Chain reaction - the neurophysiological mechanism of manual therapy
Introduction
"Regardless of how rationalised, the biomechanical model for passive movement has always suffered from the fact that positive outcomes may sometimes be obtained by treatment applied “elsewhere”. This is highly suggestive of a “neurological” rather than mechanical effect. Namely, facilitation of movement through (endogenous) inhibition of pain. This observation, together with the above and other evidence has led Wellens to conclude that where pain is the major problem to be “treated” the biomechanical model for passive movement “appears largely erroneous”; and where this is presumed to be “abnormal” mobility it is doubtful that passive movement can achieve any lasting physical “change”. (All of which begs the question: what is responsible for any observed positive effect?)." (Zusman, 2011, p. 645)
The above quote is taken from one of Zusman's more recent publications The Modernisation of Manipulative Therapy, in which the author discusses the current philosophy surrounding the positive effects of manual therapy, the limitations of a purely biomechanical model, and suggests areas for improved education and teaching of physiotherapists. I have always enjoyed reading Zusman's papers, as he provides a curious and inquisitive insight about my profession and a well-developed and well-educated opinion about pain science - a topic that continues to fascinate me.
Manual therapy techniques are a treatment modality used daily by many therapists and yet we don't completely understand the entirety of it's effect and how positive results are achieved. This blog aims to explore the ideas which have evolved around the neurophysiological effects of manual therapy. It should be noted from the beginning that the information presented is in no way concrete and research around this topic continues, as the methods of objectively quantifying the effects on the peripheral and central nervous system also continue to expand.
To my readers, I ask you to answer these questions before you continue:
What does manual therapy do?
How does it work?
How do you describe these effects to other clinicians and patients?
When performing a treatment technique, what is the purpose/goal and how are you actually achieving this?
Manual therapy
Mobilisation and manipulation are passive treatment techniques frequently applied by therapists for the treatment of painful or stiff conditions. These techniques along with soft tissue biased and neural biased techniques form the range of manual therapy treatment options available to therapists.
Why is it important to understand the neurophysiology effects of manual therapy? Because we are interested in the elements that determine success of treatment: to ensure that the most appropriate treatment modality is selected for the problem and client, and to enhance the therapist' ability to identify those suitable and likely to respond favourably to treatment.
Most often, when manual therapy techniques fail to help a patient it is because the technique was not selected and executed appropriately, the patient was inappropriately identified, or the condition was not responsive to treatment. (Bialosky et al, 2009; Maitland, 2005).
What is your reasoning and understanding around what the treatment is achieving and the mechanisms behind the response received?
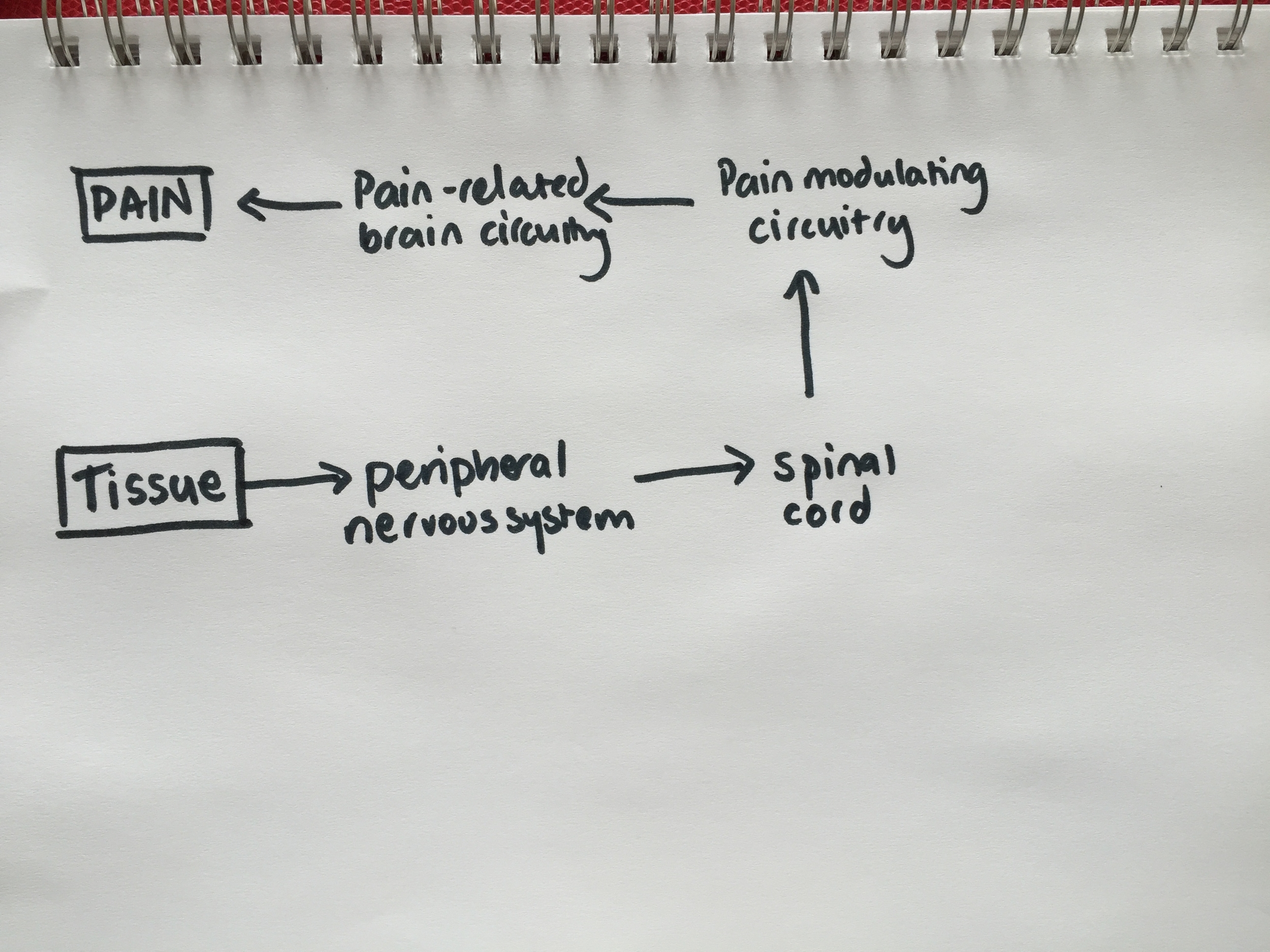
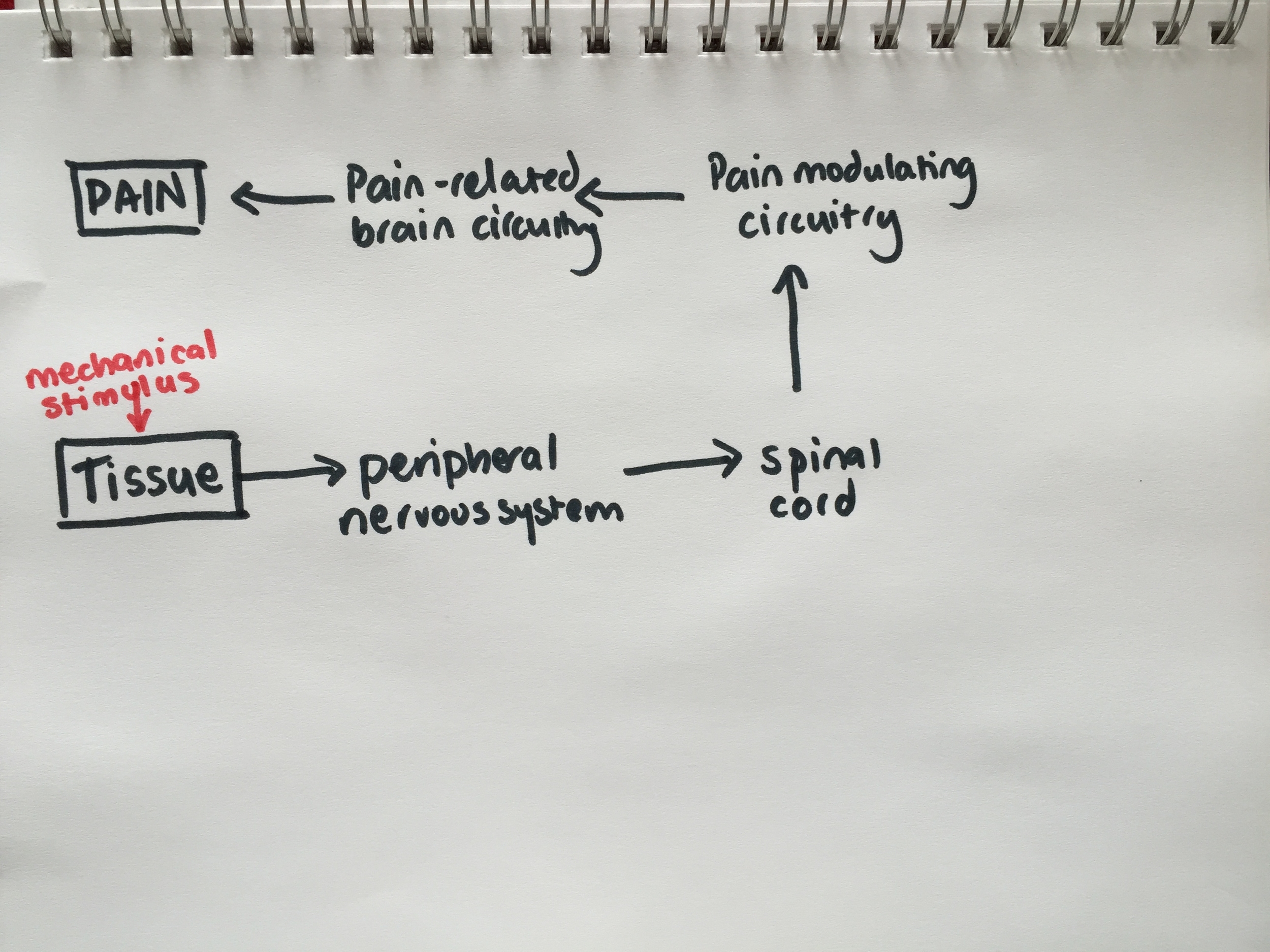
Model of the neurophysiological mechanism of manual therapy (Bialosky, et al., 2009, p. 533)
The diagram above is a schematic representation of the neurophysiological effects of mechanical stimulation. The model was published by Bialosky and collegues in 2009 - a paper well worth reading to further your knowledge. It's very detailed and incorporates many of the research areas on this topic.
The reason I’m referring to the work of Bialosky & colleagues (2009) is because their paper presents a proposed model explaining the neurophysiological effects of mechanical stimulation such as that found in manual therapy techniques. How often do patients ask “What is this treatment doing? How did you do that?” What do you say?
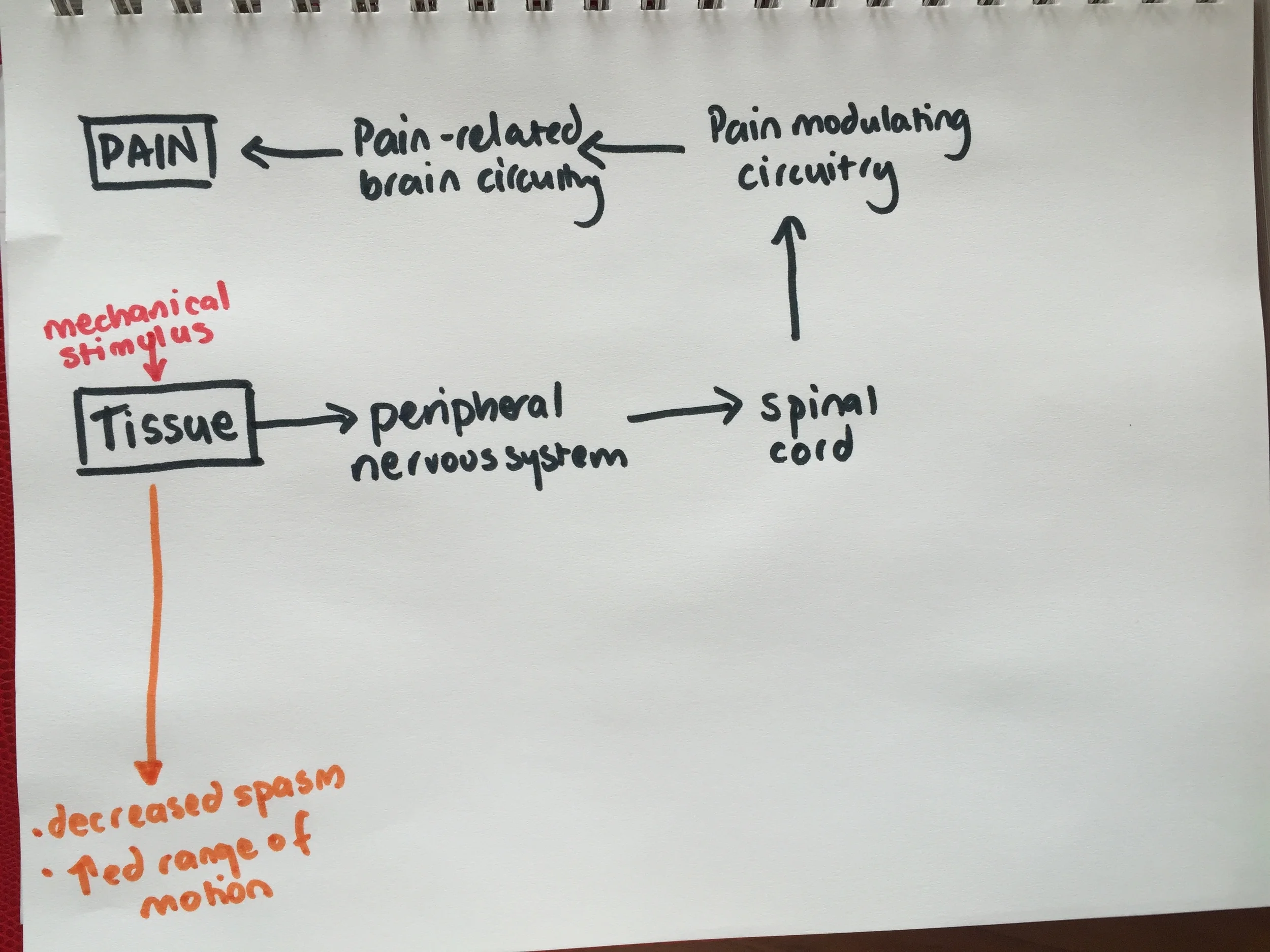
To ensure I was understanding the steps in this diagram, I drew it stage by stage. Let's take a look at each step.... follow the colours as I write out each step of the process from mechanical stimulation to pain output, or hopefully after treatment, reduction in pain output!
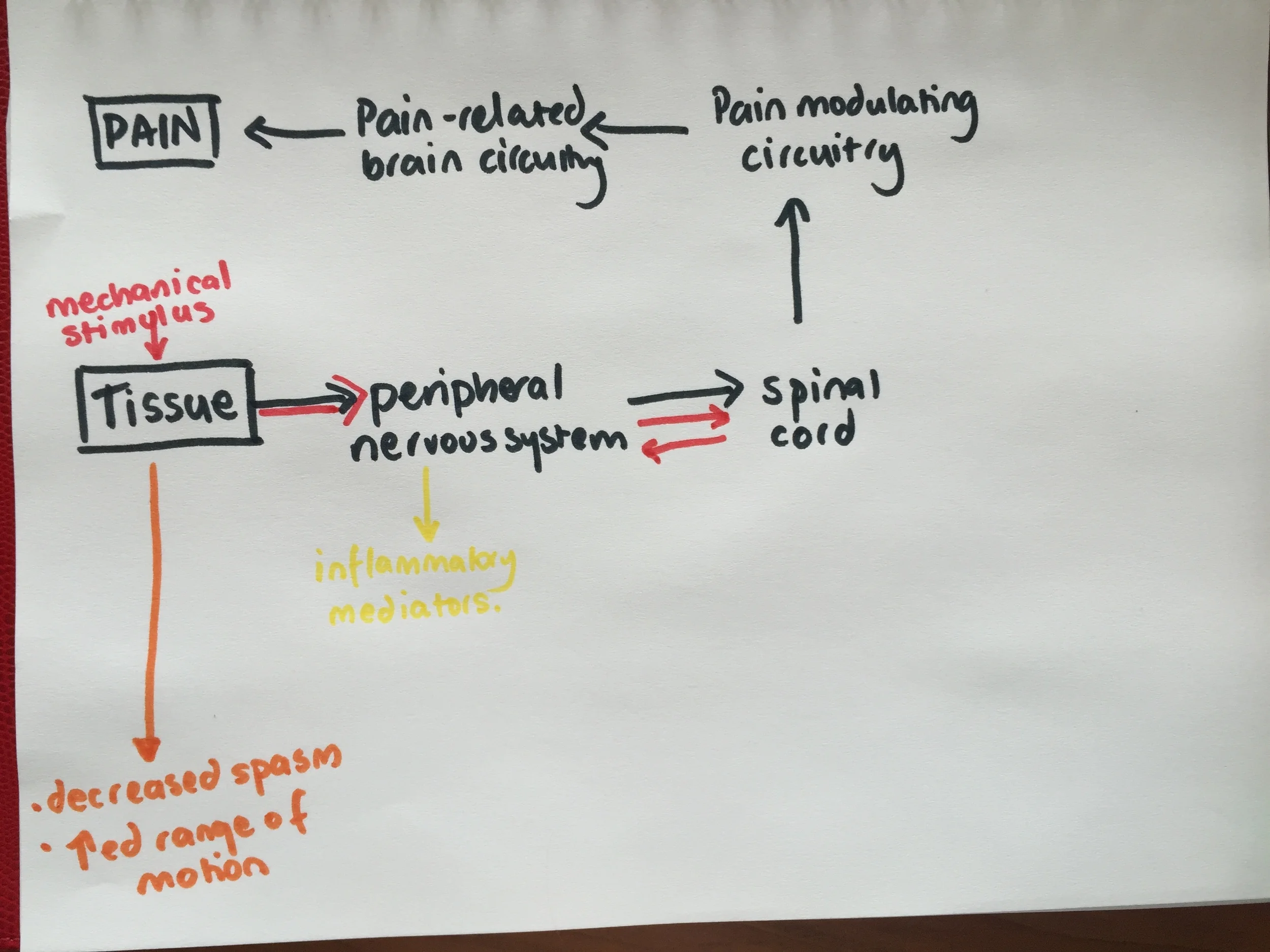
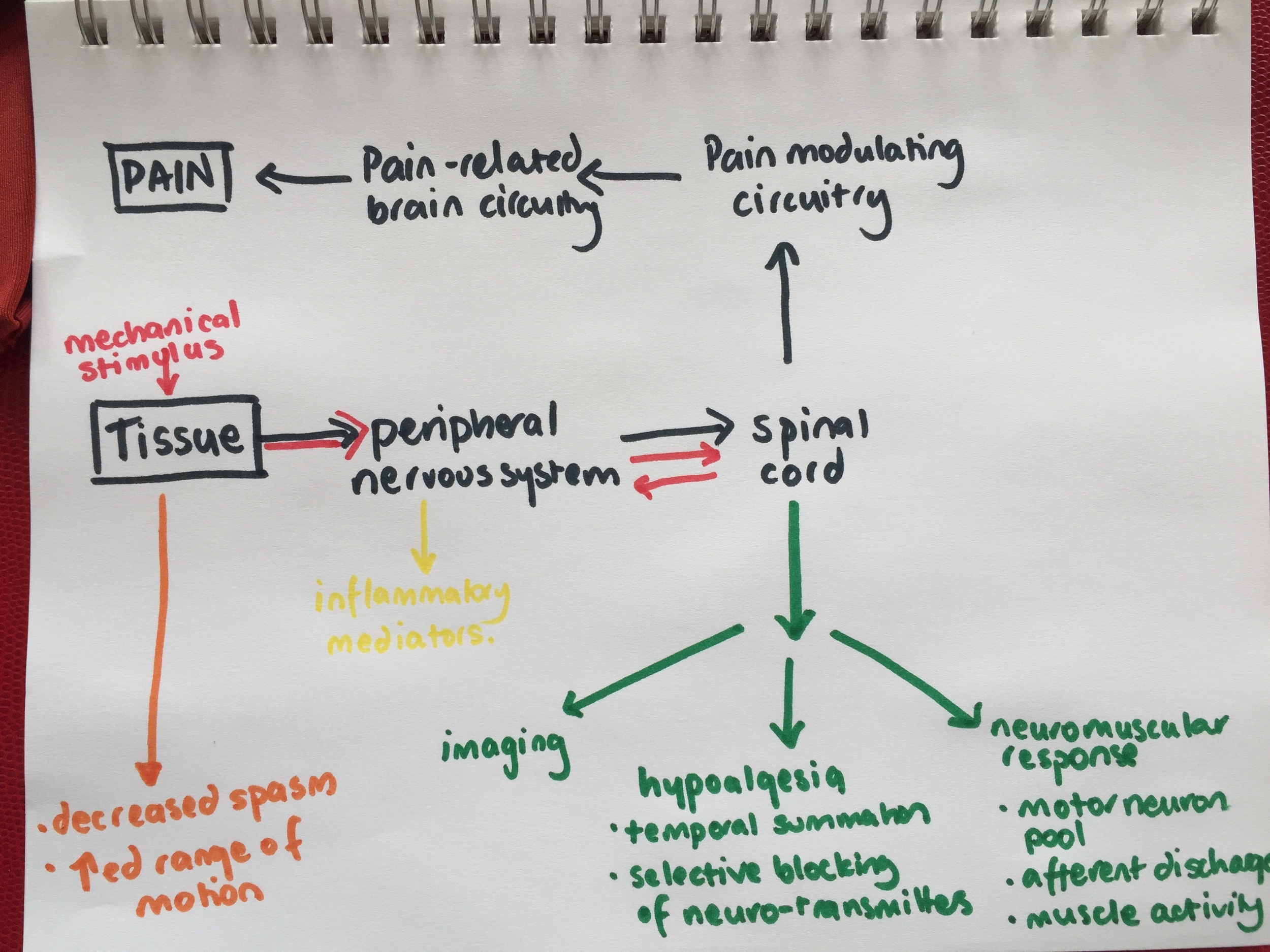
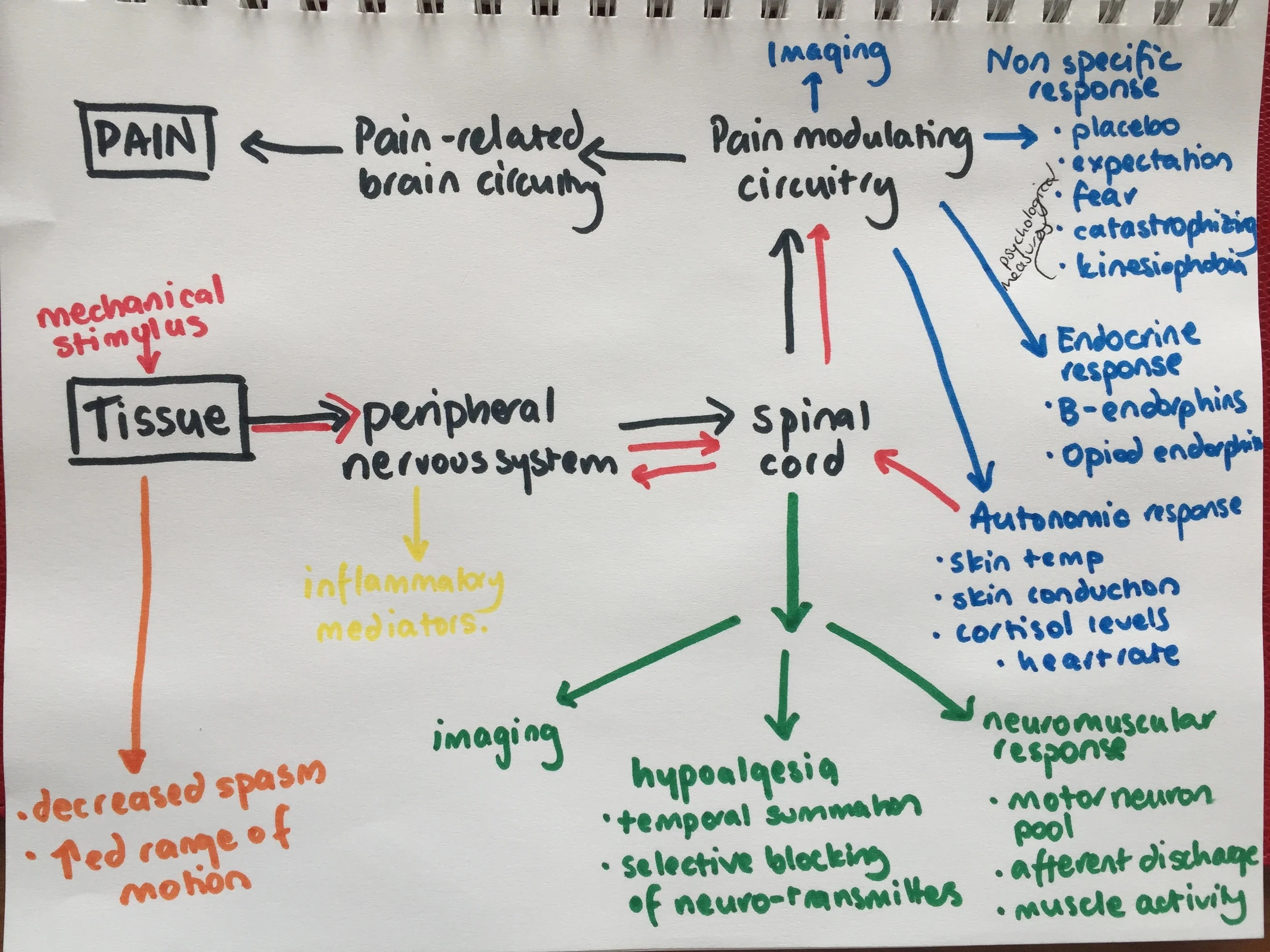
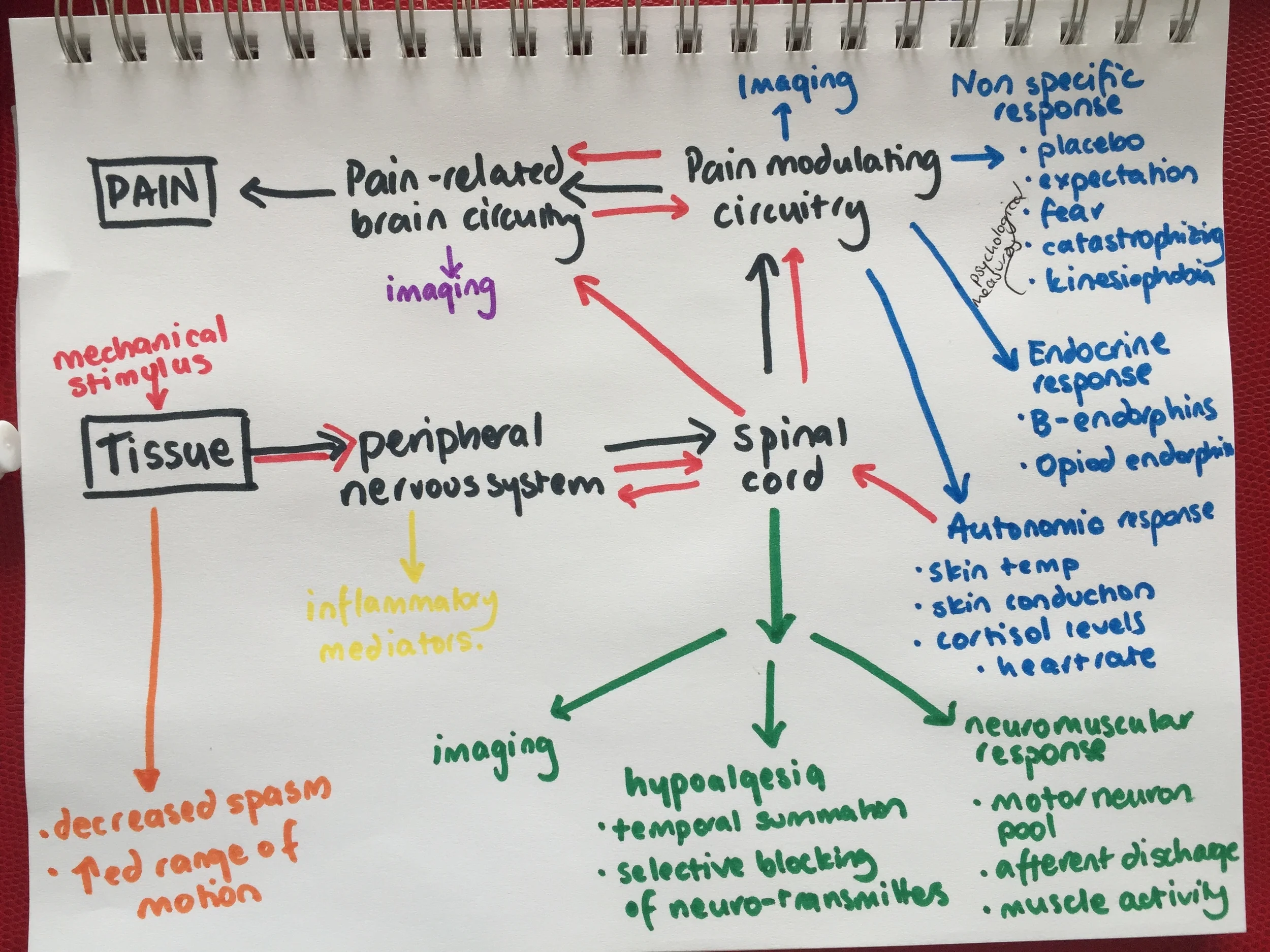
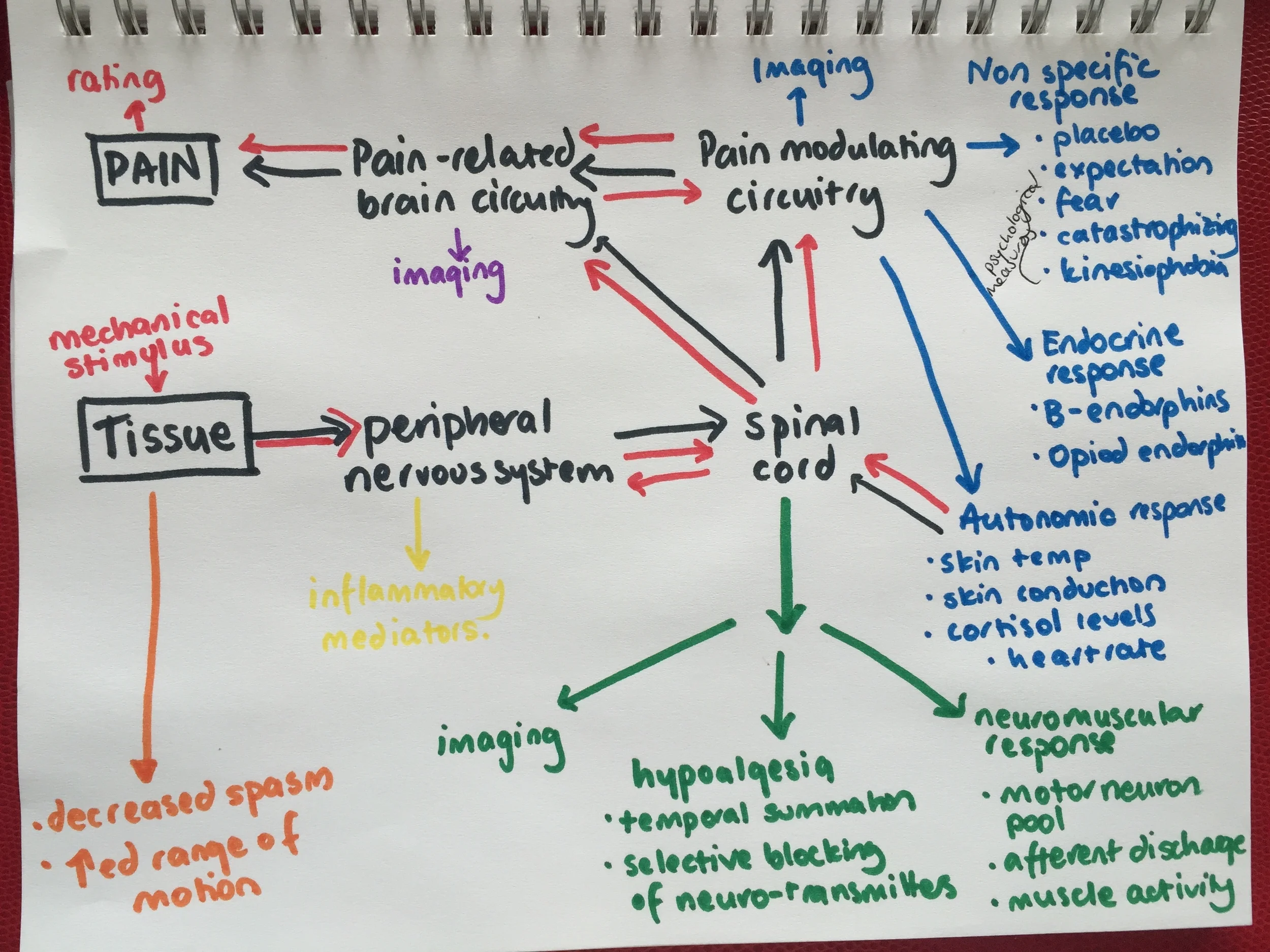
Having looked through the images you will see many mechanisms which work together as a chain reaction of neurophysiological events in the processing of mechanical stimulation. One of the questions Zusman alludes to in the first paragraph of this blog is Are there only mechanical effects of mechanical stimulation? It is clear now that there are both mechanical and neural mechanisms at play.
The Bialosky et al (2009) model provides a summary of current literature on this topic and puts the results of many studies into a single framework. This allows the reader to understand the context of the literature and knowledge in this field in a visual framework. It should be noted that this model can be applied to treatment outside of manual therapy but only the neurophysiological effects, not the biomechanical effects (Bialosky, et al., 2009. p. 535).
Mechanical mechanism
There are transient biomechanics changes in position and posture which occur after treatment, but no lasting change. That is why patients return for further treatment and the previously gained in-session changes have been lost.
There is a lack of strong reliability in treatment effectiveness because every practitioner performed techniques differently and no treatment technique is specific to a single structure i.e muscular, articular, neural structures cannot be isolated with techniques, only biased. Therefore, the mechanical effects of manual therapy will vary greatly among practitioners.
Mechanically there are changes in range of movement, EMG activity and muscle spasm, which can be used to objectively identify the effect of mechanical stimulation.
But does this model explain referred pain? Looking beyond the mechanical mechanisms....
Peripheral mechanisms - Here we are referring to the inflammatory response within tissues in response to tissue damage and healing.
Spinal mechanisms
This includes the Gate control theory established by Melzack & Wall in 1965 involving selective blocking of neuro-transmitters and temporal summation.
There is a neuromuscular response which leads to altered neurone activity, afferent discharge and muscle activity.
Supraspinal mechanisms
The processes occurring in the pain-modulating circuitry leading to muscle response changes and endogenous activation.
Endocrine activity including b-endorphine and opiod endorphine release.
Sympathetic response noted in skin conduction, cortisol levels, heart rate, respiratory rate and skin temperature.
Non-specific responses involving the affective response to stimulus - placebo effect, expectation, fear, catastrophisation, kinesiophobia etc.
Then there are processes occuring in the pain-related brain circuitry aka pain neuromatrix involving the anterior cingulate cortex, amygdala, periaquaductal gray, rostral ventromedial medulla.
The outcome of this chain reaction in response to manual therapy is often a reduction in pain but hopefully what this shows us, is how complicated the process is to achieve this outcome. And this doesn't even include aspects of treatment choice and execution. Many factors are at play which determine the success of treatment.
A brief look at history
Let’s take a step back in time…. although Bialosky and colleagues have compiled all this research into a single flowchart, it's important to know a bit of the history of where these ideas came from.
In 1965 Melzack & Wall proposed the Gate Control Theory, meaning that this model has been under construction for the past 50 years!
Around 1995-1998 the Gate Control Theory was incorporated into a Bio-psycho-social model of pain and disability. The gate control theory was expanded and so did our understanding of pain mechanisms, from which evolved a mechanism-based reasoning of pain. No longer was pain or afferent stimulation thought just to occur in the local tissues. Questions were arising...
“Just how there is an ‘after discharge’ in damaged axons which is chemically induced through injury, that causes the lingering and spreading of pain, may be a prolonged effect of mechanical stimulation of tissues following treatments” (Zusman, 1994, p. 36). In this quote Zusman is referring to the latent/prolonged pain associated with neuropathic pain compared to nociceptive pain. “Dorsal root ganglia, found in the peripheral NS, are naturally mechanically sensitive and often involved in peripheral neuropathic symptoms”. (p. 36).
Although these ideas are revolving around the mechanisms of neuropathic pain, they reinforce that for many years now physiotherapists have known that the mechanical stimulation applied in manual therapy techniques has much more than just an isolated effect mechanically on local tissues.
In 1994 Zusman said “The reason for symptomatic relief produced as a result of these mechanical movements are not known for certain. Neurologically this appears to involve inhibitions in the CNS” (p. 38). True to all his publications, Zusman is always provoking readers and researchers to continue questioning the mechanisms of pain and to explore unanswered aspects of pain science.
In 2008 Schmid, Brunner, Wright and Bachmann published a systematic review appraising the research papers evaluating the neurophysiological effects of passive joint mobilisation. One of their findings specifically related to this topic was “… passive joint mobilisation might also activate various areas within the central nervous system to produce a multisystem response that extends beyond the specific joints and spinal segments stimulated” (Schmid et al, 2008, p. 387-388). Again reinforcing this idea of a full system involvement in the processing of afferent input.
How does this model apply to clinical practice?
"Until recently, experts believed that the interplay of local and segmental responses to the mobilisation was responsible for a clinical benefit. The concept includes activation of gate-control mechanisms (Melzack and Wall, 1965; Wyke, 1985), hysteresis effects leading to a reduced neural afferent discharge (Zusman, 1986) and biomechanical effects such as tissue lubrication or ‘‘correction of spinal joint subluxation’’ (Paris, 1979).” (Schmid et al, 2008, p. 387).
Beside the importance of needing to be able to justify our treatment modalities through scientific knowledge, knowing about these neurophysiological mechanisms is required to more thoroughly understand what research exists about the efficacy of manual therapy for various musculoskeletal conditions. The main question I kept asking while reading these articles was "how do you measure these effects on the peripheral and central nervous system clinically?" And if it is hard to measure, how do they design randomised controlled trials to evaluate these effects?
Objective measures that do exist:
Pain related measures: VAS, Pain pressure threshold, thermal pain threshold, painfree grip strength, painfree range of motion tests. (Schmid et al, 2008)
Sympathetic nervous system indicators: Skin conductance, blood pressure, heart rate, respiration rate.
Inflammatory markers: funnily I didn't find much on the objective measures of inflammation but I'm assuming it refers to aching, swelling, pain, and blood flow.
Motor Function measures: painfree grip strength, EMG activity, global function.
Which conditions have systematic reviews supporting the use of manual therapy as treatment will be a discussion for a later post. Next I hope to outline the neurophysiological mechanisms of mobilisation compared to manipulation specifically in studies that investigate the effects on the spine.
In summary, the main learning points from this blog is that there is ongoing research into the neurophysiological mechanisms which occur in response to mechanical stimulation (manual therapy). Although this research has found no conclusive answer, the model published by Bialosky provides a good representation of each component thought to be involved. In the topic of pain science, there has been extensive research about different pain states and conditions and parallels can be drawn between this model and pain conditions. From my understanding there is considerable overlap in the pathway used to process mechanical stimulation and nociceptive stimulation.
Hopefully these images and this discussion has equipped you with the knowledge to answer these questions with a deeper understanding of the complexity of the processes involved.
What does manual therapy do?
How does it work?
How do you describe these effects to other clinicians and patients?
When performing a treatment technique, what is the purpose/goal and how are you actually achieving this?
Sian
References
Bialosky, J. E., Bishop, M. D., Price, D. D., Robinson, M. E., & George, S. Z. (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Manual therapy, 14(5), 531-538.
Melzack, R. (1999). From the gate to the neuromatrix. Pain, 82, S121-S126.
Melzack, R., & Wall, P. D. (1967). Pain mechanisms: a new theory. Survey of Anesthesiology, 11(2), 89-90.
Schmid, A., Brunner, F., Wright, A., & Bachmann, L. M. (2008). Paradigm shift in manual therapy? Evidence for a central nervous system component in the response to passive
Smart, K., & Doody, C. (2006). Mechanisms-based clinical reasoning of pain by experienced musculoskeletal physiotherapists. Physiotherapy, 92(3), 171-178.
Zusman, M. (1994). The meaning of mechanically produced responses.Australian Journal of Physiotherapy, 40(1), 35-39.
Zusman, M. (2011). The modernisation of manipulative therapy.

