptions'. Melzack et al (1977) assumed that acupoints must exhibit pressure pain and such pain reproduction was sufficient to correlate with MTPs (Birch, 2003; Dommerholt, et al., 2006). Birch found that only 18-19% of channel and extra acupoints examined by Melzack et al (1977) correlated with MTPs but they did not examine tender 'Ah Shi' acupoints. Hong (2000) and Audette et al (2003) surmise that acupuncturists may be treating MTPs when they needle 'Ah Shi' points. Dommerholt et al (2006) also emphasized that acupoints do not display the 'twitch'response of active MTPs and so cannot be categorized as the same. Active MTPs therefore have a clinical distinction from channel or extra acupoints (Selvaratnam, et al., 2009).
Mechanism of dry needling
There are only a few studies that have evaluated the effects of DN. The study by Huguenin, Brukner et al (2005) in Australia on the effect of DN of gluteal muscles in Australian Football League (AFL) players with hamstring injuries is one of the few randomised placebo controlled double-blind studies. Apart from this level 1 evidence based study, other studies in DN are level 2 or cohort or case controlled studies. Most neurophysiological studies on needling have been conducted on Acupuncture into acupoints and comparing with non-acupoints.
Image courtesy of Google Images of MTP of gluteus minimus
Image courtesy of Google Images of MTP of gluteus medius
Image courtesy of Google Images of MTP of gluteus maximus
Some of the theories on acupuncture which can be extended to dry needling are:
- Diffuse noxious inhibitory controls (DNIC). The primary nociceptive information of needling can be blocked by the application of a second new noxious stimulation which may then activate brain stem centres and descending modulatory pathways (Le Bars, et al., 1983).
- Local segmental effect. Needling depolarises large diameter afferents in lamina V of the dorsal horn and thereby inhibits nociceptive pathways conducted through the small diameter C nerve fibres (Le Bars, et al., 1979, 1983; Han & Terenius., 1982; Bogduk, 1989).
- Release of opiate peptides such as beta-endorphin, enkephalins and dynorphins (Terenius, 1985; He, 1987).
- Influence on sensory/motor cortex and pain modulating centres based on imaging studies.
- Influence on sympathetic nervous system.
- Neuromuscular response of myofascial trigger points (MTPs).
Now that we've discussed the distinctions between acupuncture and dry needling, let's take a look at which patients benefit from each approach and if there are any side effects, contraindications and considerations to be made...
References:
Audette, J. F., & Blinder, R. A. (2003). Acupuncture in the management of myofascial pain and headache. Current pain and headache reports, 7(5), 395-401.
Birch, S. (2003). Trigger point-acupuncture point correlations revisited. The Journal of Alternative & Complementary Medicine, 9(1), 91-103.
Birch, S., Hesselink, J. K., Jonkman, F. A., Hekker, T. A., & Bos, A. A. T. (2004). Clinical research on acupuncture: part 1. What have reviews of the efficacy and safety of acupuncture told us so far?. The Journal of Alternative and Complementary Medicine, 10(3), 468-480.
Bolton K and Selvaratnam PJ 2009. Myofascial trigger point treatment for headache and TMD. In: Selvaratnam PJ, Niere K and Zuluaga M. Headache Orofacial Pain and Bruxism. Diagnosis and multidisciplinary approaches to management. Churchill Livingstone, Elsevier, Edinburgh
Bogduk, N., (1989). Understanding pain pathways. Current Therapeutics, 30(1):25-40
Dommerholt, J., Mayoral del Moral, O., & Gröbli, C. (2006). Trigger point dry needling. Journal of Manual & Manipulative Therapy, 14(4), 70E-87E.
Dorsher, P. (2006). Trigger points and acupuncture points: anatomic and clinical correlations. Med Acupunct, 17(3), 21-25.
Gunn, C. C. (1997). Radiculopathic pain: diagnosis and treatment of segmental irritation or sensitization. Journal of Musculoskelatal Pain, 5(4), 119-134.
Han, J. S., & Terenius, L. (1982). Neurochemical basis of acupuncture analgesia. Annual review of pharmacology and toxicology, 22(1), 193-220.
Lianfang, H. E. (1987). Involvement of endogenous opioid peptides in acupuncture analgesia. Pain, 31(1), 99-121.
Hong, C. Z., & Simons, D. G. (1998). Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points. Archives of physical medicine and rehabilitation, 79(7), 863-872.
Huguenin L K 2004 Myofascial trigger points: the current evidence. Physical Therapy in Sport 5:2-12
Huguenin L F, Brukner, P, McCrory P R, SmithP, Wajeswelner, H, Bennell K L 2005 The effect of dry needling gluteal muscles on straight leg raise-a randomised, placebo controlled double-blind study. BJSM. 39, 84-90
Le Bars, D., Dickenson, A. H., & Besson, J. M. (1979). Diffuse noxious inhibitory controls (DNIC). II. Lack of effect on non-convergent neurones, supraspinal involvement and theoretical implications. Pain, 6(3), 305-327.
Le Bars, D., Dickenson, A. H., & Besson, J. M. (1982). Opiate analgesia and descending control systems. In: Bonica J J, Lindblom V, Iggo A (Eds) Advances in pain research and therapy. Raven Press, New York, Vol 5, 341-372
Lucas, K. R., Polus, B. I., & Rich, P. A. (2004). Latent myofascial trigger points: their effects on muscle activation and movement efficiency. Journal of Bodywork and Movement Therapies, 8(3), 160-166.
Lucas, 2007. The effects of latent myofascial trigger points on muscle activation patterns during scapular plane elevation. Ph.D Thesis. Australasian Digital Thesis Network.
Melzack, R., Stillwell, D. M. & Fox, E. J. (1977) Myofascial Trigger Points and Acupuncture Points for Pain: Correlation and Implications. Pain 3: 3-23
Niddam, D. M., Chan, R. C., Lee, S. H., Yeh, T. C., & Hsieh, J. C. (2008). Central representation of hyperalgesia from myofascial trigger point. Neuroimage, 39(3), 1299-1306.
Selvaratnam, P, J, Knight, K (1995) Acupuncture in sports physiotherapy applied science and practice. I: Zuluaga, M. (1995). Sports physiotherapy: applied science and practice. Churchill Livingstone.p. 289-294.
Selvaratnam P J 2004 Dry needling for acute and chronic pain - spinal and sports injuries. Seminar notes. Conducted by the Musculoskeletal Physiotherapy Association Australia, Australian Physiotherapy Association, Camberwell, Victoria, Australia
Selvaratnam P J 2008 Dry needling for Physiotherapists. Handbook of the Clinical Doctorate Physiotherapy programme in Dry Needling. School of Physiotherapy, The University of Melbourne, Parkville, Australia
Selvaratnam PJ and Gabel P. 2009 Dry needling, acupuncture and laser. In: Selvaratnam PJ, Niere K and Zuluaga M. Headache Orofacial Pain and Bruxism. Diagnosis and multidisciplinary approaches to management. Churchill Livingstone, Elsevier, Edinburgh
Shah, J. P., Danoff, J. V., Desai, M. J., Parikh, S., Nakamura, L. Y., Phillips, T. M., & Gerber, L. H. (2008). Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Archives of physical medicine and rehabilitation, 89(1), 16-23.
Simons, D. G., Hong, C. Z., & Simons, L. S. (2002). Endplate potentials are common to midfiber myofacial trigger points. American Journal of Physical Medicine & Rehabilitation, 81(3), 212-222.
Terenius, L. (1985). Families of opioid peptides and classes of opioid receptors. Advances in pain research and therapy, 9, 463-477.
Travel, J. G., Simons, D. G., & Simons, L. S. (1999a). Myofascial Pain and Dysfunction: The Trigger Point Manual-Upper Half of Body. Baltimore, Md: Wiliams & Wilkins.
Travell, J. G., Simons, D. G., & Simons, L. S. (1999b). Myofascial pain and dysfunction: the trigger point manual: Vol. 2: The lower extremities. Williams & Wilkins.