Explaining central sensitisation to patients
Introduction
In a previous blog on a 'mechanism-based classification for pain' I discussed the clinical presentation of nocicieptive pain, neuropathic pain and central sensitisation pain. As promised at the conclusion of that post, this blog will cover the mechanisms of central sensitisation in greater depth.
How many times have we heard someone say 'they say the pain is all in my head'? This statement has such negative connotations and often causes patients to become upset, angry, misunderstood and can even cause them to discontinue with treatment. It is a sticky statement, and once the patient grabs onto it, it can be so difficult to change.
Where did that statement come from?
This is a question that I'd love to know the answer to (but realise that this will take many more years of experience and reading the literature). But today I am going to make a start ... so this blog will aim to explaining what central sensitisation is, the neurophysiological processes involved, and provide an option for clinicians to educate patients more effectively to avoid sending them down the path of believing 'it's all in my head'.
Where does it all start?
My belief is that clinicians are mostly responsible (although it's never intentional) for developing the statement during the process of explaining the process of chronic pain. Either we choose the wrong words, or patients misunderstand the statements and we haven't checked their understanding of the message given?
Every treatment provided by a physiotherapist should be accompanied by sufficient patient education to gain informed consent. For cervical manipulation, dry needling, clinical pilates, we have a spiel explaining the purpose of treatment, why we've chosen it, what the benefits are and the risk involved. Pain education has to be one of the hardest treatments to explain, and even now I'm still working on my spiel. The words we choose to communicate this message can dictate the understanding and perceptions that our patients gain.
How does the literature describe central sensitisation?
The quotes below are taken from references I often refer back to (which explains in much greater detail the process of central sensitisation) when educating people about pain.
“This does not mean that the pain is not real, just that it is not activated by noxious stimuli” (Woolf, 2011, p. S4).
"Anything that is detectable or accessible to the brain and relevant to the evaluation of danger to body tissue has the capacity to modulate pain. All contributing factors should be considered in all pain states". (Mr Alastair James Flett, APAM, FACP, 2014).
But of course these statements cannot be used in isolation. They first require an explanation for the process of pain. I think this should include a diagrammatic explanation of how noxious stimulus travels through the nervous system, the points within the spinal cord and brain where that stimulus is mediated, reinforced, inhibited etc and how it is processed from the central nervous system. Then to explain that the outcome of the processing is a painful experience. From there I might go on to explain the changes which occur in the nervous system both peripherally and centrally during chronic pain. Lets look at that a little closer....
What is central sensitisation in Chronic pain?
After discovering the pain gating theory, researchers found that the peripheral terminals of nociceptors (neurones which detect noxious stimulus) can become sensitised and have a reduced threshold to heat stimuli, particularly after exposure to inflammatory modulators after acute tissue injury. This phenomenon became known as primary hyperalgesia (Woolf, 2011). Primary hyperalgesia cannot explain the clinical symptoms of pain summation, allodynia, or secondary hyperalgesia. It was speculated that these changes had to occur from alternations in the receptor fields within the central nervous system.
Central sensitisation is defined by the IASP (International Association for the Study of Pain, 2014) as "increased responsiveness of nociceptive neurones in the central nervous system to their normal or sub-threshold afferent input".
What is the pain mechanism responsible for central sensitisation pain?
- The primary mechanism for central sensitisation comes from the neuro-plastic changes which occur, which include:
- Activation of the limbic and paralimbic structures and increased activity of the prefrontal cortex.
- A previous blog explores the parts of the brain which are activated during pain processing, known as the pain neuromatrix.
- Structural changes in the brain associated with chronic pain experience.
- Increased synaptic efficacy making them more easily triggered.
- Increased neuro-modualtory cells and gene transcription - meaning our immune system has a direct impact on the maintenance of chronic pain.
- Increased receptor field size and density making a larger and more sensitive nervous system for detecting stimulus.
- Long term potentiation.
One aspects of central sensitisation that Woolf (2011) discusses is long term potentiation which occurs when a stimulus is applied but the output is sustained from the transmitter gates remaining open for a sustained period after the stimulus has stopped. We see this clinically with patients who do not require a huge stimulus to experience pain (hypersensitivity) and a prolonged experienced of pain (which makes the behaviour seem non-mechanical). This long term potentiation is an aspect of central sensitisation pain that I often forget to explain to patients. It helps them to understand that often a seemily insignificant stimulus can result in significant and prolonged pain.
Something else that can occur, which relates back to the role of the pain neuromatrix, is that the entire neural network within the CNS (a pain map as described in David Butler in Explain Pain) can be triggered by a small input. So again, what appears to be an insignificant stimulus or a stimulus that doesn’t result in serious tissue damage can result in a severe increase in pain and prolonged flare up. I’m sure we’ve all seen this clinically too.
(Woolf, 2011, p. S4)
What is the outcome of these neuroplastic changes?
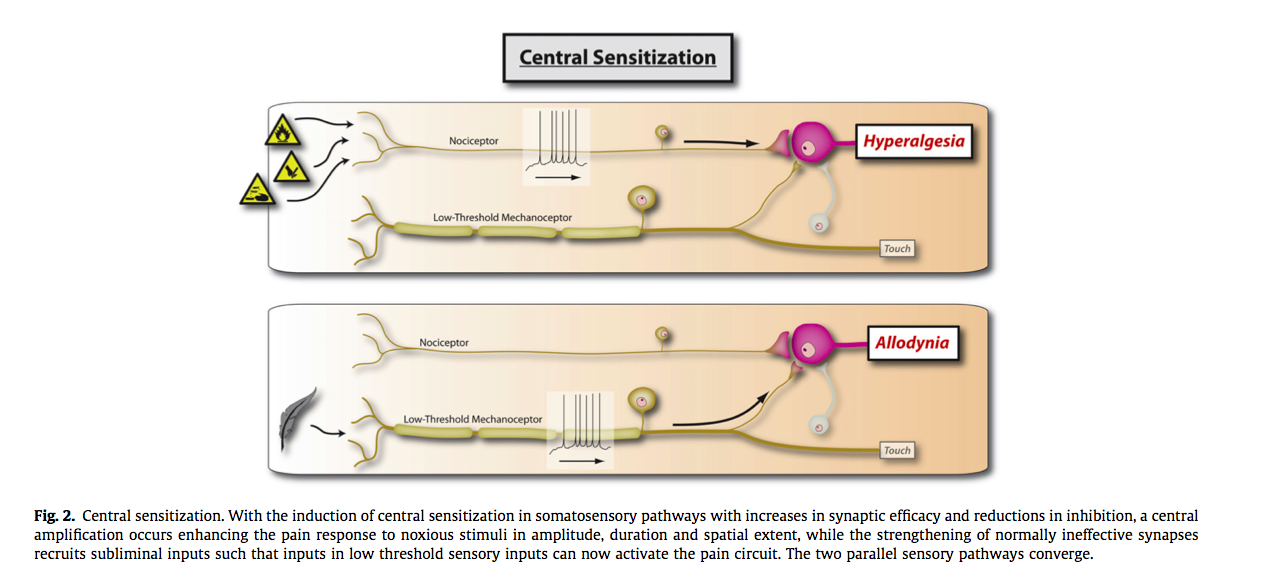
- Hyperalgesia - Increased pain from a stimulus that normally provokes pain (IASP, 2014).
- Wind up - when continuous C fibre stimulation results in increased action potential and therefore repeated stimulus results in increased pain intensity (Woolf, 2011).
- Allodynia - Pain due to a stimulus that does not normally produce pain (IASP, 2014).
From the delphi study conducted by Smart et al (2012), experienced clinicians noted that there were three cardinal symptoms and one sign indicative of this pain type.
- The strongest predictor was disproportionate, non-mechanical, unpredictable pattern of pain provocation in response to multiple/ non-specific aggravating/easing factors.
Pain disproportionate to the nature and extent of the injury or pathology.
Strong association with maladaptive psychosocial factors (e.g. negative emotions, poor self-efficacy, maladaptive beliefs and pain behaviours).
Diffuse/non-anatomic areas of pain/tenderness on palpation. (K. M. Smart, Blake, Staines, & Doody, 2012, p. 342)
What are the barriers to recovery?
Teaching and addressing CSP involves educating patients about the changes in pain science and evidence-based medicine and this requires "reconceptualisation of the problem" (Moseley, 2003c, p. 184).
Moseley (2003c) used the Neurophysiology of Pain Test to assess both the understanding of patients and professionals about pain, and to investigate if professionals accurately estimate their patient's ability to understand and learn about pain. The results were very interesting.
The main finding was that both professionals and patients have the capacity to understand the neurophysiology of pain. Two points were highlighted from this study:
- Health professionals with post graduate training in pain achieved ~85% accuracy on the survey, which was significantly higher than health professionals without pain-specific education (~65%). This supports the role of pain-science education across all health professional domains.
- That health professionals underestimate their patient's ability to learn, understand and reconceptualize chronic pain.
In summary, the health professionals understanding of the neurophysiology of pain and their education to patients is one of the primary barriers to patients reconceptualizing and understanding their problem of chronic pain.
So what do I say?
"We are going to take time during the course of your treatment to discuss your pain and the processes which occur in the body that have lead to where you are today. This is a conversation that may take some time to complete, and I'm happy to work through any questions that come up over the next few sessions. Lets make it an ongoing dialogue where you can give me any feedback and ask any questions about what I am going to teach you."
"For today, my goal is to teach you about the mechanisms of acute pain and how these are different to chronic pain. Pain is not an input, pain is an output from the brain. It starts with a noxious stimulus in the tissues which can be either thermal, chemical or mechanical, that travel through particular nerve fibres to the spinal cord. From there, these messages travel up the spinal cord to the brain, where a series of parts of the brain (known as the pain neuromatrix) receive and interpret the stimulus or input. Once it has been processed, the body has the ability to dampen or enhance these messages and the output back down to the body part, is what you feel, pain."
"However, when a noxious stimulus has been present for a prolonged period (over 12 weeks), changes start to occur within the peripheral and central nervous system. This is commonly referred to as central sensitisation pain or peripheral sensitisation pain. The reason being is that the nervous system, particularly the central nervous system, is plastic and susceptible to change. The changes we know that occur are increased receptor field size, reduced threshold for activation and enhanced activation of the neuromatrix. This is a process which you didn't choose or consciously drive, but what we do know is that it changes the pain you experience and can lead to amplification of your pain."
"This is where we need to break down what pain you experience and to try decipher what is related to actual or potential tissue damage, and what is a result of this sensitisation of your nervous system. Sometimes the best tool we have is to think about the nature of the pain and how it occurred. Acute pain caused by mechanical stimulus will behave in a mechanical (on/off or predictable way). Chronic pain is far less predictable and harder to measure in relation to input and often you can experience allodynia (when something which isn't painful feels painful), wind up (when a repeated stimulus becomes pain) and hypersensitivity (increased pain levels for a painful stimulus). Lets discuss now what parts of the central sensitisation process you present with and ways to address this problem."
"The most positive thing to remember is that plastic changes occurred to lead you to where you are today, and these plastic changes are equally as reversible if you can learn to understand the problem, reconceptualise how you interpret your pain/problem and how to pace you life and retrain and re-expose your body to regain the function you want."
Obviously I wouldn't say all of that in one session, but is a gist of how I choose to talk to patients. Each time there is improvement or a flare up come back to the explanation you've given your patient to help reinforce their learning.
And the most important thing to do.... is check exactly what they have understand by simply saying "If someone asked you what you learnt from your physiotherapist today, what would you tell them?"
These are all small steps in the direction of improving patient outcomes through improved understanding of pain education and communication. Good luck!
Sian
References
International Association for the Study of Pain. (http://www.iasp-pain.org/Taxonomy). Accessed January 9th, 2015.
Woolf, C. J. (2011). Central sensitization: implications for the diagnosis and treatment of pain. Pain, 152(3), S2-S15.