Cervical Motor Control Part 4 - Rehabilitation Principles
“The combined exercise and manual therapy approach is also superior to results found for manual therapy intervention alone” (O’Leary, Falla, Elliot & Jull., 2009., p. 331).
Neck pain complaints continue to rise and we need to become more proficient in managing these problems and preventing reoccurrences. As our knowledge of muscular impairments increases we are able to draw stronger conclusions about the optimal exercise prescriptions and progressions. Clinically, I feel that most Physiotherapists are aware of the cranio-cervical flexion test (CCFT) and the initial phases of rehabilitating the deep cervical neck flexors (DCNF). But, sadly, I also feel most patients are left with DNCF exercises in supine and never progressed out of this cognitive learning phase. The aim of this blog therefore is to discuss the three phases of rehabilitation, from cognitive learning, to integration with posture and functional movements, and finishing with strengthening and endurance training. The second aim is to provide information for these phases for both cervical flexor and extensor muscles in the hope of showing how a rehabilitation program can be designed and progressed.
“Similar to findings in low back pain, cervical muscle dysfunction does not appear to spontaneously recover following the alleviation of symptoms. A recent systematic review suggests that the combination of exercise and manual therapy are the most efficacious of all conservative managements for subacute or chronic mechanical neck pain” (O’Leary, Falla, Elliott & Jull., 2009., p.324).
One aspect of this quote that catches my attention is the first statement similar to findings in low back pain. It makes be wonder how many similarities we can draw between the lumbar and cervical spine? One of the reasons why I feel motor control for the cervical spine is so important is because structurally, biomechanically and functionally the cervical and lumbar spine are completely different. It is thought that 80% of the stability of the cervical spine is derived from the muscular system, giving further credit for its relevance in assessment and treatment. Muscular dysfunction results not only in pain and loss of movement or function, but also can lead to cervicogenic headache and somatosensory disturbances,
When it comes to rehabilitation there has traditionally been two approaches, one of general exercise and one of specific exercise. General exercise included walking for general health and a non-specific strength training program for the neck and shoulder muscles. The aim of these programs are to promote general health and gain an analgesic effect to alleviate pain, and restore strength and function (Schomacher & Falla., 2013, 363). The second approach to rehabilitation is that of a specific muscle retraining program and a major focus of this blog.
If you think back to the research highlighted in the first blog you'll remember that results have shown two different changes in muscle behaviour. The first is that there is reduced activation of the DCNF and increased activity of the superficial neck flexors. The second is that there is less strength and more fatiguability in neck flexors as a group (Falla., 2004). Therefore, when designing rehabilitation programs it could be hypothesised that a program that addresses both activation patterns and endurance will have a beneficial effect. When designing the rehab programs it is important that the dosage prescription reflects the roles of the muscles in terms of coordination, endurance, or fatigue (Edmondston, et al., 2011).
There are three phases of specific rehabilitation that can be viewed as a continuum for prescribing exercises (Jull, 2008, p. 208):
- Phase 1: focus on low-load precision to activate deep cervical and axioscapular muscles.
- Phase 2: continuation of muscle re-education by training the coordination of muscles during postural movements and functional tasks.
- Phase 3: address strength and endurance matching to the patient’s functional requirements.
Phase 1 of rehab - precision & low load exercises
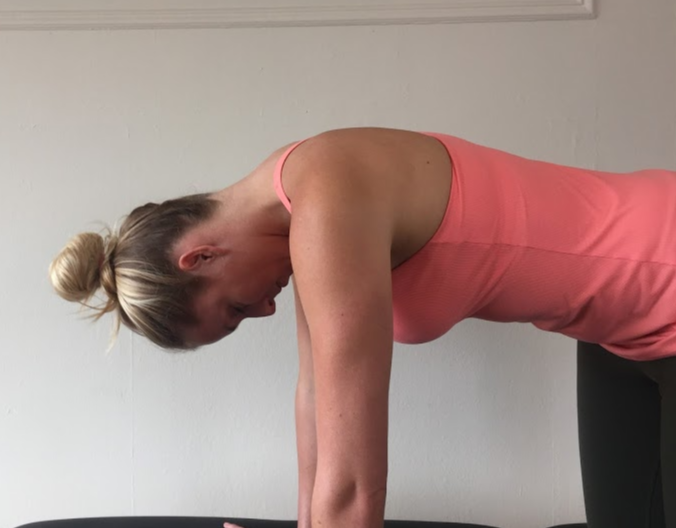
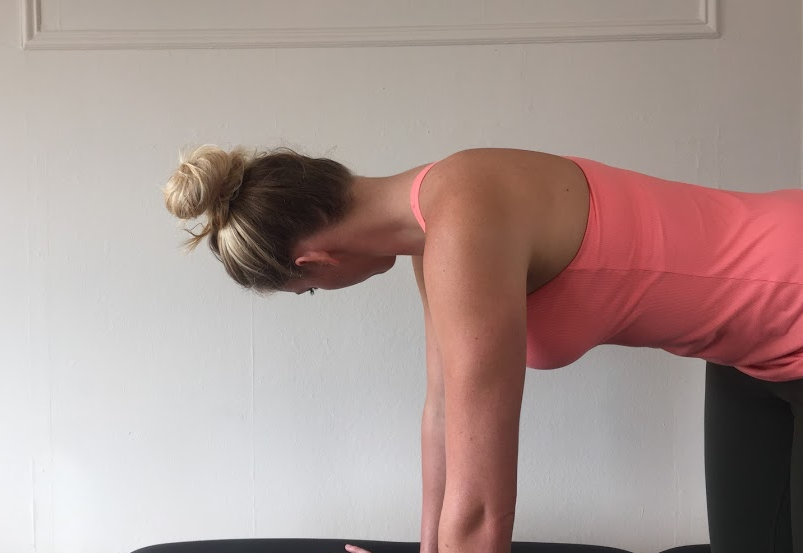
In this first stage the focus is on training deep cervical neck flexor control in supine, scapula setting in sitting and 4PK and deep neck extensor and suboccipital muscle activity in 4PK. The aim with each exercise is to achieve the correct pattern of movement without substitution from other muscle synergies and the starting positions are going to be the same as the assessment positions for each of the muscle groups.
Cervical flexion exercises:
Longus colli and longus capitus activation is trained in supine in the same position as the CCFT (Jull, 2008, p.209).
- DCNF need to be correctly activated to perform CCF in the correct manner.
- It is an activation movement and therefore should be performed slowly.
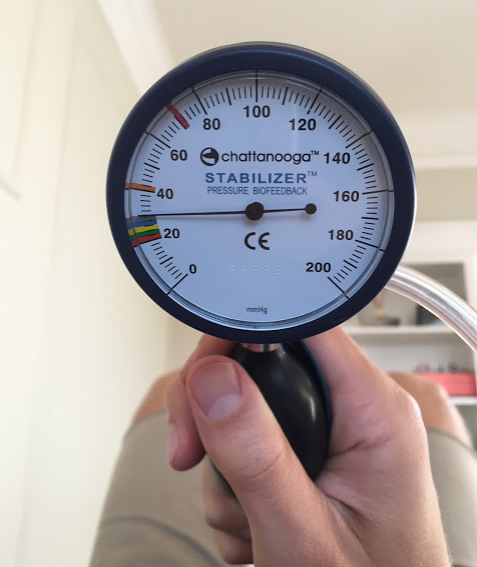
- It is better not to use the PBFU in this phase of training but to use other external feedback cues.
- Clinicians can help their patients by looking for compensation strategies such as: apical breathing, jaw clenching, retraction over CCF, not returning to neutral, overshooting past neutral, and activity in the SCM and AS.
- The aim is to perform the correct exercise 2-3 times a day and building up to 10 x 10 second holds.
- Over the course of 4-6 weeks the patient will develop technique and endurance for this exercise.
In 2009 Jull, Falla, Vincenzino & Hodges explored the difference between general exercise of head lifting strength and specific cranio-cervical flexion exercises and their impact on changes in the CCFT. The specific group practiced DCNF with PBFU for 6 weeks progressing from their initial level of control to 10 x 10 second holds at 30mmHg. The general strengthening group did weighted head lifting exercises progressing to 3 x 10 reps of 50% 10RPM then 75% 10RM then full RM. Initially the weight of the head was enough and as patients progressed more weight was added in 0.5kg increments. What this study suggested is that as SCM and AS activity decreases, DNCF strength improves and that DCNF exercises are the only exercises that change performance on the CCFT. You can look at these results from two perspectives. The first is that if we only perform DCNF in supine we only change our performance on the CCFT in supine. The second is that general head lifting strength as a role in changing endurance but may not change DNCF activity. Just something to keep in the back of your mind when you are choosing where to begin with your rehab program.
If you are going to prescribe DCNF in sitting to you clients the aim is still to build up to 10 seconds holds throughout the day and couple this with lumbo-pelvic upright sitting.
In 2012, Beer, Treleaven & Jull published a paper showing that performing the DCNF movement i.e. upper cervical flexion, in a position of lumbo-pelvic upright sitting results in similar improvements on the CCFT as desired from performing the exercises in supine (i.e. of reduced SCM and AS activity and improved coordinated CCF from the DCNFs). These subjects performed the exercise holding it for 10 seconds every 15-20 minutes during the day and the movement was described as gentle lift of the base of the skull from the top of the neck. I find this study very encouraging and it links nicely with what other studies have shown about ideal sitting posture and the impact it has on the cervical spine.
When we are retraining sitting posture simply using the cue to ‘sit up straight’ is not good enough. We need to teach our patients about lumbo-pelvic upright sitting if we want to reduce the loads on the cervical spine as well as education patients about ideal resting scapula posture (Jull, 2008). “Sitting postures are typically associated with levels of muscle activation of between 2 and 6 % maximum voluntary contraction with activity being present in the deep and superficial muscle” (Edmondston, et al., 2011, p.333). We also need to take into consideration the surface they are sitting on or work station they are sitting at, as discussed in the previous blog [INSERT LINK]
Cervical extension exercises:
To train DCNE we replicate the test environment. There are two main exercises which address each muscle group (Selvaratnum, 2009, p. 184; Jull, 2008, p. 212-213):
- Suboccipitals are trained with craniocervical rotation and craniocervical extension/flexion.
- Semispinalis cervicis and multifidis are trained with cervical extension while maintaining neutral craniocervical positions.
- Because there are more exercises to complete for this group the aim is to complete 5 repetitions of each of the three movements building up to 3 sets of 10.
- A further progression into sitting would involve the therapist applying a resistance at 10% MVC and the patient resisting the movement. This is a great exercise for moving into coordinated co-contractions at low level activity in a functional position.
- To progress between each stage of rehabilitation may be rapid (2-4 weeks) for some but may also take 6-8 weeks for others (Selvaratnum, 2009, p. 184).
One important note about phase 1 exercises for both the flexor and extensor group is that they can be commenced very early in rehabilitation and are often performed in a pain-free manner (O’Leary, Falla, Elliot & Jull., 2009., p. 330). Aside from not taking the time to perform these tests, there rarely is a reason why the exercises can't be commenced very early on. Don't leave it too late before you assess motor control and start retraining muscle function.
Some tips about 4PK neck extension exercises.
- Schomacher & Falla (2013, p.364) suggest that if the head is in a neutral position, extension movements activate the superficial muscles below C2 but, if in 15 degrees craniocervical extension it will promote more semispinalis cervicis activity.
- These authors also suggest that applying a ventral/cranial pressure to the C2 arch while the patient pushing into extension further increases semispinalis cervicis activity.
- This is the only reference where I read about these fine changes to the movement of training cervical extension but they may be worthwhile exploring with your patient if you’re having difficultly isolating the deeper cervical extensor muscles.
Phase 2 of rehab - retraining coordination and posture
The role of endurance training.
Training cervical flexion endurance with a sustained head lift & hold.
Falla (2004) discuss how research has demonstrated greater fatigability in SCM and AS between 25-50% maximal voluntary contraction in patients with neck pain. This suggests that addressing fatigability during rehabilitation is an important focus. You may be wondering why I am now talking about SCM and AS when our initial goal was to reduce their activity and promote DCNF? Well, we have to progress our rehabilitation to incorporate strengthening of the global muscles as they work synergistically with the local stabilisers. This is an important component of treatment progression.
Cervical flexion endurance capacity is trained with a head lifting task but the emphasis is placed on maintaining craniocervical flexion (Selvaratnum, 2009, p. 187; Jull, 2008, p. 205). But remember that before we get to head lifting endurance, cervical flexor endurance can be commenced early in training but increasing the holds of CCF in supine. In this case the PBFU is helpful to train the patient in their endurance. Before they can begin training their endurance in this position they need to have built their strength up to 28-30mmHg on the CCFT. From there, the aim is to build up to 10 x 10 second holds 2 x day but before you achieve this, technique must be perfect.
If you are aiming to train cervical extension endurance you can position the patient in sitting. From here they look slowly into full extension and return making sure that the DCNFs are controlling CCF not SCM. Once this movement is pain free the patient can progress to looking into extension. At the end of range the patient rests their head on the hand of the therapist. From a completely relaxed position the patient initiates a head lift using CCF and holds the weight of their head for 5 seconds before returning to upright. This is repeated 5 times (Jull, 2008, p. 219-220).
As mentioned above, it you want to train flexors and extensor coordination then isometric contractions in sitting are a good place to start. From there you want to move into patterns of cervical and scapula movement. The exercises at this point are based purely on the rehabilitation goals of your patient.
Another option for training coordination and endurance is rhythmic stabilisation beginning with alternating isometric contractions (especially in rotation) and then moving to resistance through range. Start slowly and at around 10% MVC and build your way from there.
To try help demonstrate a difference in programs we are going to offer a variety of exercises that would be used for an office worker compared to a painter and a rugby player.
Phase 3 of rehab - high load & functional training
By this point I hope you are realising that neck rehabilitation extends much further than DCNF in supine. To build strength and endurance we need to introduce theraband resisted exercises which are completed in a functional position for that of the patient.
As an example though, a 2006 study investigated the efficacy of physiotherapy treatments for cervicogenic headaches (Ettekoven & Lucas). Their exercises consisted of postural correction with CCF into the resistance of a blue theraband. The exercise was performed twice a day for about 10 minute sessions over the course of 6 weeks and then twice a week for 6 months. At the six month follow up the treatment group had significant reductions in headache frequency, intensity and duration. This trial demonstrates that using a theraband immediately in treatment i.e going straight to phase three but performing the exercises consistently, has a positive impact on cervicogenic headaches.
At this stage of rehabilitation the exercises are specifically designed for the functional requirements of the patient and their professional/athletic movement patterns. Many of the papers I've read don't expand in this area as it is hard to give advice in a hypothetical sense. For this blog however, we just wanted to give some indication of exercises might look like for three different patient types; the office working, the painter and the rugby player.
THE OFFICE WORKER
Of the three examples provided here, the office worker is the easiest to imagine as it involves sitting education, cervical extension endurance training and scapula positioning in low levels of elevation. Depending on the style of work completed by your patient, rotational control to one side might also be required.
THE PAINTER
Painting involves sustained overhead and repetitive tasks that require excellent scapula stability and the ability to withstand long periods of cervical extension. It can be suggested therefore that cervical extensor endurance and scapular stability above 90 degrees flexion or abduction would be two focussed on this phase of treatment. What you can see from these pictures is that the first theraband is being used to strengthen cervical extension and the second is creating a depression and anterior tilting force, for which the patient as to correct to achieve scapula upward rotation, posterior tilt and elevation.
THE RUGBY PLAYER
Alicia is deeply involved in rugby as a Physiotherapist and has taken some pictures of the exercises she uses with her athletes. Rugby is a great sporting example where cervical motor control is paramount to being able to control tackles and the scrum.
summary
“The challenge for clinicians is to optimize the training of muscles to best address the patient’s key functional deficits” (O’Leary, Falla, Elliott & Jull., 2009, p.329).
So remember:
- You can’t progress if you don’t monitor change.
- You need to develop a function-orientated approach which is specific and meaningful to the patient.
- Training begins early in rehabilitation and is often painfree even if the patient is stiff recovering from their pain and loss of movement.
- Addressing the axioscapular muscles is also very important to consider based on the patient’s problem.
- Progression between levels depends purely on your patient and how quickly they progress.
- Progression into the final stages of rehabilitation requires a thorough understanding of the functional requirements of the patient and some creativity.
- Stages of training lie on a continuum.
We can say with confidence that muscular impairments in both cervical extensor and flexors are associated with neck pain, and that these impairments are complicated. To assess these motor control deficits takes time and I hope you now see the importance for making such time. Clinically we should persist and continue prescribing rehab protocols on a treat what you find basis until we more clearly understand the physiological mechanisms as to how each exercise works.
Sian & Alicia :)
References:
Beer, A., Treleaven, J., & Jull, G. (2012). Can a functional postural exercise improve performance in the cranio-cervical flexion test? –A preliminary study. Manual therapy, 17(3), 219-224.
Caneiro, J. P., O'Sullivan, P., Burnett, A., Barach, A., O'Neil, D., Tveit, O., & Olafsdottir, K. (2010). The influence of different sitting postures on head/neck posture and muscle activity. Manual therapy, 15(1), 54-60.
Cleland, J. (2005). Orthopaedic clinical examination: an evidence-based approach for physical therapists. WB Saunders Co.
Edmondston, S., Björnsdóttir, G., Pálsson, T., Solgård, H., Ussing, K., & Allison, G. (2011). Endurance and fatigue characteristics of the neck flexor and extensor muscles during isometric tests in patients with postural neck pain. Manual Therapy, 16(4), 332-338.
Falla, D. (2004). Unravelling the complexity of muscle impairment in chronic neck pain. Manual therapy, 9(3), 125-133.
Falla, D., Bilenkij, G., & Jull, G. (2004). Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine, 29(13), 1436-1440.
Falla, D., Jull, G., O’leary, S., & Dall’Alba, P. (2006). Further evaluation of an EMG technique for assessment of the deep cervical flexor muscles. Journal of Electromyography and Kinesiology, 16(6), 621-628.
Jull, G. (2008). Whiplash, headache, and neck pain: research-based directions for physical therapies. Elsevier Health Sciences.
Jull, G. A., O'Leary, S. P., & Falla, D. L. (2008). Clinical assessment of the deep cervical flexor muscles: the craniocervical flexion test. Journal of manipulative and physiological therapeutics, 31(7), 525-533.
O'Leary, S., Falla, D., Elliott, J. M., & Jull, G. (2009). Muscle dysfunction in cervical spine pain: implications for assessment and management. journal of orthopaedic & sports physical therapy, 39(5), 324-333.
O’Leary, S., Falla, D., & Jull, G. (2011). The relationship between superficial muscle activity during the cranio-cervical flexion test and clinical features in patients with chronic neck pain. Manual therapy, 16(5), 452-455.
Schomacher, J., & Falla, D. (2013). Function and structure of the deep cervical extensor muscles in patients with neck pain. Manual therapy, 18(5), 360-366.
SELVARATNAM, Peter, et al. Headache, orofacial pain and bruxism. 2009.
Szeto, G. P., Straker, L., & Raine, S. (2002). A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Applied ergonomics, 33(1), 75-84.
VAN ETTEKOVEN, H.; LUCAS, C. Efficacy of physiotherapy including a craniocervical training programme for tension‐type headache; a randomized clinical trial. Cephalalgia, 2006, vol. 26, no 8, p. 983-991.